Abstract
Introduction
Epidural analgesia has demonstrated superiority over conventional analgesia in controlling pain following open colorectal resections. Controversy exists regarding cost-effectiveness and postoperative outcomes.
Methods
The Nationwide Inpatient Sample (2002–2010) was retrospectively reviewed for elective open colorectal surgeries performed for benign and malignant conditions with or without the use of epidural analgesia. Multivariate regression analysis was used to compare outcomes between epidural and conventional analgesia.
Results
A total 888,135 patients underwent open colorectal resections. Epidural analgesia was only used in 39,345 (4.4 %) cases. Epidurals were more likely to be used in teaching hospitals and rectal cancer cases. On multivariate analysis, in colonic cases, epidural analgesia lowered hospital charges by US$4,450 (p < 0.001) but was associated with longer length of stay by 0.16 day (p < 0.05) and a higher incidence of ileus (OR = 1.17; p < 0.01). In rectal cases, epidural analgesia was again associated with lower hospital charges by US$4,340 (p < 0.001) but had no effect on ileus and length of stay. The remaining outcomes such as mortality, respiratory failure, pneumonia, anastomotic leak, urinary tract infection, and retention were unaffected by the use of epidurals.
Conclusion
Epidural analgesia in open colorectal surgery is safe but does not add major clinical benefits over conventional analgesia. It appears however to lower hospital charges.
Similar content being viewed by others
Introduction
Epidural analgesia (EA) has been utilized in abdominal surgery for over 40 years and several reports have already demonstrated its superiority over other forms of analgesia in terms of pain control.1,2
However, the effects of epidural analgesia on several postoperative outcomes have been the subject of debate. Because of its sympatholytic effect on spinal reflex mechanism,3 its anti-inflammatory activity, and its potential to reduce postsurgical stress response,4,5 epidural analgesia in open colorectal surgery has been suggested to shorten postoperative ileus,3,4 increase the blood flow to the intestine thereby contributing to the healing of intestinal anastomosis,6 reduce the incidence of major complications,5 and reduce 30-day mortality.7 Moreover, because of its superior pain control, EA may be associated with lower incidences of pulmonary complications.8
The controversy in previous reports stems from the significant heterogeneity in the study populations as the effect of epidural analgesia has been analyzed in patients undergoing thoracic and upper and lower abdominal surgery without controlling for this heterogeneity.8 Moreover, because of the increased adoption of laparoscopic techniques in colorectal surgery,9 recent reports have been focusing on the outcomes of EA following laparoscopic resections. As such, most of the studies that specifically examined the outcomes of EA in open colorectal surgery are now either outdated or limited by small sample sizes. In addition, many of these published series come from tertiary care centers which have specialized teams in the placement and management of epidural catheters.
Despite the recent increase in the use of laparoscopic techniques, 57 % of colorectal resections are still performed through an open approach.9 There are currently no reports evaluating the use and outcomes of epidural analgesia in open colorectal resections at the national level in different hospital settings and disease states.
Our aim was to retrospectively review the use of epidural analgesia in elective open colorectal resections in the USA and examine its short-term outcomes compared to conventional analgesia (CA).
Methods
Patient Population
The Healthcare Cost and Utilization Project-Nationwide Inpatient Sample (NIS) database was retrospectively analyzed for elective open colon and rectal resections performed with or without the use of EA from 2002 to 2010. The NIS is the largest all-payer inpatient care database in the USA and contains information from nearly eight million hospital stays each year across the country. Data elements within the NIS are drawn from hospital discharge abstracts that allow determination of all procedures performed during a given hospitalization as well as outcomes, charges, and length of stay.10 Approval for the use of the NIS patient-level data in this study was obtained from the institutional review board of the University of California–Irvine Medical Center and the NIS.
