Abstract
Purpose
Vertebral fractures (VFs) are the hallmark of osteoporosis and are responsible for almost 70,000 hospital admissions yearly, implying social costs and impaired quality of life for patients. In recent years, several techniques, both qualitative and quantitative, have been proposed for VF diagnosis, but a gold standard is not yet available and the visual semiquantitative (VSQ) assessment proposed by Genant remains the most validated. However, given the lack of a standardised method, in clinical practice, the diagnosis of VF is often missed, and patients are not correctly assessed. The aim of our study was to estimate the percentage of VFs not detected in clinical practice in italian population using the VSQ method and a new morphometric technique.
Materials and methods
In 283 postmenopausal women referred to our clinic for osteoporosis screening, we performed a clinical examination, plain spinal radiographs (for VSQ assessment) and digital computerised morphometry (DCM) to assess VFs. Bone density was measured using dual-energy X-ray absorptiometry (DXA).
Results
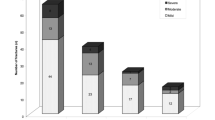
Forty-seven percent of patients had a T score <−2.5 standard deviations (SD), and 35.2% were osteopenic, but no significant correlations between T score and grade or number of fractures were found. DCM identified VFs in 38.5% of patients versus 32.5% using the VSQ method. Overall, 280 VFs were detected by DCM and 236 by VSQ, whereas only 105 were recognised by the reports.
Conclusions
VFs went undetected in 55.5% according to the VSQ method on standard spinal radiographs. Therefore, the morphometric technique may be helpful when performed with the semiquantitative approach to improve recognition of VFs. However, other studies are needed to further validate the utility of this new morphometric technique in clinical practice.
Riassunto
Obiettivo
Le fratture vertebrali (FV) rappresentano il segno caratteristico dell’osteoporosi e sono responsabili di circa 70000 ricoveri ospedalieri ogni anno, con notevoli implicazioni per quel che concerne i costi sociali e la scadente qualità di vita dei pazienti. Negli ultimi anni diverse tecniche, sia qualitative che quantitative, sono state proposte per la diagnosi di FV, ma allo stato attuale non è ancora disponibile una metodica considerata gold standard e la valutazione visiva semiquantitativa (VSQ) proposta da Genant, resta la più validata. Comunque, data l’assenza di una metodica standardizzata, nella pratica clinica quotidiana le FV sono spesso misconosciute e quindi i pazienti non sono correttamente valutati.
Materiali e metodi
Scopo del nostro studio è stato quello di valutare la percentuale di FV non diagnosticate nella pratica clinica in una popolazione italiana, usando il metodo VSQ e una nuova tecnica morfometrica. Per la valutazione delle FV, in 283 donne in età postmenopausale giunte alla nostra osservazione per lo screening dell’osteoporosi, abbiamo effettuato: l’esame clinico, i radiogrammi tradizionali del rachide (per il metodo VSQ) e la morfometria digitale computerizzata (MDC). La densità ossea è stata misurata utilizzando l’apparecchiatura dual energy X-ray absorptiometry (DXA).
Risultati
Il 47% dei pazienti presentava un T score<−2,5 deviazioni standard (DS) ed il 35,2% presentava una condizione osteopenica, tuttavia non è stata riscontrata alcuna correlazione significativa tra il T score e il grado o numero di fratture riscontrate. La MDC ha identificato le FV nel 38,5% dei pazienti rispetto al 32,5% del metodo VSQ. Complessivamente, la MDC ha identificato 280 FV, 236 sono state diagnosticate mediante approccio VSQ, mentre soltanto 105 FV sono state riportate nei referti.
Conclusioni
Le FV sono state sottostimate nel 55,5% dei casi in accordo con il metodo VSQ effettuato sui radiogrammi standard del rachide. Pertanto, la tecnica morfometrica rappresenta una metodica valida, complementare all’approccio semiquantitativo, al fine di migliorare il riconoscimento delle FV. Sono comunque necessari ulteriori studi per validare maggiormente l’utilità di questa nuova tecnica morfometrica nella pratica clinica.
