Abstract
A cross-sectional survey of 298 pregnant women from Cape Town, South Africa was conducted to examine socio-demographic, reproductive health, mental health, and relationship correlates of lifetime trauma exposure and whether these correlates vary as a function of age. Overall, 19.8 % of participants reported trauma exposure. We found similarities and differences in correlates of trauma exposure among women in emerging adulthood and older women. Prior termination of pregnancy was associated with trauma exposure in both age groups. Difficulties in resolving arguments, lifetime substance use, and a prior sexually transmitted infection were associated with trauma exposure among women in emerging adulthood. In contrast, depression and awareness of substance abuse treatment programmes were associated with trauma exposure among older women. These findings highlight the need for interventions that prevent and treat trauma exposure among vulnerable women. Such interventions should be tailored to address the correlates of trauma exposure in each age group.
Similar content being viewed by others
Background
Parts of South African society experience high levels of exposure to traumatic events (Kaminer et al. 2008), such as violent crime (Jewkes and Abrahams 2002; Seedat et al. 2009a, b), child abuse and neglect (Kaminer et al. 2013; Suliman et al. 2009), and intimate partner violence (IPV) (Gass et al. 2010; Jewkes et al. 2002). South African women are particularly at risk for trauma related to IPV, sexual assault, and childhood abuse (Kaminer et al. 2008), with between 20 and 50 % of South African women having lifetime histories of exposure to these types of trauma (Dunkle et al. 2004; Gass et al. 2010; Jewkes et al. 2002).
Among women, a history of trauma exposure is associated with the development of common mental disorders such as post-traumatic stress disorder, depression, and substance use disorders (Kaminer et al. 2013; Nabakulu et al. 2013; Seedat et al. 2009a, b), which not only reduce women’s quality of life but also increase risk of HIV acquisition from increased sexual-risk taking behaviour (Jewkes et al. 2010; Myers et al. 2013; Wechsberg et al. 2013). These correlates of trauma exposure have also been found among pregnant women. Several studies conducted in the USA and other high-income countries document that trauma exposure either prior to or during pregnancy increases the likelihood of antenatal and postnatal depression, and other postpartum mental health problems (Beydoun et al. 2012; Lesser et al. 2007; Meltzer-Brody et al. 2013). A history of trauma exposure is also associated with greater difficulties in coping with stressors, more conflict in relationships and lower perceived social support (Monson et al. 2009; Punamaki et al. 2005). When present during pregnancy, these factors exacerbate the risk for postpartum mental health difficulties (Divney et al. 2012; Ghosh et al. 2010).
This is cause for concern as maternal mental health difficulties are associated with poorer infant neonatal outcomes, including increased risk of low birth weight, preterm delivery, and the need for neonatal ICU care (El-Kady et al. 2004; Silverman et al. 2006). Untreated mental health difficulties during pregnancy also disrupt the mother-infant relationship, increasing the risk of adverse developmental and health outcomes for the infant (Forman et al. 2007; Fowler et al. 2013). In South Africa where there are very high rates of maternal and infant morbidity and mortality (Chopra et al. 2009), intervening with trauma-exposed pregnant women to mitigate the risk of adverse mental health outcomes may be critical to efforts to reduce maternal and infant morbidity and mortality.
The development of such interventions has been constrained by a dearth of locally relevant knowledge on correlates of lifetime trauma exposure among pregnant women. Only a handful of studies (Choi et al. 2014; Hartley et al. 2011) have explored the correlates of trauma exposure among pregnant women from low-and middle-income countries. These studies have methodological limitations in that they only examine the mental health outcomes of prior trauma exposure (despite the fact that the US literature also identifies reproductive health and relationship correlates of trauma exposure among pregnant women). Furthermore, research on this topic has largely examined correlates of trauma exposure among populations of pregnant women undifferentiated by age. A substantial proportion of women attending antenatal services in South Africa are in emerging adulthood, defined as being between 18 and 25 years of age (Williams et al. 2013). This developmental period has been associated with heightened risk of substance use involvement, sexual-risk taking behavior, and relationship conflict relative to adulthood (Harris et al. 2006; Nelson and Barry 2005). Consequently, the correlates of lifetime trauma exposure for pregnant women in emerging adulthood could differ substantially from those among older women; yet these potential age differences remain unexplored. This knowledge gap limits our ability to develop interventions tailored to address the specific needs associated with trauma exposure among younger and older women.
As a first step to addressing this gap, we explored the reproductive health, mental health, and relationship correlates of lifetime trauma exposure among pregnant women attending antenatal services in a low-income community in Cape Town. We hypothesized that correlates of lifetime trauma exposure would differ among women in emerging adulthood and older women. As a result, we also compared and contrasted the profile of variables associated with trauma exposure among younger and older pregnant women.