Inclusion Criteria
All patients with an ICD-9 CM diagnosis code of benign colon polyps (211.3, 230.3, V12.72), colon cancer (153.0–153.9), rectal benign polyps (211.4, 230.4, 230.5, 569.0), rectal cancer (154.0–154.2, 154.8), and diverticular disease (562.10–562.13) who underwent elective open surgery were included in our analysis. Cases that underwent epidural catheter placement were identified by the ICD-9 CM procedure codes 03.90 and 03.91 and were counted in the EA group. All other cases were considered in the CA group. The following colorectal procedures were included in our analysis: right and left hemicolectomy, transverse colectomy, sigmoidectomy, anterior resection, and abdominoperineal resection (APR).
Exclusion Criteria
Urgent and emergent cases as well as laparoscopic and converted cases were excluded from our analysis. Missing data on ethnicity, payer type, and hospital type were also excluded.
Study Variables
Patient age, gender, ethnicity, payer type, and comorbidities provided by the NIS dataset were listed for the EA and CA groups. A comorbidity score based on the Elixhauser–Van Walraven index11 was used. Hospital characteristics were also included in our analysis. The use of EA by disease type and procedure types was also included.
Endpoints
The choice of endpoints was made a priori based on previously published studies that had conflicting results.1,4,7,8,12–18 The endpoints examined include mortality, respiratory failure, pneumonia, ileus, anastomotic leak, urinary tract infection (UTI), urinary retention, wound complications, total hospital charges, and length of stay.
Statistical Analysis
All statistical analyses were conducted using SAS version 9.3 and the R Statistical Environment. Chi-square test and the t test were used for univariate analysis. Multivariate logistic and linear regression were used to compare the selected endpoints after controlling for age, gender, ethnicity, payer type, comorbidities, hospital factors, disease type, and procedure type. For anastomotic complications, APR and cases performed with an end ostomy were excluded. We also accounted for the use of diverting stoma. Because of the different nature and complexities involved in colon and rectal resections, we performed two separate analyses of outcomes: one for the colonic subgroup and another for the rectal subgroup. Odds ratios were obtained with 95 % confidence intervals. Robust standard errors were used for inference. Statistical significance was declared if p < 0.05.
Results
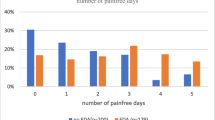
Based on our sampling criteria, a total of 888,135 patients underwent elective open colon and rectal resections in the USA over the study period. Epidurals were only used in 39,345 cases (4.4 %). The use of epidurals remained low over the study period without showing an obvious trend (Fig. 1).
Mean patient age was 65 years both in the CA and EA groups (p = 1). Gender distribution was also similar as there were 52.46 % females in the CA group and 51.69 % females in the EA group (p = 0.18). Although ethnicity and payer type were distributed similarly in both groups, EA was more likely to be used in Caucasians (65.69 vs. 60.48 %; p < 0.001) and in patients with private insurance (27.56 vs. 25.98 %; p = 0.002) (Table 1).
Looking at patient comorbidities, EA was more likely to be used in patients with metastatic cancer (22.85 vs. 19.61 %; p < 0.001) and, interestingly, obese patients with a BMI >30 (7.56 vs. 6.45 %; p < 0.001). EA was less likely to be used in patients with congestive heart failure (4.60 vs. 5.28 %; p = 0.02) and chronic kidney disease (2.00 vs. 2.56 %; p = 0.003). No differences were observed in the calculated comorbidity scores (Table 1).
The use of epidurals was different depending on hospital status. In teaching hospitals, epidurals were used in 5.03 % of cases compared to 3.92 % in non-teaching hospitals (p < 0.001). This difference was seen when comparing hospital bed size as epidurals were less likely to be used in small hospitals (3.62 %) and more likely to be used in medium-sized (4.38 %) or large hospitals (4.53 %) (p < 0.01 for difference between medium and large hospital compared with small hospitals) (Table 2).
