Abstract
The aim of this work was to form NiTi and TiNiCo body temperature activated and superelastic staples for clinical joining of mandible and face bone fractures. The alloys were obtained by VIM technique. Hot and cold processing was applied to obtain wires of required diameters. The martensitic transformation was studied by DSC, XRD, and TEM. The shape memory effects were measured by a bend and free recovery ASTM F2082-06 test. The superelasticity was recorded in the tension stress-strain and by the three-point bending cycles in an instrument equipped with a Hottinger force transducer and LVDT. Excellent superelastic behavior of TiNiCo wires was obtained after cold working and annealing at 400-500 °C. The body temperature activated shape memory staples were applied for fixation of mandibular condyle fractures. In experiments on the skull models, fixation of the facial fractures by using shape memory and superelastic staples were compared. The superelastic staples were used in osteosynthesis of zygomatico-maxillo-orbital fractures.
Similar content being viewed by others
Introduction
NiTi shape memory alloys with a chemical composition consistent with ASTM F2063-05 have been approved as metal biomaterials and are used in production of medical implants and devices (Ref 1-3). Products of NiTi alloys exhibiting phenomena of shape memory and superelasticity are widespread in such applications as orthodontic archwires, staples for osteosynthesis, stents, endodontic and surgical instruments (Ref 4-6). These implants show good mechanical properties, high corrosion resistance, and biocompatibility (Ref 7, 8). It is well known that improvement of shape memory and superelastic properties can be achieved by ternary additions and thermal or thermomechanical treatments (Ref 9-12). The NiTi staples applied to internal osteosynthesis in orthopedics and maxillofacial surgery operate usually as the shape memory staples activated by patient body heat (Ref 13, 14). For fixation of craniofacial bone fractures, the NiTi staples that are superelastic at the room temperature can also be used (Ref 15).
The studied NiTi-based implants were prepared at the Institute of Materials Science at the University of Silesia. They were applied to osteosynthesis of craniofacial bone fractures in the clinical experiments carried out by Department of Cranio-Maxillofacial Surgery of Medical University of Silesia in Katowice. Staples made of Ti50Ni48.7Co1.3 obtained agreement of the Bioethical Commission to be used for fixation of mandible bone fractures and were applied in 1990-1995 in clinical applications (Ref 16). Positive results of experiments carried out first for animals and then in human body applications showed that the NiTiCo implants as small staples may be used, for example, for fixation of mandibular condyle fractures or osteosynthesis of zygomatico-maxillo-orbital fractures.
Recently, it was confirmed that the NiTi alloys with Co additions in the range of 1-2 at.% should be considered for future medical applications (Ref 17).
The aim of these studies was to form NiTi and TiNiCo body temperature activated and superelastic staples for clinical joining of mandible and face bone fractures.
Materials and Experiments
In the experiments two types of alloys were used: commercial NiTi Euroflex wires (Ti-50.8 at.% Ni) with diameters of 1 to 1.4 mm and wires made of TiNiCo alloys of our own production by vacuum induction melting. The melted ingots were homogenized at 900 °C for 48 h under vacuum of about 10−5 Torr and followed pack hot rolled on the shape mill at 900-800 °C to rods with diameters of about 4 mm. After removing surface oxides, the rods were rotary forged to about 2 mm diameters and subsequently hot or cold drawn in sintered carbides wire drawing dies to wires with various diameters.
Samples of the wires 70 mm long and of different diameters were polished, washed in distillated water, scoured in acetone, and then subjected to proper heat treatment. They were solution treated at 700 °C for 15 min, cooled down in iced water, and then annealed at the temperature range of 300-500 °C for 15, 30, and 60 min. The cold worked wires with total deformation of 20-50% were annealed in the range of 300-600 °C in air atmosphere. Short annealing times from 5 to 15 min were used. Colored oxide layers were removed by chemical etching in water solution of HF and HNO3.
X-ray phase analysis was carried out using Philips X’Pert diffractometer with graphite monochromator on the diffracted beam. Cu Kα1 radiation was used. Phase transformation courses were studied by the DSC-7 Perkin Elmer calorimeter in the temperature range −100 to +80 °C. Cooling and heating speed was 10°/min. Shape recovery was studied for the wires deformed at low temperature (in martensite state) by bend-free recovery according to ASTM F 2082-06 test (Ref 18). The superelasticity and shape memory properties were measured in the elongation tests using Instron 4469 machine and in cyclic three-point bending tests using self-constructed machine. Compression forces of the staples were measured using digital FG-5000A gage.