Methods
This article reports findings from a cross-sectional survey nested within a study that sought to develop and initially evaluate an integrated model of HIV prevention and substance use treatment for pregnant women (Jones et al. 2014).
Study Setting
The survey took place at three community-based midwife obstetric units (MOUs) located within the Metro-North district of Cape Town. MOUs are midwife managed facilities that provide free antenatal and postpartum care to pregnant women in low-income communities who do not have medical insurance. Women with uncomplicated pregnancies present at these clinics for “booking,” the first antenatal appointment during which comprehensive obstetric services are initiated.
Participants and Procedures
During April to June 2013 we recruited pregnant women waiting for their first appointment at the selected MOUs. Participants were recruited simultaneously from the three MOUs, which had different days assigned for first appointments. At each MOU, project staff approached pregnant women as they waited for their appointment and asked if they would be willing to complete an interviewer-administered questionnaire. Every second woman was approached and asked to participate in the survey. To ensure that the women were sampled in a systematic manner and to avoid recruitment biases, field staff distributed numbers to all women waiting for an appointment. The staff approached only women with even numbers for possible study inclusion.
A screener was administered to determine eligibility. To be eligible for inclusion in this survey, participants had to be women residing in low-income communities within the Metro-North district of Cape Town, no younger than 18 years of age, currently pregnant, and willing to answer questions of a personal nature regarding their pregnancy, habits, and relationships with partners. Women who were ineligible or unwilling to participate were replaced by the woman with the next consecutive even number. Project staff obtained consent from eligible women and administered the pen-and-paper survey to consenting participants in a private space in the MOU. The survey was administered in English or Afrikaans, the primary languages spoken in the communities located within the MOUs’ catchment areas. The survey took approximately 30 minutes to complete. Participants received a gift card to the value of ZAR 30 (roughly USD 4) as compensation for their time.
Measures
The survey was a modified Revised Risk Behavior Assessment (RRBA) adapted for use among pregnant women in the Western Cape (Jones et al. 2014). The RRBA collects self-reported information on socio-demographic characteristics, sexual and reproductive health, mental health and substance use, quality of relationships with partner, and trauma exposure. To address our study aims, we explored associations between lifetime trauma exposure and various socio-demographic, reproductive and sexual health, mental health, and quality of relationship variables.
Trauma Exposure
Lifetime exposure to trauma, was assessed with the question “Have you experienced a traumatic event in your lifetime?” Interviewers explained the definition of a traumatic event to participants, namely the experiencing or witnessing of an incident where there was a threat of or actual serious injury or death, to which the person responded with strong feelings of fear, helplessness, or horror. An open-ended question assessed the type of traumatic event to which they had been exposed.
Socio-Demographic Variables
Socio-demographic variables included age (18–25 and ≥26 years of age); ethnicity, specifically whether the participant self-identified as Black African, Coloured (in South Africa, the term “Coloured” is an officially accepted descriptor of ethnicity and describes people of mixed race ancestry who have their own language and cultural traditions), White, or Asian/Indian; and education (whether or not the person had completed high school). We also enquired about employment status (employed vs. unemployed) and marital status (married/cohabiting vs. not married/cohabiting).
Sexual and Reproductive Health
Participants were asked whether this was their first pregnancy and whether they had ever had a previous pregnancy terminated through miscarriage, abortion, or stillbirth. Participants were also asked if they had ever been treated for an STI and an STI symptom checklist was used to assess whether they currently had symptoms clinically indicative of an STI.
Mental Health and Substance Use
We used the Center for Epidemiological Studies Depression (CES-D) scale to measure symptoms of depression during the past week (Radloff 1977). This scale consists of 20 items that are rated on a four-point Likert scale with responses ranging from 0 (No symptom presence) to 3 (Symptoms are present most or all of the time). Composite scale scores range from 0 to 60, with a score of 16 or higher signifying risk of clinically meaningful depression (Radloff 1977). Participants who scored above this cutoff were provided with a referral to mental health services. Among different populations, the CES-D has shown acceptable psychometric properties (Naughton and Wiklund 1993) and has been validated for use in South Africa (Hamad et al. 2008). This study obtained a Cronbach’s alpha coefficient of 0.89 for the CES-D.
We used the 10-item Kessler psychological distress scale (K-10) to examine extent of current psychological distress (Kessler et al. 2002). Psychological distress is a broad term that reflects emotional distress and suffering and as such it is conceptually distinct from clinical depression. K-10 items ask about frequency of symptoms experienced in the past month, with responses ranging from 1 (None of the time) to 5 (All of the time). Composite scores range from 10 to 50, with higher scores indicating more symptoms of current nonspecific psychological distress. Prior research with South African populations, including pregnant women, has indicated good reliability and validity (Spies et al. 2009). This study obtained a Cronbach’s alpha coefficient of 0.90 for the K-10. We used the K-10 as a continuous measure because we were interested in exploring the extent of current psychological distress.