Examining disease types, we found that colon resections for cancer accounted for the majority of cases in both groups. Epidural analgesia was more likely however to be used for rectal cancer cases (22.85 vs. 17.82 %; p < 0.001) and less likely to be used for benign pathology of the colon such as polyps (10.69 vs. 13.79 %; p < 0.001) and diverticular disease (25.35 vs. 28.18 %; p < 0.001). The selective use of epidurals in rectal cancer cases translated into more anterior resections and APR cases in the epidural group (p < 0.001) (Table 2). The use of diverting stoma was higher in the EA group. In colonic resections, a stoma was used in 15.35 % of cases in the EA group compared to 13.82 % in the CA group (p < 0.001). In anterior resections, a diverting stoma was used in 21.90 % of cases in the EA group vs. 20.03 % in the CA group (p < 0.001).
The outcomes of colonic and rectal cases were analyzed separately. In the colonic subgroup, after adjusting for age, gender, ethnicity, payer type, comorbidities, hospital factors, disease type, and procedure type, EA was associated with a US$4,450 reduction in hospital charges (p < 0.001) and a tendency towards lower mortality rates which did not achieve statistical significance (p = 0.06). However, EA however was associated with a higher rate of postoperative ileus OR = 1.17 (95 % CI, 1.08–1.28; p < 0.01) and a slightly longer hospital stay by 0.16 day (95 % CI, 0.01–0.32; p < 0.05). There was no association between the use of epidurals and the incidence of respiratory failure, pneumonia, anastomotic leak (the use of diverting stoma was also accounted for this endpoint), UTI, urinary retention, and wound complications (Table 3).
In patients undergoing rectal resections (Table 4), after adjusting for the same confounders, EA again lowered hospital charges by US$4,340 when compared with CA (p < 0.001). The incidences of the remaining postoperative outcomes were unaffected by EA.
Discussion
Despite superior pain control over other forms of conventional analgesia,1,2 the use of epidural analgesia in open colorectal resections is limited in the USA. This limited use which was observed across the entire study period may be due to several factors. Although, epidural analgesia is safe and does not appear to be detrimental, it lacks major benefits over other forms of analgesia as demonstrated in our results. Moreover, issues related to its cost-effectiveness may have hindered its use. It has previously been shown that epidural analgesia is associated with higher cost.19 The results of our study were the opposite: EA was associated with lower hospital charges. Our results echo the findings of a systematic review by Gendall et al.18 who found that although epidural analgesia may apparently be more costly, alternatives may incur higher indirect costs. Moreover, a prospective non-randomized study comparing different methods of perioperative analgesia found that EA was actually less costly compared to intravenous patient controlled analgesia (IV PCA) in patients undergoing major intraabdominal surgery.20 This difference in cost was attributed to the initial financial outlay and routine operational costs of IV PCA which are higher than epidurals. The findings that epidural analgesia is associated with higher cost came from older studies in the late 1990s19 when the use of PCA was not widespread as it is nowadays and hence cost comparisons were made between EA and non-opioid analgesics administered parenterally. We should however stress on the fact that although charges are a good reflection of cost, they are different entities. We have adjusted for all potential confounders such as payer type, and even took into account the incidence of postoperative complications, and our findings still held true. In the absence of plausible explanations, we believe that this is the result of unmeasured confounders. These unmeasured confounders include intensive care unit (ICU) admissions which are well known to increase cost. In a study evaluating 462 consecutive surgical cancer patients, it has been demonstrated that the use of epidurals may reduce ICU length of stay and the time spent on the ventilator.21 These explanations remain tentative however, as more proof is needed in the form of randomized controlled trials.
