Abstract
Purpose
Attempts to understand the causes of cognitive impairment in obstructive sleep apnea (OSA) are complicated by the overlap among clinical and demographic factors that may impact cognition. The goal of the current study was to isolate the contribution of hypoxemia to cognitive impairment in OSA.
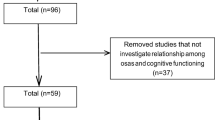
Methods
Two groups of 20 patients with newly diagnosed OSA were compared. The groups differed on severity of hypoxemia but not other demographic (e.g., age, gender, education, estimated premorbid IQ) or clinical (e.g., sleep related respiratory disturbances, daytime sleepiness, depressive symptoms) variables. Participants completed polysonmography and cognitive assessment.
Results
We compared patients with high and low hypoxemia on measures of memory, attention, executive functioning, and motor coordination using independent sample t-tests. The high hypoxemia group performed significantly better on immediate recall (Hopkins Verbal Learning Test — Revised; t = −2.50, p < 0.02) than the low hypoxemia group. No group differences were observed on other neuropsychological measures.
Conclusions
This study is one of the first to compare the cognitive performance of patients with high and low hypoxemia after controlling for demographic factors and aspects of OSA severity that could confound the relationship. In our carefully matched sample, we observed an unexpected advantage of higher hypoxemia on memory. These preliminary findings are discussed in the context of basic science literature on the protective effects of adaptation to intermittent hypoxemia. Our data suggest that the association between hypoxemia and cognition may not straightforward. Future research targeting the effects of hypoxemia on cognition controlling for other clinical factors in large groups of patients with OSA will be important.

Similar content being viewed by others
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235
Sateia MJ (2003) Neuropsychological impairment and quality of life in obstructive sleep apnea. Clin Chest Med 24(2):249–259
Golbin JM, Somers VK, Caples SM (2008) Obstructive sleep apnea, cardiovascular disease, and pulmonary hypertension. Proc Am Thorac Soc 5(2):200–206
Aloia MS, Arnedt JT, Davis JD, Riggs RL, Byrd D (2004) Neuropsychological sequelae of obstructive sleep apnea–hypopnea syndrome: a critical review. J Int Neuropsychol Soc 10(5):772–785
Twigg GL, Papaioannou I, Jackson M, Ghiassi R, Shaikh Z, Jaye J, Graham KS, Simonds AK, Morrell MJ, Twigg GL, Papaioannou I, Jackson M, Ghiassi R, Shaikh Z, Jaye J, Graham KS, Simonds AK, Morrell MJ (2009) Obstructive sleep apnea syndrome is associated with deficits in verbal but not visual memory. Am J Respir Crit Care Med 182(1):98–103
Quan S, Chan C, Dement W, Gevins A, Goodwin J, Gottlieb D, Green S, Guilleminault C, Hirshkowitz M, Hyde P, Kay G, Leary E, Nichols D, Schweitzer P, Simon R, Walsh J, Kushida C (2011) The association between Obstructive Sleep Apnea and neurocognitive performance—the Apnea Positive Pressure Long-term Efficacy Study (APPLES). Sleep 34(3):303–314
Alchanatis M, Zias N, Deligiorgis N, Liappas I, Chroneou A, Soldatos C, Roussos C (2008) Comparison of cognitive performance among different age groups in patients with obstructive sleep apnea. Sleep Breath 12:17–24
Anonymous (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 22(5):667–689
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep 14(6):540–545
Beck AT, Steer RA, Ball R, Ranieri W (1996) Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients. J Pers Assess 67(3):588–597
Spreen O, Strauss E (1998) A compendium of neuropsychological tests: administration, norms, and commentary, 2nd ed. Oxford University Press, New York, NY
Gronwall DM (1977) Paced auditory serial-addition task: a measure of recovery from concussion. Percept Mot Skills 44(2):367–373
Army Individual Test Battery: Manual of Directions and Scoring (1944). War Department, Adjuctant General's Office, Washington, DC
Benton AL, Hamsher K de S (1989) Multilingual Aphasia Examination. Iowa City, Iowa: AJA Associates
Wechsler D (1997) Wechsler Adult Intelligence Scale, 3rd ed. Pearson Assessment, San Antonio, TX
Benedict RHB, Schretlen D, Groninger L, Brandt J (1998) Hopkins Verbal Learning Test—Revised: normative data and analysis of inter-form and test–retest reliability. Clin Neuropsychol 12:43–55
Reitan RM, Davison LA (1974) Clinical neuropsychology: current status and applications. VH Winston & Sons, Oxford
Findley LJ, Barth JT, Powers DC, Wilhoit SC, Boyd DG, Suratt PM (1986) Cognitive impairment in patients with obstructive sleep apnea and associated hypoxemia. Chest 90(5):686–690