For substance use, we included items that asked about current substance use (defined as any past week use of alcohol or other drugs), lifetime substance use, and awareness of treatment programmes for substance use disorders.
Relationship Quality with Partner
We explored the extent to which participants viewed the father of their child as supportive of the pregnancy. Response options ranged from 1 (Not at all) to 4 (Considerably), which were collapsed because of small cell sizes. We also examined the degree to which participants experienced difficulty in resolving arguments with their partners, with response options ranging from 1 (No difficulty) to 4 (Great difficulty). As responses were skewed, we recoded this variable into two response categories: no difficulty vs. any difficulty. In addition, for the 28 women (9 %), who either declined or reported that they did not know, we coded them as having any difficulty. This coding preserved the sample size for multivariable analysis. We also examined the perceived quality of women’s relationship with their partner. Response options ranged from 1 (Excellent) to 4 (Not good). As responses were skewed, we recoded this variable into three response categories: excellent, good, and less than good.
Analyses
We performed chi-square and t-tests to compare the distribution of correlates among women who did and did not report lifetime exposure to trauma. For bivariate analyses, we used logistic regression and computed crude odds ratios to identify and assess the strength of the associations among variables correlated with lifetime trauma exposure. Because we were interested in assessing the differences in the profile of factors associated with lifetime trauma exposure among pregnant women in emerging adulthood as compared with older women, subsequent analyses were stratified by ages 18–25 and ≥26 years. The stratified analyses included descriptive statistics comparing and contrasting the distribution of characteristics in each age stratum and multivariable logistic regression modelling of lifetime exposure to trauma. We selected variables to include in the multivariable models on the basis of their association with trauma exposure in bivariate analyses of the complete sample, marginal correlations among variables within each stratum, and for the entire sample, cell sizes, and ability to compare groups on key factors. The results of all regression models are reported as odds ratios (ORs) with 95 % confidence intervals (95 % CI). All statistical analyses were conducted using Stata 13 (College Station, Texas).
Results
Description of Sample
We approached 326 women for screening for potential study inclusion, of which 300 were interested in participating and agreed to be screened. Of these women, 298 met study eligibility criteria and were enrolled in the study. Participants were between 18 and 42 years of age. Women in emerging adulthood (18–253 years of age) accounted for 54.7 % of the sample (Table 1). The majority of participants were Coloured (66.1 %). More than half of participants (56.4 %) were married or cohabitating. One third (33.2 %) of participants had completed high school. In terms of parity, 46.0 % of participants were pregnant for the first time and 21.6 % reported a previous termination of pregnancy. The prevalence of ever being diagnosed with an STI was low overall (7.7 %), but 18.8 % of participants reported current symptoms clinically indicative of an STI (Table 1).
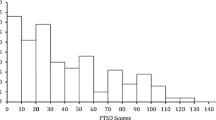
Overall 46.3 % of participants reported lifetime and 32.9 % reported current substance use. Of the 298 participants, 19.8 % reported lifetime exposure to a traumatic event. The most common traumatic event reported (35.6 %) was witnessing the death or serious injury of a close friend or family member due to gang or crime-related violence, followed by physical or sexual abuse (32.2 %), death of a family member (28.8 %), and learning that they were HIV positive (3.4 %).
Correlates of Exposure to Trauma
Most Coloured women (83.0 %) reported lifetime exposure to trauma and they were three times as likely (OR = 3.02; 95 % CI: 0.48, 1.53) as Black African women to report it (Table 1). Lifetime exposure to trauma was 2.14 (95 % CI: 1.19, 3.82) times more likely among participants who had completed high school as compared with participants who had not completed high school. In terms of reproductive health, women who reported previous termination of pregnancy were 3.37 (95 % CI: 1.48, 7.66) times as likely to report past trauma as women who did not report this experience. In addition, participants with a prior STI diagnosis had more than triple the odds (OR = 3.55; 95 % CI: 1.47, 8.56) and those with current STI symptoms had more than double the odds (OR = 2.59; 95 % CI: 1.36, 4.96) of lifetime trauma exposure compared with women without these symptoms (Table 1).
In terms of relationship quality, relative to women who reported that the quality of their relationship was excellent, women who reported that the quality of their relationship was good (OR = 3.18; 95 % CI: 1.48, 6.86) or less than good (OR = 3.72; 95 % CI: 1.70, 8.17) were significantly more likely to report prior exposure to trauma. Likewise, women who reported difficulty resolving arguments with their partner were more likely to report prior exposure to trauma (OR = 3.49; 95 % CI: 1.86, 6.54) than women without relationship conflict (Table 1).