The limited use of epidural analgesia may be due to the lack of major benefits. Epidural analgesia appears to be associated with an increased incidence of prolonged postoperative ileus in colonic cases but had no effect on ileus in rectal cases. The majority of the studies that examined the effect of epidural analgesia on the ileus following colorectal surgery found no association,13–15,22,23 while a recent randomized controlled trial revealed a higher incidence of ileus associated with epidural analgesia.24 There are several possible reasons for our findings. First, the sensory blockade provided by EA may delay early mobilization which may prolong ileus. Second, the prolonged sympathetic blockade in the epidural group may lead to a higher intravenous fluid requirement to maintain intravascular volume in the face of vasodilatation and arterial hypotension.24 This in turn leads to edematous bowel which consequently contributes to ileus.25 Since edema tends to be more pronounced at the anastomotic site, this may explain why EA was associated with ileus in colonic procedures as most of these procedures are performed with a primary anastomosis without requiring a diverting stoma. Conversely, the lack of association between EA and ileus in rectal procedures is due to the fact that a larger number of anterior resections are performed with a diverting ileostomy located more proximally and thus the effect of edema on bowel function would be less apparent.
Epidural analgesia was associated with a slight increase in the length of stay in colonic resection but not in rectal resections. Several reports1,13,16–18,23,26 and a meta-analysis12 of 16 randomized trials found that epidural analgesia did not affect the length of stay following colorectal surgery. Only one study found a longer length of stay associated with the use of epidural analgesia.24 The remaining few studies that did show a shorter length of stay with EA were either small and non-randomized27 or contained a heterogeneous group of patients and the effect of epidural analgesia on length of stay was more pronounced in upper abdominal and thoracic surgery.21 The increase in length of stay may be due to the time needed to transition patients from EA to other forms of analgesia prior to discharge. The reason why this finding was only restricted to colonic procedures may be related to the fact that these procedures are associated with a shorter length of stay compared to rectal procedures and thus the potential effect of this transition may be more obvious. We should stress on the fact that although our results are statistically significant, their clinical significance is low as the increase in length of stay observed in colonic cases was by 0.16 day (4 h).
Epidural analgesia did not affect the incidence of respiratory failure and pneumonia in colon and rectal resection. The effect of epidural analgesia on pulmonary function and the incidence of pulmonary complications has been the subject of debate. On one hand, high thoracic epidurals bear the side effects of both pulmonary sympathetic and respiratory motor blockade which may lead to an increased risk of respiratory failure.28 On the other hand, the superior pain relief associated with epidural analgesia may reduce the detrimental effect of hypoventilation which leads to pneumonia and respiratory failure. The lack of association in our results may be explained by the fact that epidurals are inserted at the T7–T12 level where the risk of high thoracic blockade and hence respiratory failure is low.22,24,26,27 Our findings contradict the findings of a large retrospective review16 and a meta-analysis8 that showed a lower incidence of pulmonary complications associated with the use of EA. The large retrospective review was performed over a 17-year period, whereas the meta-analysis included studies over a 35-year period. Both studies noted that the effect of EA on pulmonary function diminished in more recent data years as a consequence of a reduced baseline risk of pneumonia due to a shift to safer analgesia methods. Thus, older findings were due to a lack of safety profile of systemic analgesia rather than a beneficial effect of EA. The other explanation may be that the meta-analysis also included thoracic and upper abdominal cases where the protective effects of EA were more obvious.8
Epidural analgesia did not affect the incidence of urinary retention which is in contrast to previously published studies that found a higher incidence of urinary retention with epidural analgesia.13,22,29,30 These studies which reported an incidence of urinary retention in the EA group ranging from 5.5 to 10 % were limited by small sample sizes precluding a meaningful analysis. Our results show a low incidence of urinary retention in both the EA and CA groups. The lack of association can be explained by the fact that epidurals are usually removed at least 4 h prior to the discontinuation of bladder catheters to avoid this complication.24 Since the effect of EA medication is usually short lived, the risk of urinary retention should technically be low. On the other hand, the lack of association between the use of EA and an increased risk of UTI can be explained by the fact that most institutions remove epidural and bladder catheters 48 h postoperatively to reduce the risk of UTI.