Manukhina EB, Downey HF, Mallet RT (2006) Role of nitric oxide in cardiovascular adaptation to intermittent hypoxia. Exp Biol Med 231(4):343–365
Serebrovskaya TV, Manukhina EB, Smith ML, Downey HF, Mallet RT, Serebrovskaya TV, Manukhina EB, Smith ML, Downey HF, Mallet RT (2008) Intermittent hypoxia: cause of or therapy for systemic hypertension? Exp Biol Med 233(6):627–650
Lyamina NP, Lyamina SV, Senchiknin VN, Mallet RT, Downey HF, Manukhina EB (2011) Normobaric hypoxia conditioning reduces blood pressure and normalizes nitric oxide synthesis in patients with arterial hypertension. J Hypertens 29:2265–2272
Koo BB (2012) Cerebral response to obstructive apnea: the times they are a-changin. Sleep Breath 16:269–270
Goryacheva AV, Kruglov SV, Pshennikova MG, Smirin BV, Malyshev IY, Barskov IV, Viktorov IV, Downey HF, Manukhina EB, Goryacheva AV, Kruglov SV, Pshennikova MG, Smirin BV, Malyshev IY, Barskov IV, Viktorov IV, Downey HF, Manukhina EB (2010) Adaptation to intermittent hypoxia restricts nitric oxide overproduction and prevents beta-amyloid toxicity in rat brain. Nitric Oxide 23(4):289–299
Sharp F, Ran R, Lu A, Tang Y, Strauss K, Glass T, Ardozzone T, Bernaudin M (2004) Hypoxic preconditioning protects against ischemic brain injury. NeuroRx 1:24–35
Prass K, Scharff A, Ruscher K, Lowl D, Muselmann C, Victorov I, Kapinya K, Dirnagl U (2003) Hypoxia-induced stroke tolerance in the mouse is mediated by erythropoietin. Stroke 34:1981–1986
Lopez-Ramos J, Yi P, Eleore L, Madronal N, Rueda A, Delgado-Garcia J (2007) Classical eyeblink conditioning during acute hypobaric hypoxia is improved in acclimatized mice and involves FOS expression in selected brain areas. J Appl Physiol 103:1479–1478
Almendros I, Farré R, Planas A, Torres M, Bonsignore M, Navajas D, Montserrat JM (2011) Tissue oxygenation in brain, muscle, and fat in a rat model of sleep apnea: differential effect of obstructive apneas and intermittent hypoxia. Sleep 34(8):1127–1133
Almendros I, Montserrat JM, Torres M, Gonzalez C, Navajas D, Farre R (2010) Changes in oxygen partial pressure of brain tissue in an animal model of obstructive apnea. Respir Res 11:3
Lavie P, Lavie L (2009) Unexpected survival advantage in elderly people with moderate sleep apnea. J Sleep Res 18:397–403
Petito K, Feldmann E, Pulsinelli WA, Plum F (1987) Delayed hippocampal damage in humans following cardiorespiratory arrest. Neurol 37:1281–1286
Rempel-Clower NL, Zola-Morgan SM, Squire LR, Amaral DG (1996) Three cases of enduring memory impairment after bilateral damage limited to the hippocampal formation. J Neurosci 16:5233–5255
Rybnikova E, Sitnik N, Gluschenko T, Tjulkova E, Samoilov MO (2006) The preconditioning modified neuronal expression of apoptosis-related proteins of Bcl-2 superfamily following severe hypobaric hypoxia in rats. Brain Res 1089:195–202
Rybnikova E, Vataeva L, Tyulkova E, Gluschenko T, Otellin V, Telto-Huikko M, Samoilov MO (2005) Mild hypoxia preconditioning prevents impairment of passive avoidance learning and suppression of brain NGFI-A expression induced by severe hypoxia. Behav Brain Res 160:107–114
Manukhina EB, Pshennikova MG, Goryacheva AV, Khomenko IP, Mashina SY, Pokidyshev DA, Malyshev IY (2008) Role of nitric oxide in prevention of cognitive disorders in neurodegenerative brain injuries in rats. Bull Exp Biol Med 146(4):391–395
Acknowledgements
This work was supported by the National Institutes of Health [Grant HL067209]. Dr. Aloia takes responsibility as the guarantor of the work presented in the manuscript. All authors assisted in reviewing and editing of the manuscript. Additionally, Dr. Hoth, Ms. Meschede, Dr. Zimmerman, and Dr. Aloia engaged in data analysis and interpretation, Dr. Aloia and Dr. Zimmerman contributed to the design of the study, and Dr. Arnedt assisted in data collection. The authors acknowledge Dr. Richard P. Millman, Leisha Smith, Jaime Skrekas, Sarah Harris, and Charleen Pysz for assistance with patient recruitment, neuropsychological assessment, and data entry.
Conflict of interest
Dr. Zimmerman has received investigator-initiated research funding from Merck Sharp and Dohme Corp., and Bristol-Myers Squibb. Dr. Aloia is a paid employee and stockholder for Philips/Respironics, Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
Institutions at which work was performed: Brown University, Rhode Island Hospital, National Jewish Health
Rights and permissions
About this article
Cite this article
Hoth, K.F., Zimmerman, M.E., Meschede, K.A. et al. Obstructive sleep apnea. Sleep Breath 17, 811–817 (2013). https://doi.org/10.1007/s11325-012-0769-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-012-0769-0