Women who reported lifetime substance use had fourfold greater odds of reporting trauma exposure relative to women without substance use (OR = 4.07; 95 % CI: 2.17, 7.64). Similarly women who were aware of substance use treatment programmes were more than two-fold more likely to report lifetime exposure to trauma than women who were not aware of these programmes (OR = 2.48; 95 % CI: 1.35, 4.56). Women with poorer mental health were also more likely to report prior trauma than women with better mental health. For each 4-unit increase in the CES-D score, the odds of reporting past trauma increased (OR = 1.14; 95 % CI: 1.06, 1.23). Likewise, for each 3-point increase in the K-10 score, the odds of reporting prior trauma exposure increased (OR = 1.14; 95 % CI: 1.03, 1.25).
Stratified Analyses by Age
A higher proportion of women in emerging adulthood were Coloured (76.1 vs. 54.1 %, p < 0.001) and employed (77.3 vs. 57.8 %, p < 0.001; Table 2) compared with the older age group. Significantly more women in the older age group than the younger age group were married or cohabitating (74.8 vs. 41.1 %, p < 0.001). More women in the younger age group than the older age group were pregnant for the first time (60.7 vs. 28.1 %, p < 0.001) and twice as many women in emerging adulthood than older women reported a prior termination of pregnancy (31.3 vs. 15.3 %, p = 0.016). More of the younger women than older women reported current substance use (40.5 vs. 23.7 %, p = 0.002) and they had higher mean CES-D (11.6 vs. 8.0, p = 0.003) and K-10 scores (17.5 vs. 15.6, p = 0.04) than older women.
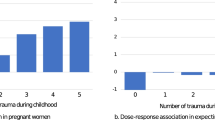
The multivariable logistic regression analyses revealed similarities and differences in factors associated with lifetime exposure to trauma for women in emerging adulthood compared with older women (Table 3). Although ethnicity was not correlated with trauma in either model, we adjusted for it because of the strength of the association in the bivariate analysis and its critical role in South Africa’s history and current sociopolitical climate. In terms of the reproductive health variables, for women in emerging adulthood (AOR = 4.00; 95 % CI: 1.09, 14.64) and older women (AOR = 4.09; 95 % CI: 1.15, 15.80), prior termination of pregnancy was associated with lifetime trauma exposure. Because the two variables related to past and current STIs were highly correlated among both younger and older women, only one of these variables was included in each age model. The choice of which variable to include was based on cell sizes. The “STI variable” was only associated with trauma exposure among women in emerging adulthood. Young women who reported a history of past STI diagnosis were almost sevenfold more likely to report past trauma exposure than women with no prior STI diagnosis (AOR = 6.95; 95 % CI: 1.41, 34.30). In terms of relationship variables, young women who had difficulty resolving arguments with their partner had fourfold greater odds of reporting prior exposure to trauma than those who reported no difficulty (AOR = 3.91; 95 % CI: 1.39, 10.97). This variable was not associated with trauma exposure among older women.
For the substance use and mental health variables, young women who reported lifetime substance use were fourfold more likely to report past trauma exposure than women with no history of substance use (AOR = 3.98; 95 % CI: 1.24, 12.77). For older women, the variables “awareness of substance abuse treatment programmes” and “lifetime substance use” were highly correlated; consequently, we excluded lifetime substance use from the model on the basis of small cell sizes. Older women who were aware of where to go for treatment had almost fourfold greater odds of reporting lifetime trauma exposure relative to women who were not aware of these services (AOR = 3.70; 95 % CI: 1.11,12.30). Among older women, every 3-unit increase in CES-D scores increased the odds of past trauma exposure by 20 % (AOR = 1.20; 95 % CI: 1.01, 1.44). This mental health variable was not associated with trauma exposure among younger women.
Discussion
This study explored health-related factors associated with a history of trauma exposure among pregnant women in South Africa, where the prevalence of exposure to trauma among women is high (Kaminer et al. 2008). Although the majority of previous studies among pregnant women in Africa report trauma exposure rates in excess of 27 % (Shamu et al. 2011), only 20 % of women in this study reported exposure to a traumatic event in their lifetime. This lower figure was surprising given the very high levels of interpersonal violence present in the catchment areas of the MOUs from which we recruited participants (Govender et al. 2012). Measurement and other methodological differences between our study and previous studies may account for this lower prevalence rate. Most other studies have asked participants to report the frequency of exposure to a broad range of adverse experiences considered to be traumatic. In contrast, this study required participants to recall whether they had ever been exposed to a traumatic event. Although many participants are likely to have been exposed to a range of adverse experiences, these experiences may not have been interpreted as traumatic, especially if these experiences are part of the fabric of social life in participants’ communities (Wechsberg et al. 2013). In addition, trauma disclosure rates may have been affected by the use of fieldworkers to administer the survey questionnaire. Other studies have reported higher disclosure rates when sensitive questions around trauma exposure are asked by people with whom pregnant women have established relationships (Shamu et al. 2011). Nonetheless, almost a fifth of women reported prior exposure to trauma, a rate much higher than those reported for US populations (Silverman et al. 2006). This highlights the urgent need to scale up efforts to prevent trauma exposure among women in this region.