Results and Discussion
X-ray phase analysis of the NiTi wires annealed at 700 °C for 15 min followed by cooling in iced water showed that despite applying argon atmosphere during annealing the wire surfaces were slightly oxidized. Weak diffraction lines for TiO2 were observed (Fig. 1a). The oxide layer was totally removed after chemical etching in water solution of HF and HNO3. The diffraction patterns showed the B2-phase lines only (Fig. 1b).
Superelastic properties of NiTi wires recorded at room temperature by tension tests indicated that there existed long plateau up to 8% deformation (Fig. 2). Superelastic properties of these wires in the three-point bending tests were confirmed (Fig. 3). On all recorded force-deformation plots, the plateau of forces during loading and unloading were observed.
In the as-received wires no transformation effects were observed in the DSC curves, the heat effects appeared for wires annealed in the temperature range 400-600 °C (Fig. 4).
In the specimen annealed at 400 °C one distinguished peak was observed at about 40 °C on cooling and two wide, hardly separated peaks could be seen on heating between 10-40 °C. This proves that the transformation course is B2 ⇔ R ⇔ B19′.
Similarly, two stage transformations were observed for specimens annealed at 500 °C. Increasing the annealing temperature causes that the transformation occurs directly from the B2 to B19′ martensite phases. It is worth to mention that for the specimen annealed at 400 °C the characteristic temperatures are higher than for the wires annealed at 500 and 600 °C. This can be explained by interaction of recovery and precipitation of the Ni4Ti3 phase processes.
Shape recovery measurements carried out according to the ASTM F 2082-06 standard showed that the as-received wires recovered at too low temperatures, i.e., A f ~ −20 °C (Fig. 5a). Implants working at the body temperature require much higher recovery temperature. This was obtained by annealing the samples for 0.5 h at 400-600 °C for which the recovery occurred at about 40 °C (Fig. 5b).
XRD analysis proved that also the NiTiCo alloys were in the B2-phase at room temperature (Ref 19). Cold drawing followed by annealing caused that on the X-ray diffraction patterns splitting of the 110B2 reflection appeared. This means that the R-phase occurred in the specimens (Ref 20, 21). This was confirmed by TEM studies (Fig. 6).
This is typical for the alloys deformed and then annealed with specific dislocation structure (Ref 22). The recovery process causes the dislocation cellular structure, i.e., in the specimen two regions can be distinguished: with low dislocation density—inside the cells; and high dislocation density—in the cell boundaries. The transformation occurs in these two regions at different temperatures.
Also the DSC curves for the specimens annealed after cold drawing show multi-stage character of the transformation (Fig. 7). For specimen annealed at 500 °C two distinguished, well-separated peaks of the R-phase and then B19′ transformations were observed. Annealing at lower temperature caused also that both transformations occurred each in two stages.
The shape recovery curves of the TiNiCo hot drawn wires, solution treated from 750 °C and additionally aged at 400 °C for 1 h show that recovery occurred at about 50 °C (Fig. 8). This is too high for implants activated by human body temperature. These wires can be used as implants activated by outer heat source (e.g., warm physiological salt).
Good temperature of shape recovery was obtained for the cold drawn wire of Ti50Ni48.7Co1.3 annealed at 400 °C for 15 min (Fig. 9). These wires were used to prepare staples for fixation of broken bones, activated by human body temperature, 37 °C.
In the wires of similar chemical composition subjected to high deformation followed by annealing good superelasticity was obtained (Fig. 10).
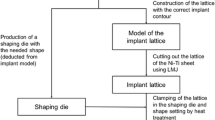
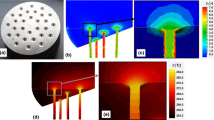
These alloys were used to prepare staples that could be easily inserted in the bone holes by mechanical bending their legs (Fig. 11). The staples for fixation of bone fractures were formed under the flame of gas burner by bending their ends up using the pliers for forming the wires. From wires with diameter 1.3, 1.2, and 1.1 mm the staples with the length of the span between 7 and 15 mm were formed.
