Abstract
Background
Gastric fundus invagination (GFI) is a novel weight loss procedure. The gastric fundus is invaginated inside the gastric lumen and anastomosed to the gastric antrum. In gastric plication (GP), the greater curvature is plicated inside the gastric lumen leaving a narrow gastric channel for food passage. This study compares GFI to GP in a diet-induced obesity rat model.
Methods
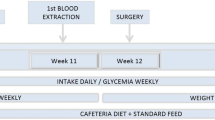
Twenty Long-Evans male rats were fed a 60 % high fat diet for 6 weeks. At 14 weeks of age, the rats underwent either GFI (N = 10) or GP (N = 10) surgery. Body weight and food intake were measured for 6 weeks. Serum adipokines and ghrelin hormone were assayed. Six weeks after surgery, all rats were euthanized and the stomachs examined. The two-sample t test was used to compare the results between the two groups.
Results
All GFI rats had an intact fundus invagination at 6 weeks following surgery. The greater curvature plication unfurled in three out of ten GP rats. Part of the fundus herniated through the plication suture line in one GP rat. There was no significant difference between the mean percent weight change for the GFI (4.2 ± 4.1 %) and GP (8.8 ± 6.0 %) groups. There was no difference in food intake between both groups. GFI was associated with a significant lower fasting ghrelin levels (101.1 ± 13.1 versus 137.3 ± 27.4; p = 0.044) compared with GP.
Conclusions
GFI offers a more effective and more durable surgical alternative for weight loss than GP.






Similar content being viewed by others
References
Mason EE. Development and future of gastroplasties for morbid obesity. Arch Surg. 2003;138:361–6.
Tretbar LL, Taylor TL, Sifers EC. Weight reduction. Gastric plication for morbid obesity. J Kans Med Soc. 1976;77(11):488–90.
Brethauer SA, Harris JL, Kroh M, et al. Laparoscopic gastric plication for treatment of severe obesity. Surg Obes Relat Dis. 2011;7:15–22.
Spiegelman BM, Flier JS. Obesity and the regulation of energy balance. Cell. 2001;104:531–43.
Sumithran P, Prendergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365:1597–604.
Scott WR, Batterham RL. Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: understanding weight loss and improvements in type 2 diabetes after bariatric surgery. Am J Physiol Regul Integr Comp Physiol. 2011;301:R15–27.
Valderas JP, Irribarra V, Rubio L, et al. Effects of sleeve gastrectomy and medical treatment for obesity on glucagon-like peptide 1 levels and glucose homeostasis in non-diabetic subjects. Obes Surg. 2011;21:902–9.
Lindeboom MY, Vu MK, Ringers J, et al. Function of the proximal stomach after partial versus complete laparoscopic fundoplication. Am J Gastroenterol. 2003;98:284–90.
Longo KA, Charoenthongtrakul S, Giuliana DJ, et al. Improved insulin sensitivity and metabolic flexibility in ghrelin receptor knockout mice. Regul Pept. 2008;150(1–3):55–61.
Cummings DE, Weigle DS, Frayo RS, et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Eng J Med. 2002;346(21):1623–30.
Dimitriadis E, Daskalakis M, Kampa M, et al. Alterations in gut hormones after laparoscopic sleeve gastrectomy: a prospective clinical laboratory investigational study. Ann Surg. 2013;257(4):647–54.
Shen D, Ye H, Wang Y, et al. Comparison of short-term outcomes between laparoscopic greater curvature plication and laparoscopic sleeve gastrectomy. Surg Endosc. 2013;27:2768–74.
Fusco PE, Poggetti RS, Younes RN, et al. Evaluation of gastric greater curvature invagination for weight loss in rats. Obes Surg. 2006;16:172–7.
Fusco PE, Poggetti RS, Younes RN, et al. Comparison of anterior gastric wall and greater gastric curvature invaginations for weight loss in rats. Obes Surg. 2007;17:1340–5.
Menchaca HJ, Harris TL, Thompson SE, et al. Gastric plication: a pre-clinical study of the durability of serosa-to-serosa apposition. Surg Obes Relat Dis. 2011;7(1):8–14.
Guimaraes M, Nora M, Ferreira T, et al. Sleeve gastrectomy and gastric plication in the rat result in weight loss with different endocrine profiles. Obes Surg. 2013;23:710–7.
Talebpour M, Amoli BS. Laparoscopic total gastric vertical plication in morbid obesity. J Laparoendosc Adv Surg Tech A. 2007;17(16):793–8.
Conflict of Interest
None of the authors have a conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Darido, E., Moore, J.R. Comparison of Gastric Fundus Invagination and Gastric Greater Curvature Plication for Weight Loss in a Rat Model of Diet-Induced Obesity. OBES SURG 24, 897–902 (2014). https://doi.org/10.1007/s11695-014-1181-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1181-6