In keeping with findings from studies conducted in the United States demonstrating that trauma exposure is associated with a range of adverse birth outcomes (El-Kady et al. 2004; Silverman et al. 2006), untreated trauma exposure was associated with a history of termination of pregnancy due to miscarriage, abortion and stillbirth among younger and older women in this study. While the cross-sectional nature of this study precludes a definitive understanding of the directionality of this association, it is noteworthy that none of our participants described the prior loss of a pregnancy as a traumatic event. This finding suggests that a substantial proportion of pregnant women from disadvantaged communities in Cape Town may potentially benefit from interventions that address trauma exposure and prevent adverse maternal and infant health outcomes associated with lifetime exposure to trauma.
Trauma exposure appears associated with substance use among pregnant women of all ages. Overall, a significantly greater proportion of trauma-exposed pregnant women reported lifetime substance use than non-exposed women. Among younger women, lifetime substance use was significantly associated with trauma exposure. For older pregnant women, trauma exposure was associated with increased awareness of where to go for substance abuse treatment. As this variable was strongly associated with lifetime substance use, it is likely that these older women had previous substance use problems that prompted them to seek out these services. Given the cross-sectional nature of the data and evidence from our earlier studies that substance use increases risk for victimisation (Wechsberg et al. 2013), it is possible that lifetime substance use may have preceded exposure to trauma. Even if this is the case, given the negative impact of trauma exposure on women’s ability to quit substance use (Reed et al. 2014), and our finding that almost a third of trauma-exposed pregnant women reported current substance use, efforts to mitigate the consequences of trauma exposure should include screening, brief interventions, and referral to treatment for substance use.
Additionally, our findings of differences in reproductive health and relationship difficulties associated with trauma exposure among pregnant women in emerging adulthood and older women suggest that such interventions should be tailored to the unique profile of factors associated with trauma exposure for each age group. Among pregnant women in emerging adulthood, trauma exposure was associated with having an STI (a possible indicator of sex risk behaviours) and conflict resolution difficulties. Although trauma exposure may have directly resulted in an STI (particularly if it involved sexual violence) (Dunkle et al. 2004; Jewkes et al. 2010), this would not explain why having an STI was not associated with trauma exposure for older women, as they are just as likely as younger women to have been exposed to sexual violence. One possible explanation for these findings lies in the documented relationship between trauma exposure in early life and increased likelihood of sexual risk taking and conflict in relationships in early adulthood (Schlack et al. 2013; Walsh et al. 2014). Trauma exposure in early life leads to dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis responsible for affect regulation and impulse control. Dysregulation of the HPA axis is one mechanism thought to account for the increased likelihood of sexual risk taking and conflict in intimate relationships among women in emerging adulthood (Andersen and Teicher 2009; Laurent and Power 2007). For many women, these emotional regulation processes stabilize as they transition to adulthood (Diamond and Fagundes 2008), possibly explaining why we did not observe a significant relationship between difficulties in resolving relationship conflict and trauma exposure among older women.
Because sexual risk taking and difficulties in resolving conflict in intimate relationships have long-term implications for maternal and infant health (Fowler et al. 2013), could lead to further victimisation (Lesser et al. 2007) and increase risk for HIV (Wechsberg et al. 2013), interventions are urgently needed to address these risks among pregnant women in emerging adulthood. Interventions that equip young women to resolve conflict in relationships and empower them to reduce their sex risk behaviours may reduce the risk of further adverse consequences. There is emerging evidence from high-income countries to suggest that couple-focused interventions that include parent-skills training may be effective in mitigating the effects of prior exposure to trauma on young pregnant women’s health outcomes (e.g., Lesser et al. 2007), although these interventions require adaptation to low- and middle-income country contexts and testing for effectiveness.
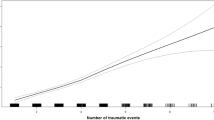
In contrast, trauma exposure was associated with depression only among older pregnant women. This was unexpected given the large body of evidence suggesting that trauma exposure is also associated with increased risk of depression among younger women (Suliman et al. 2009) and our finding that younger women had significantly more symptoms of depression than older women. Evidence that multiple exposures to trauma have a cumulative effect on risk for depression (Suliman et al. 2009; Williams et al. 2007) may help account for this finding. As a function of age, older pregnant women may have been more frequently exposed to traumatic events than pregnant women in emerging adulthood. This may explain why depression risk was associated with trauma exposure among older pregnant women only. However, this explanation remains hypothetical, as we did not measure the frequency or severity of exposure to traumatic events. To confirm this hypothesis, further studies that examine the relationship between age, frequency of trauma exposure, and risk for mental health problems are needed. Nonetheless, as untreated depression during pregnancy is associated with lasting adverse maternal and infant health outcomes (Hartley et al. 2011; Fowler et al. 2013), it is critical that trauma-exposed pregnant women at risk for depression are identified and linked to mental health treatment for depression and trauma. Detection and treatment of depression and trauma remains low in health care settings because there is not a standard protocol that requires all pregnant women attending MOUs to be screened for these difficulties (Rochat et al. 2011). More work needs to be done with health care providers to ensure that they are adequately addressing the mental health needs of this vulnerable population.