Epidural analgesia did not affect the incidence of anastomotic leak. We examined this endpoint as some authors believe that the sympathetic blockade offered by epidural analgesia may protect against anastomotic leakage because of an increased splanchnic blood flow to the anastomosis.6 On the other hand, other authors demonstrated that epidural analgesia may increase the rate of anastomotic leak due to a steal effect,31 or by causing early colonic contractions at a time where the anastomosis is still fresh.32 Our results here are consistent with the majority of studies1,14,16,33,34 and a meta-analysis12 that showed no effect. Previous studies including the meta-analysis by Marret et al.12 included 42 to 1,470 patients and their reported leak rates ranges between to 2.4 and 15.3 %. The leak rates following anterior resections in our results fall in that range. However in colonic procedures, we observed leak rates which were higher with the study by Warschkow et al.16 who found a 3.4 % incidence of anastomotic leak following colon resections. The relatively high incidence of anastomotic leakage in our study may be explained by the fact that data are collected from a wide range of hospital settings and surgeons’ expertise and the fact that we included ICD9 codes for intraabdominal and pelvic abscesses, and enterocutaneous fistula. We have to emphasize that the large numbers in our study afforded us enough power to examine this endpoint. Holte and Kehlet35 performed a power analysis to examine how many cases would be needed in each arm to detect an association between EA and anastomotic leak; they found that 1,037 patients would be needed in each arm. Despite the retrospective design of our study, we had enough numbers that enabled us to account for all potential confounders. However, many other factors such as the distance of the anastomosis from the anal verge in rectal cases and history of preoperative radiation may affect leak rates and these variables are not available in the NIS database.
Because of its anti-inflammatory effects and the potential to reduce the immunosuppression associated with surgical trauma, EA was thought to lower the incidence of wound infections, wound dehiscence,4,5 and mortality.7,16 Consistent with previous investigations,16,18 our study did not reveal an effect of EA on the incidence of wound complications. With respect to mortality, our results did not achieve statistical significance. Lower mortality associated with EA was observed in large single-center studies16 and other large population studies7; however, it was not apparent in smaller studies.1,15,17 It is difficult to explain the tendency towards lower mortality as we did not observe a decrease in the incidence of major complications.
The main limitation of our study lies in its retrospective nature and its inherent biases. The use of a population database may be prone to coding errors. NIS does not provide specific information such as pain levels, patient satisfaction, time to tolerating a diet, and the length of time the epidural or the indwelling bladder catheters were left in place. Epidural analgesia does not exclude intravenous narcotic use if the situation warrants it. Unfortunately, we were not able to adjust for this confounder due to the limitations of the database. Procedural complications specific to epidurals such as epidural hematoma, abscess, hypotension, and motor deficit are also not provided. These complications are rare but may further explain its limited use.36 There could be several unmeasured confounders that may have affected our results; however, we tried to account for this effect by adjusting for a large numbers of variables readily available. NIS only provides information related to one single hospital stay and, as such, long-term data, readmission rates, and 30-day mortality rates are unknown. However, this is likely to affect both groups. Nevertheless, to our knowledge, this study represents the largest and the most recent analysis of the use of epidural analgesia in elective open colorectal surgery.
Conclusion
The use of epidural analgesia in elective open colorectal resection is limited in the USA. Although safe, epidural analgesia does not add major clinical benefits over conventional analgesia. These results need to be validated by large randomized controlled trials.
References
Carli F, Trudel JL, Belliveau P. The effect of intraoperative thoracic epidural anesthesia and postoperative analgesia on bowel function after colorectal surgery: a prospective, randomized trial. Diseases of the colon and rectum. Aug 2001;44(8):1083-1089.
Kong SK, Onsiong SM, Chiu WK, Li MK. Use of intrathecal morphine for postoperative pain relief after elective laparoscopic colorectal surgery. Anaesthesia. Dec 2002;57(12):1168-1173.
Bredtmann RD, Herden HN, Teichmann W, et al. Epidural analgesia in colonic surgery: results of a randomized prospective study. The British journal of surgery. Jun 1990;77(6):638-642.