Measurements of compression force of superelastic staples were recorded by using digital force gage (Fig. 12). The staples were opened at room temperature up to 90° angle between the legs and the span.
The compression forces of NiTi staples versus the deflection angle are shown in Fig. 13. The forces of prepared superelastic NiTi and TiNiCo staples in dependence of length of span, diameters of wires, and angles of legs were comprised in a range from several to about 30 N.
Recently in the Department of Skull and Maxillofacial Surgery of Silesian Medical University in Katowice carries out research on the development in implementation of a new method of subcondylar mandible fracture fixation by means of NiTi shape memory staples.
In the laboratory test it appeared that if the fixation is made by a single staple (Fig. 14a), the broken mandibular condyle may slip (Fig. 14b). It has been shown that better stability of the fixation of mandibular condyle fracture is secured by two parallel shape memory staples (Fig. 14c). After analysis by using the finite element method, for stabilization of subcondylar fractures, two shape memory staples were used in each case (Ref 23).
The use of NiTi superelastic staples for joining of zygomatic and Le Fort I face bone fractures is demonstrated on the model of the cranium (Fig. 15a, b).
Prepared NiTi shape memory staples with desired dimensions and properties after their laboratory studies were selected and applied for fixation of low subcondylar fractures of mandible of patients with multiple condyle mandible fracture (Ref 24). The superelastic staples were used for joining of zygomatic bone fracture.
An example of joining of multiple condyle fracture by using a body heat-activated NiTi staples and postoperative radiogram which proves an anatomical position of joined bone fragments in shown in Fig. 16.
Conclusions
-
NiTi staples which recover the desired shape under the influence of the human body heat can be prepared from the studied wires after cold drawing and annealing in the temperature range from 400 to 500 °C for 15-30 min.
-
After cold drawing with 40-50% deformation and annealing at 400 °C for 30 min very good superelastic properties of TiNiCo wires were obtained.
-
Staples from the wire of a small diameter can be used for fixation of bone fractures as superelastic staples which may be mechanically opened at a room temperature with a pincer and inserted into the drilled bone holes. Those staples we proposed for fixation of face bone fractures, for example: for fixation of zygomatic bone fracture or the Le Fort I face bone fracture.
-
The use of shape memory and superelastic staples instead of titanium plates and screws is easier and shortens the operation time.
References
T. Yoneyama and S. Miyazaki, Ed., Shape Memory Alloys for Biomedical Applications, Woodhead Publishing Limited, CRC Press LLC, Cambridge, 2009
S.M. Russell, Design Considerations for Nitinol Bone Staples, J. Mater. Eng. Perform., 2009, 18, p 831–835
M.H. Wu, Fabrication of Nitinol Materials and Components, Proceedings of the International Conference on Shape Memory and Superelastic Technologies, Kuming, China, 2001, p 285–292
A.R. Pelton, D. Stockel, and T.W. Duerig, Medical Uses of Nitinol, Mater. Sci. Forum, 2000, 327–328, p 63–70
L.G. Machado and M.A. Savi, Medical Applications of Shape Memory Alloys, Braz. J. Med. Biol. Res., 2003, 36, p 683–691
D. Tarnita, D.N. Tarnita, N. Bizdoaca, I. Mindrila, and M. Vasilescu, Properties and Medical Application of Shape Memory Alloys, Rom. J. Morphol. Embryol., 2009, 50(1), p 15–21
S.A. Shabalovskaya, Surface Corrosion and Biocompatibiity Aspects of Nitinol as an Implant Material, Biomed. Mater. Eng., 2002, 12, p 69–109