Although this study sheds light on the correlates of trauma exposure among pregnant women, it does present some limitations. First, because we collected data from three MOUs within one health district in the Cape Town metropole, the extent that findings can be generalised to other health districts in the region is unclear. Second, the cross-sectional nature of the data also makes it difficult to disentangle whether sexual risk, partner conflict, depression, and substance use preceded or followed exposure to trauma. To address this limitation, future research should consider prospective designs that enable researchers to unpack the temporal associations between variables associated with exposure to trauma. Third, the survey did not assess frequency or severity of exposure to trauma. Future studies should assess the frequency and severity of exposure to capture a more nuanced understanding of how exposure to trauma impacts on pregnant women.
Conclusions
The high rates of trauma exposure among pregnant women from disadvantaged communities in Cape Town indicate that more work is needed to prevent women’s exposure to trauma in this region. Findings suggest that while trauma-exposed pregnant women of all ages would benefit from interventions to reduce substance use, tailored interventions that target the unique profile of factors associated with trauma exposure among pregnant women in emerging adulthood and older women are also needed. Our findings suggest that older women would benefit most from linkage to mental health treatment, whereas younger women would benefit most from linkage to comprehensive services that includes not only mental health treatment but also sexual health services and conflict resolution skills. To mitigate the adverse maternal and infant health outcomes associated with diverse risk exposures, it is essential for health care providers to not only screen pregnant women for prior exposure to trauma and substance use, but link them to appropriate care and ensure they receive it.
References
Andersen, S., & Teicher, M. H. (2009). Desperately driven and no brakes: developmental stress exposure and subsequent risk for substance abuse. Neuroscience and Biobehavioral Reviews, 33, 516–524.
Beydoun, H. A., Beydoun, M. A., Kaufman, J. S., Lo, B., & Zonderman, A. B. (2012). Intimate partner violence against adult women and its association with major depressive disorder, depressive symptoms and postpartum depression: a systematic review and meta-analysis. Social Science and Medicine, 75, 959–975.
Choi, K. W., Abler, L. A., Watt, M. H., Eaton, L. A., Kalichman, S. C., Skinner, D., Pieterse, D., & Sikkema, K. J. (2014). Drinking before and after pregnancy recognition among South African women: the moderating role of traumatic experiences. BMC Pregnancy and Childbirth, 14, 97. doi:10.1186/1471-2393-14-97.
Chopra, M., Daviaud, E., Pattinson, R., Fonn, S., & Lawn, J. E. (2009). Saving the lives of South Africa’s mothers, babies, and children: can the health system deliver? The Lancet, 374, 835–846.
Diamond, L. M., & Fagundes, C. P. (2008). Developmental perspectives on links between attachment and affect regulation over the lifespan. Advances in Child Development and Behavior, 36, 83–134.
Divney, A. A., Sipsma, H., Gordon, D., Niccolai, L., Magriples, U., & Kershaw, T. (2012). Depression during pregnancy among young couples: the effect of personal and partner experiences of stressors and the buffering effects of social relationships. Journal of Pediatric and Adolescent Gynecology, 25, 201–207.
Dunkle, K. L., Jewkes, R. K., Brown, H. C., Gray, G. E., McIntryre, J. A., & Harlow, S. D. (2004). Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. The Lancet, 363, 1415–1421.
El-Kady, D., Gilbert, W. M., Anderson, J., Danielsen, B., Towner, D., & Smith, L. H. (2004). Trauma during pregnancy: an analysis of maternal and fetal outcomes in a large population. American Journal of Obstetrics and Gynecology, 190, 1661–1668.
Forman, D. R., O’Hara, M. W., Stuart, S., Gorman, L. L., Larsen, K. E., & Coy, K. C. (2007). Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Development and Psychopathology, 19, 585–602.
Fowler, J. C., Allen, J. G., Oldham, J. M., & Frueh, B. C. (2013). Exposure to interpersonal trauma, attachment insecurity and depression severity. Journal of Affective Disorders, 149, 313–318.
Gass, J. D., Stein, D. J., Williams, D. R., & Seedat, S. (2010). Intimate partner violence, health behaviours, and chronic physical illness among South African women. South African Medical Journal, 100, 582–585.