Wu CT, Jao SW, Borel CO, et al. The effect of epidural clonidine on perioperative cytokine response, postoperative pain, and bowel function in patients undergoing colorectal surgery. Anesthesia and analgesia. Aug 2004;99(2):502-509, table of contents.
Moselli NM, Baricocchi E, Ribero D, Sottile A, Suita L, Debernardi F. Intraoperative epidural analgesia prevents the early proinflammatory response to surgical trauma. Results from a prospective randomized clinical trial of intraoperative epidural versus general analgesia. Annals of surgical oncology. Oct 2011;18(10):2722-2731.
Johansson K, Ahn H, Lindhagen J, Tryselius U. Effect of epidural anaesthesia on intestinal blood flow. The British journal of surgery. Jan 1988;75(1):73-76.
Wu CL, Rowlingson AJ, Herbert R, Richman JM, Andrews RA, Fleisher LA. Correlation of postoperative epidural analgesia on morbidity and mortality after colectomy in Medicare patients. Journal of clinical anesthesia. Dec 2006;18(8):594-599.
Popping DM, Elia N, Marret E, Remy C, Tramer MR. Protective effects of epidural analgesia on pulmonary complications after abdominal and thoracic surgery: a meta-analysis. Archives of surgery. Oct 2008;143(10):990-999; discussion 1000.
Kang CY, Halabi WJ, Luo R, Pigazzi A, Nguyen NT, Stamos MJ. Laparoscopic colorectal surgery: a better look into the latest trends. Archives of surgery. Aug 2012;147(8):724-731.
HCUP (2012) Healthcare cost and utilization project—Nationwide Inpatient Sample
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Medical care. Jun 2009;47(6):626-633.
Marret E, Remy C, Bonnet F. Meta-analysis of epidural analgesia versus parenteral opioid analgesia after colorectal surgery. The British journal of surgery. Jun 2007;94(6):665-673.
Carli F, Mayo N, Klubien K, Schricker T, Trudel J, Belliveau P. Epidural analgesia enhances functional exercise capacity and health-related quality of life after colonic surgery: results of a randomized trial. Anesthesiology. Sep 2002;97(3):540-549.
Lehman JF, Wiseman JS. The effect of epidural analgesia on the return of peristalsis and the length of stay after elective colonic surgery. The American surgeon. Nov 1995;61(11):1009-1012.
Kuruba R, Fayard N, Snyder D. Epidural analgesia and laparoscopic technique do not reduce incidence of prolonged ileus in elective colon resections. American journal of surgery. Nov 2012;204(5):613-618.
Warschkow R, Steffen T, Luthi A, et al. Epidural analgesia in open resection of colorectal cancer: is there a clinical benefit? a retrospective study on 1,470 patients. J Gastrointest Surg. Aug 2011;15(8):1386-1393.
Liu SS, Carpenter RL, Mackey DC, et al. Effects of perioperative analgesic technique on rate of recovery after colon surgery. Anesthesiology. Oct 1995;83(4):757-765.
Gendall KA, Kennedy RR, Watson AJ, Frizelle FA. The effect of epidural analgesia on postoperative outcome after colorectal surgery. Colorectal Dis. Sep 2007;9(7):584-598; discussion 598-600.
Bartha E, Carlsson P, Kalman S. Evaluation of costs and effects of epidural analgesia and patient-controlled intravenous analgesia after major abdominal surgery. British journal of anaesthesia. Jan 2006;96(1):111-117.
Shapiro A, Zohar E, Hoppenstein D, Ifrach N, Jedeikin R, Fredman B. A comparison of three techniques for acute postoperative pain control following major abdominal surgery. Journal of clinical anesthesia. Aug 2003;15(5):345-350.
de Leon-Casasola OA, Parker BM, Lema MJ, Groth RI, Orsini-Fuentes J. Epidural analgesia versus intravenous patient-controlled analgesia. Differences in the postoperative course of cancer patients. Regional anesthesia. Sep-Oct 1994;19(5):307-315.