M. Es-Souni, M. Es-Souni, and H. Fischer-Brandies, Assessing the Biocompatibility of NiTi Shape Memory Alloys Used for Medical Application, Anal. Bioanal. Chem., 2005, 381, p 557–567
A.R. Pelton, J. DiCello, and S. Miyazaki, Optimization of Processing and Properties of Medical Grade Nitinol Wire, Min. Invas. Ther. Allied Technol., 2000, 9(1), p 107–118
M.C. Carroll, Ch Somsen, and G. Eggeler, Multiple-step Martensitic Transformations in Ni-Rich NiTi Memory Alloys, Scripta Mater., 2004, 50, p 187–192
P. Filip, J. Lausmma, J. Musialek, and K. Mazanec, Structure and Surface of NiTi Human Implants, Biomaterials, 2001, 22, p 2131–2138
D. Favier, Y. Liu, L. Orgeas, A. Sandel, L. Debove, and P. Comte-Gaz, Influence of Thermomechanical Processing on the Superelastic Properties of a Ni-Rich Nitinol Shape Memory Alloy, Mater. Sci. Eng., A, 2006, 429, p 130–136
J. Musialek, P. Filip, and J. Nieslanik, Titanium-Nickel Shape Memory Clamps in Small Bone Surgery, Arch. Orthop. Trauma Surg., 1998, 117, p 341–344
Z. Laster, A.D. MacBean, P.R. Ayliffe, and L.C. Nawlands, Fixation of a Frontozygomatic Fracture with a Shape-Memory Staple, Brit. J. Oral Maxillofac. Surg., 2001, 39, p 324–325
Z. Lekston, M. Jędrusik-Pawłowska, T. Cieślik, and J. Drugacz, Superelastic NiTi Staples for Fixation of Face Bone Fractures, Eng. Biomater., 2009, XII(89–91), p 42–46
J. Drugacz, Z. Lekston, H. Morawiec, and K. Januszewski, Use of TiNiCo Shape Memory Clamps in the Surgical Treatment of Mandibular Fractures, J. Oral Maxillofac. Surg., 1995, 53, p 665–701
A. Fasching, D. Norwich, T. Geiser, and G.W. Paul, An Evaluation of a NiTiCo Alloy and Its Suitability for Medical Device Applications, J. Mater. Eng. Perform., 2011, 20, p 641–645
ASTM F2082-06, Standard Test Method for Determination Temperature of Nickel-Titanium Shape Memory Alloys by Bend and Free Recovery, Annual Book of Standards, ASTM International, Philadelphia, PA, 2006, p 1–7.
Z. Lekston and E. Łągiewka, X-ray Diffraction Studies of NiTi Shape Memory Alloys, Arch. Mater. Sci. Eng., 2007, 28(11), p 665–672
V.E. Naish, T.V. Novoselova, I.V. Sagaradze, and Z. Lekston, Theoretical and Experimental Study of the R Phase Structure in Ti50Ni48.7Co1.3 Alloy, Mater. Sci. Forum, 2000, 321–324, p 710–715
Z. Lekston, D. Stróż, and M. Jędrusik-Pawłowska, Structure and Properties of Cold-Worked and Annealed Ti-Ni-Co Shape Memory Wires Designed for Medical Application, Solid State Phenom., 2010, 163, p 118–122
D. Chrobak and D. Stróż, Two-Stage R Phase Transformation in a Cold-Rolled and Annealed Ti50.6at.%Ni Alloy, Scripta Mater., 2005, 52, p 757–760
M. Kromka-Szydek, M. Jędrusik-Pawłowska, G. Milewski, Z. Lekston, T. Cieślik, and J. Drugacz, Numerical Analysis of Displacements of Mandible Bone Parts Using Various Elements for Fixation of Subcondylar Fractures, Acta Bioeng. Biomech., 2010, 12(1), p 12–18
M. Jędrusik-Pawłowska, Z. Lekston, M. Kromka-Szydek, J. Drugacz, and T. Cieślik, NiTi Shape Memory Staples as a Novel Surgical Fixation Method for Condylar Process Fractures, Eng. Biomater., 2008, 11(77–80), p 70–72
Acknowledgments
The work was financially supported by the Polish Ministry of Education and Science within the frame of the project Nr N N507 296339.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is an invited paper selected from presentations at the International Conference on Shape Memory and Superelastic Technologies 2011, held November 6-9, 2011, in Hong Kong, China, and has been expanded from the original presentation.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lekston, Z., Stróż, D. & Jędrusik-Pawłowska, M. Preparation and Characterization of Nitinol Bone Staples for Cranio-Maxillofacial Surgery. J. of Materi Eng and Perform 21, 2650–2656 (2012). https://doi.org/10.1007/s11665-012-0372-3
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11665-012-0372-3