Ghosh, J. K. C., Wilhelm, M. H., Dunkel-Schetter, C., Lombardi, C. A., & Ritz, B. R. (2010). Paternal support and preterm birth, and the moderation of effects of chronic stress: a study in Los Angeles County mothers. Archives of Women's Mental Health, 13(327), 338.
Govender, I., Matzopoulos, R., Makanga, P., & Corrigall, J. (2012). Piloting a trauma surveillance tool for primary healthcare emergency centres. South African Medical Journal, 102, 303–306.
Hamad, R., Fernald, L. C. H., Karlan, D. S., & Zinman, J. (2008). Social and economic correlates of depressive symptoms and perceived stress in South African adults. Journal of Epidemiology and Community Health, 62, 538–544.
Harris, K. M., Gordon-Larsen, P., Chantala, K., & Udry, J. R. (2006). Longitudinal trends in race/ethnic disparities in leading health indicators from adolescence to young adulthood. Archives of Pediatric and Adolescent Medicine, 160, 74–81.
Hartley, M., Tomlinson, M., Greco, E., Comulada, W. S., Stewart, J., Le Roux, I., Mbewu, N., & Rotheram-Borus, M. J. (2011). Depressed moood in pregnancy: prevalence and correlates in two Cape Town peri-urban settlements. Reproductive Health, 8, 9. doi:10.1186/1742-4755-8-9.
Jewkes, R., & Abrahams, N. (2002). The epidemiology of rape and sexual coercion in South Africa: an overview. Social Science and Medicine, 55, 153–166.
Jewkes, R., Levin, J., & Penn-Kekana, L. (2002). Risk factors for domestic violence: findings from a South African cross-sectional study. Social Science & Medicine, 55, 1603–1617.
Jewkes, R. K., Dunkle, K., Nduna, M., Jama, N., & Puren, A. (2010). Associations between childhood adversity and depression, substance abuse and HIV and HSV2 incident infections in rural South African youth. Child Abuse and Neglect, 34, 833–841.
Jones, H., Myers, B., O’Grady, K., Gerbhardt, S., Theron, G. B., & Wechsberg, W. M. (2014). Initial feasibility and acceptability of a comprehensive intervention for methamphetamine-using pregnant women in South Africa. Psychiatry Journal, 2014, 929767. doi:10.1155/2014/929767.
Kaminer, D., Grimsrud, A., Myer, L., Stein, D. J., & Williams, D. R. (2008). Risk for post-traumatic stress disorder associated with different forms of interpersonal violence in Ssouth Africa. Social Science and Medicine, 67, 1589–1595.
Kaminer, D., Hardy, A., Heath, K., Mosdell, J., & Bawa, U. (2013). Gender patterns in the contribution of different types of violence to posttraumatic stress symptoms among South African urban youth. Child Abuse and Neglect, 37, 320–330.
Kessler, R. C., Andrews, G., Colpe, L. J., Hiripi, E., Mroczek, D. K., Normand, S. L., Walters, E. E., & Zaslavsky, A. M. (2002). Short screening scales to monitor population prevalences and trends in nonspecific psychological distress. Psychological Methods, 32, 959–976.
Laurent, H., & Power, S. (2007). Emotion regulation in emerging adult couples: temperament, attachment and HPA response to conflict. Biological Psychiatry, 76, 61–71.
Lesser, J., Koniak-Griffin, D., Gonzalez-Figueroa, E., Huang, R., & Cumberland, W. G. (2007). Childhood abuse history and risk behaviors among teen parents in a culturally rooted, couple-focused HIV prevention program. Journal of the Association of Nurses in AIDS Care, 18, 18–27.
Meltzer-Brody, S., Bledsoe-Mansori, S. E., Johnson, N., Killian, C., Hamer, R. M., Jackson, C., Wessel, J., & Thorp, J. (2013). A prospective study of perinatal depression and trauma history in pregnant minority adolescents. American Journal of Obstetrics and Gynecology, 28, 211.e1–211.e7.
Monson, C. N., Gradus, J. L., la Bash, H. A. J., Grifin, M. G., & Resick, P. A. (2009). The role of couples’ interacting world assumptions and relationship adjustment in women’s post-disaster PTSD symptoms. Journal of Traumatic Stress, 22, 276–281.
Myers, B., Kline, T. L., Browne, F. A., Carney, T., Parry, C. D. H., Johnson, K., & Wechsberg, W. M. (2013). Ethnic differences in alcohol and drug use and related sexual risks for HIV among vulnerable women in Cape Town, South Africa: implications for interventions. BMC Public Health, 13, 174.
Nabakulu, D., Klipstein-Grobusch, K., Herbst, K., & Newell, M. L. (2013). Mortality in women of reproductive age in rural South Africa. Global Health Action, 6, 22834. doi:10.3402/gha.v6i0.22834.