Neudecker J, Schwenk W, Junghans T, Pietsch S, Bohm B, Muller JM. Randomized controlled trial to examine the influence of thoracic epidural analgesia on postoperative ileus after laparoscopic sigmoid resection. The British journal of surgery. Oct 1999;86(10):1292-1295.
Turunen P, Carpelan-Holmstrom M, Kairaluoma P, et al. Epidural analgesia diminished pain but did not otherwise improve enhanced recovery after laparoscopic sigmoidectomy: a prospective randomized study. Surg Endosc. Jan 2009;23(1):31-37.
Levy BF, Scott MJ, Fawcett W, Fry C, Rockall TA. Randomized clinical trial of epidural, spinal or patient-controlled analgesia for patients undergoing laparoscopic colorectal surgery. The British journal of surgery. Aug 2011;98(8):1068-1078.
Holte K, Sharrock NE, Kehlet H. Pathophysiology and clinical implications of perioperative fluid excess. British journal of anaesthesia. Oct 2002;89(4):622-632.
Zingg U, Miskovic D, Hamel CT, Erni L, Oertli D, Metzger U. Influence of thoracic epidural analgesia on postoperative pain relief and ileus after laparoscopic colorectal resection: benefit with epidural analgesiaSurg Endosc. Feb 2009;23(2):276-282.
Senagore AJ, Whalley D, Delaney CP, Mekhail N, Duepree HJ, Fazio VW. Epidural anesthesia-analgesia shortens length of stay after laparoscopic segmental colectomy for benign pathology. Surgery. Jun 2001;129(6):672-676.
Takasaki M, Takahashi T. Respiratory function during cervical and thoracic extradural analgesia in patients with normal lungs. British journal of anaesthesia. Dec 1980;52(12):1271-1276.
Paulsen EK, Porter MG, Helmer SD, Linhardt PW, Kliewer ML. Thoracic epidural versus patient-controlled analgesia in elective bowel resections. American journal of surgery. Dec 2001;182(6):570-577.
Senagore AJ, Delaney CP, Mekhail N, Dugan A, Fazio VW. Randomized clinical trial comparing epidural anaesthesia and patient-controlled analgesia after laparoscopic segmental colectomy. The British journal of surgery. Oct 2003;90(10):1195-1199.
Sala C, Garcia-Granero E, Molina MJ, Garcia JV, Lledo S. Effect of epidural anesthesia on colorectal anastomosis: a tonometric assessment. Diseases of the colon and rectum. Aug 1997;40(8):958-961.
Bigler D, Hjortso NC, Kehlet H. Disruption of colonic anastomosis during continuous epidural analgesia. An early postoperative complication. Anaesthesia. Mar 1985;40(3):278-280.
Ryan P, Schweitzer SA, Woods RJ. Effect of epidural and general anaesthesia compared with general anaesthesia alone in large bowel anastomoses. A prospective study. Eur J Surg. Jan 1992;158(1):45-49.
Lai R, Lu Y, Li Q, Guo J, Chen G, Zeng W (2012) Risk factors for anastomotic leakage following anterior resection for colorectal cancer: the effect of epidural analgesia on occurrence. International journal of colorectal disease. 2012. doi: 10.1007/s00384-012-1585-5
Holte K, Kehlet H. Epidural analgesia and risk of anastomotic leakage. Reg Anesth Pain Med. Mar-Apr 2001;26(2):111-117.
Cook TM, Counsell D, Wildsmith JA. Major complications of central neuraxial block: report on the Third National Audit Project of the Royal College of Anaesthetists. British journal of anaesthesia. Feb 2009;102(2):179-190.
Conflict of Interest
The authors have no disclosures or conflict of interest related to the content of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Halabi, W.J., Jafari, M.D., Nguyen, V.Q. et al. A Nationwide Analysis of the Use and Outcomes of Epidural Analgesia in Open Colorectal Surgery. J Gastrointest Surg 17, 1130–1137 (2013). https://doi.org/10.1007/s11605-013-2195-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-013-2195-4