Similar content being viewed by others
References/Bibliografia
Link TM, Guglielmi G, van Kuijk C, Adams JE (2005) Radiologic assessment of osteoporotic vertebral fractures: diagnostic and prognostic implications. Eur Radiol 15:1521–1532
Gehlbach SH, Burge RT, Puleo E, Klar J (2003) Hospital care of osteoporosisrelated vertebral fractures. Osteoporos Int 14:53–60
Ross PD (1997) Clinical consequences of vertebral fractures. Am J Med 103:S30–S43
Gehlbach SH, Bigelow C, Heimisdottir M et al (2000) Recognition of vertebral fracture in a clinical setting. Osteoporos Int 11:577–582
Andrade SE, Majumdar SR, Chan KA et al (2003) Low frequency of treatment of osteoporosis among postmenopausal women following a fracture. Arch Intern Med 163:2052–2057
Angeli A, Guglielmi G, Dovio A et al (2006) High prevalence of asymptomatic vertebral fractures in post-menopausal women receiving chronic glucocorticoid therapy: a cross-sectional study. Bone 39:253–259
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1935
World Health Organization Study Group (1984) Assessment of fracture risk and its application to postmenopausal osteoporosis. World Health Organ Teach Ser 843
Ross PD, Davis JW, Epstein RS (1991) Pre-existing fractures and bone mass predict vertebral fracture incidence in women. Ann Intern Med 114:919–923
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Guglielmi G, Stoppino LP, Placentino MG et al (2009) Reproducibility of a semi-automatic method for 6-point vertebral morphometry in a multicentre trial. Eur J Radiol 69:173–178
Guglielmi G, Palmieri F, Placentino MG et al (2009) Assessment of osteoporotic vertebral fractures using specialized workflow software for 6-point morphometry. Eur J Radiol 70:142–148
Genant HK, Jergas M, Palermo L et al (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 11:984–996
Kim N, Rowe BH, Raymond G et al (2004) Underreporting of vertebral fractures on routine chest radiography. AJR Am J Roentgenol 182:297–300
Mui LW, Haramati LB, Alterman DD et al (2003) Evaluation of vertebral fractures on lateral chest radiographs of inner-city postmenopausal women. Calcif Tissue Int 73:550–554
Majumdar SR, Kim N, Colman I et al (2005) Incidental vertebral fractures discovered with chest radiography in the emergency department: prevalence, recognition, and osteoporosis management in a cohort of elderly patients. Arch Intern Med 165:905–909
Cataldi V, Laporta T, Sverzellati N et al (2008) Detection of incidental vertebral fractures on routine lateral chest radiographs. Radiol Med 113:968–977
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Delmas PD, Van de Langerijt L, Watts NB et al (2005) Underdiagnosis of vertebral fractures is a worldwide problem: The IMPACT study. J Bone Miner Res 20:557–563
Diacinti D, Guglielmi G, Tomei E et al (2001) Vertebral morphometry: evaluation of osteoporosis-caused fractures. Radiol Med 101:140–144
O’Neill TW, Cockerill W, Matthis C et al (2004) Back pain, disability and radiographic vertebral fracture in European women: a prospective study. Osteoporos Int 15:760–765
Nevitt MC, Ettinger B, Black DM et al (1998) The associations of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med 128:793–800
Kado DM, Browner WS, Palermo L et al (1999) Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med 159:1215–1220
Jinbayashi H, Aoyagi K, Ross PD et al (2002) Prevalence of vertebral deformity and its associations with physical impairment among Japanese women: The Hizen-Oshima Study. Osteoporos Int 13:723–730
Burger H, Van Daele PLA, Gashuis K et al (1997) Vertebral deformities and functional impairment in men and women. J Bone Miner Res 12:152–157
Ross PD, Genant HK, Davis JW et al (1993) Predicting vertebral fracture incidence from prevalent fractures and bone density among non-black, osteoporotic women. Osteoporos Int 3:120–126
Rea JA, Li J, Blake GM et al (2000) Visual assessment of vertebral deformity by X-ray absorptiometry: a highly predictive method to exclude vertebral deformity. Osteoporos Int 11:660–668
Rea JA, Chen MB, Li K et al (2000) Morphometric X-ray absorptiometry and morphometric radiography of the spine: a comparison of prevalent vertebral deformity identification. J Bone Miner Res 15:564–574
Grados F, Roux C, de Vernejoul MC et al (2001) Comparison of four morphometric definitions and a semiquantitative consensus reading for assessing prevalent vertebral fractures. Osteoporos Int 12:716–722
Guglielmi G, Diacinti D, van Kuijk C et al (2008) Vertebral morphometry: current methods and recent advances. Eur Radiol 18:1484–1496
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Difede, G., Scalzo, G., Bucchieri, S. et al. Underreported vertebral fractures in an Italian population: comparison of plain radiographs vs quantitative measurements. Radiol med 115, 1101–1110 (2010). https://doi.org/10.1007/s11547-010-0554-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-010-0554-8