Naughton, M. J., & Wiklund, I. (1993). A critical review of dimension-specific measures of health-related quality of life in cross-cultural research. Quality of Life Research, 2, 397–432.
Nelson, L. J., & Barry, C. M. (2005). Distinguishing features of emerging adulthood: the role of self-classification as an adult. Journal of Adolescent Research, 20, 242–262.
Punamaki, R.-L., Komproe, I., Quoto, S., El-Masri, M., & de Jong, J. T. V. M. (2005). The deterioration and mobilization effects of trauma on social support: childhood maltreatment and adulthood military violence in a Palestinian community sample. Child Abuse and Neglect, 29, 351–373.
Radloff, L. S. (1977). The CES-D scale. A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401.
Reed, E., Myers, B., Novak, S. P., Browne, F. A., & Wechsberg, S. M. (2014). Experiences of violence and association with decreased drug abstinence among women in Cape Town, South Africa. AIDS and Behavior. doi:10.1007/s10461-014-0820-1.
Rochat, T. J., Tomlinson, M., Barnighausen, T., & Newell, M. L. (2011). The prevalence and clinical presentation of antenatal depression in rural South Africa. Journal of Affective Disorders, 135, 362–373.
Schlack, R., Ravens-Sieberer, U., & Petermann, F. (2013). Psychological problems, protective factors and health-related quality of life in youth affected by violence: the burden of the multiply victimized. Journal of Adolescence, 46, 587–601.
Seedat, S., Stein, D. J., Jackson, P. B., Heeringa, S. G., Williams, D. R., & Myer, L. (2009a). Life stress and mental disorders in the South African stress and health study. South African Medical Journal, 99, 375–382.
Seedat, M., van Niekerk, A., Jewkes, R., Suffla, S., & Ratele, K. (2009b). Violence and injuries in South Africa: prioritising an agenda for prevention. The Lancet, 374, 1011–1022.
Shamu, S., Abrahams, N., & Temmerman, M. (2011). A systematic review of African Studies on Intimate Partner violence against pregnant women: prevalence and risk factors. PLoS ONE, 6, e17591.
Silverman, J. G., Decker, M. R., Reed, E., & Raj, A. (2006). Intimate partner violence victimization prior to and during pregnancy among women residing in 26 U.S. states: associations with maternal and neonatal health. American Journal of Obstetrics and Gynecology, 195, 140–148.
Spies, G., Stein, D. J., Roos, A., Faure, S. C., Mostert, J., Seedat, S., & Vythilingum, B. (2009). Validity of the Kessler 10 (K-10) in detecting DSM-IV defined mood and anxiety disorders among pregnant women. Archives Women’s Mental Health, 12, 69–74.
Suliman, S., Mkabile, S. G., Fincham, D. S., Ahmed, R., Stein, D. J., & Seedat, S. (2009). Cumulative effect of multiple trauma on symptoms of posttraumatic stress disorder, anxiety, and depression in adolescents. Comprehensive Psychiatry, 50, 121–127.
Walsh, K., Latzman, N. E., & Latzman, R. D. (2014). Pathway from child sexual and physical abuse to risky sex among emerging adults: the role of trauma-related intrusions and alcohol problems. Journal of Adolescent Health, 54, 442448.
Wechsberg, W., Myers, B., Reed, E., Carney, T., Emmanuel, A. N., & Browne, F. A. (2013). Substance use, gender inequity, violence and sexual risk among couples in Cape Town. Culture, Health and Sexuality, 15, 1221–1236.
Williams, S. L., Williams, D. R., Stein, D. J., Seedat, S., Jackson, P. B., & Moomal, H. (2007). Multiple traumatic events and psychological distress: the South Africa Stress and Health Study. Journal of Traumatic Stress, 20, 845–855.
Williams, J., Ibisomi, L., Sartorius, B., Kahn, K., Collinson, M., Tollman, S., & Garenne, M. (2013). Convergence in fertility of South Africans and Mozambicans in rural South Africa 1993–2009. Global Health Action, 6, 19236. doi:10.3402/gha.v6i0.19236.
Ethics Statement
Ethics approval was granted by the Institutional Review Board of RTI International and the South African Medical Research Council’s Research Ethics Committee. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study
Conflicts of Interest and Sources of Funding
The authors have no conflicts of interest. This study was funded by U.S. National Institute on Drug Abuse (NIDA) grant R21DA030565. The views and conclusion are those of the authors and do not necessarily represent the official views of the NIDA. The funding agency had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the article; or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Myers, B., Jones, H.E., Doherty, I.A. et al. Correlates of Lifetime Trauma Exposure Among Pregnant Women from Cape Town, South Africa. Int J Ment Health Addiction 13, 307–321 (2015). https://doi.org/10.1007/s11469-015-9544-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11469-015-9544-3