Abstract
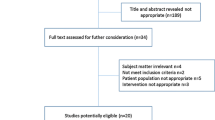
A significant proportion of the outcomes reported in trials assessing venous thromboembolism (VTE) prophylaxis in medical patients are related to asymptomatic events found on routine imaging studies. The implications of these events are controversial. Moreover, such trials did not always reflect the patient mix in today’s internal medicine departments. We summarized the evidence assessing the rate of symptomatic VTE events and the benefit of pharmacological prophylaxis in unselected medical patients, and formally evaluated the benefit versus risk of this intervention. We searched MEDLINE, EMBASE and CENTRAL until June 2011 for studies that prospectively followed cohorts of medical patients and assessed the rates of VTE, and randomized controlled trials reporting the effect of prophylaxis on these events, at 3 weeks and 3 months. Eight trials were included. The rates of symptomatic VTE were 0.69 and 3.7 % for short term and long term follow-up periods, respectively. In the interventional meta-analysis, the odds ratio (OR) for overall mortality and for symptomatic VTE at 3 weeks were 0.93 and 0.59, favouring intervention. The OR for major bleeding at 3 weeks was 2.0, favouring no intervention. None of these results were statistically significant. The number needed to treat to prevent one overt VTE event was 292, while the number needed to treat for an additional major bleeding was 336. In unselected medical patients, the rate of symptomatic VTE is lower than the reported overall VTE rate, and the benefit to risk ratio of pharmacological intervention for alleviating this condition in at-risk medical inpatient is questionable. Further specifying the population at risk for an overt VTE, and the clinical significance of asymptomatic events, is warranted.


Similar content being viewed by others
References
Antiplatelet Trialists’ Collaboration (1994): Collaborative overview of randomised trials of antiplatelet therapy. III. Reduction in venous thrombosis and pulmonary embolism by antiplatelet prophylaxis among surgical and medical patients. BMJ.;308:235–246
Heit JA, Silverstein MD, Mohr DN, Petterson TM, O’Fallon WM, Melton LJI (2000) Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case-control study. Arch Intern Med 160:809–815
Anderson FAJ, Wheeler HB, Goldberg RJ (1991) A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism: the Worcester DVT Study. Arch Intern Med 151:933–938
Goldhaber SZ, Dunn K, MacDougall RC (2000) New onset of venous thromboembolism among hospitalized patients at Brigham and women’s hospital is caused more often by prophylaxis failure than by withholding treatment. Chest 118:1680–1684
Goldhaber SZ, Tapson VF (2004) A prospective registry of 5,451 patients with ultrasound-confirmed deep vein thrombosis. Am J Cardiol 93:259–2562
Wein L, Wein S, Haas SJ, Shaw J, Krum H (2007) Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients. Arch Intern Med 14:1476–1486
Kanaan AO, Silva MA, Donovan JL, Roy T, Al-Homsi AS (2007) Meta-analysis of venous thromboembolism prophylaxis in medically ill patients. Clin Ther 29(11):2395–2405
Dentali F, Douketis JD, Gianni M, Lim W, Crowther MA (2007) Meta-analysis: anticoagulant prophylaxis to prevent symptomatic venous thromboembolism in hospitalized medical patients. Ann Intern Med 146:278–288
Geerts WH, Bergqvist D, Pineo GF et al (2008) Prevention of venous thromboembolism: American college of chest physicians evidence-based clinical practice guidelines (8th edn). Chest 133(Suppl 6):381S–453S
Duckit R, Palsson R, Bosanka L, Dagna L, Durusu Tanriover M, Vardi M et al (2010) Common diagnoses in internal medicine in Europe 2009: a pan-European, multi-centre survey. Eur J Intern Med 21(5):449–452
Cohen AT, Tapson VF, Bergmann JF, Goldhaber SZ, Kakkar AK, Deslandes B et al (2008) Venous thromboembolism risk and prophylaxis in the acute care setting (ENDORSE study): a multinational cross-sectional study. Lancet 371(9610):387–394
Anderson FA, Goldhaber SZ, Tapson VF, Bergmann JF, Kakkar AK, Deslandes B et al (2010) Improving practices in US hospitals to prevent venous thromboembolism: lessons from ENDORSE. Am J Med 123(12):1099–1106
Kucher N, Koo S, Quiroz R, Cooper JM, Paterno MD, Soukonnikov B et al (2005) Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med 352:969–977
Lederle FA, Sacks JM, Fiore L, Landefeld CS, Steinberg N, Peters RW et al (2006) The prophylaxis of medical patients for thromboembolism pilot study. Am J Med 119(1):54–59
Metlay JP, Fine MJ, Schulz R, Marrie TJ, Coley CM, Kapoor WN et al (1997) Measuring symptomatic and functional recovery in patients with community-acquired pneumonia. J Gen Intern Med 12(7):423–430
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ et al (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17(1):1–12
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
Cohen AT, Davidson BL, Gallus AS, Lassen MR, Prins MH, Tomkowski W et al (2006) Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ 332(7537):325–329
Samama MM, Cohen AT, Darmon JY, Desjardins L, Eldor A, Janbon C et al (1999) A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. N Engl J Med 341(11):793–800
Leizorovicz A, Cohen AT, Turpie AGG, Olsson CG, Vaitkus PT, Goldhaber SZ (2004) Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation 110(7):874–879
Dahan R, Houlbert D, Caulin C, Cuzin E, Viltart C, Woler M et al (1986) Prevention of deep vein thrombosis in elderly medical in-patients by a low molecular weight heparin: a randomized double-blind trial. Haemostasis 16(2):159–164
Bergmann JF, Neuhart E (1996) A multicenter randomized double-blind study of enoxaparin compared with unfractionated heparin in the prevention of venous thromboembolic disease in elderly in-patients bedridden for an acute medical illness. The Enoxaparin in Medicine Study Group. Thromb Haemost 76(4):529–534
Gussoni G, Campanini M, Silingardi M, Scannapieco G, Mazzone A, Magni G et al (2009) In-hospital symptomatic venous thromboembolism and antithrombotic prophylaxis in internal medicine. Findings from a multicenter, prospective study. Thromb Haemost 101(5):893–901
Oger E, Bressollette L, Nonent M, Lacut K, Guias B, Couturaud F et al (2002) High prevalence of asymptomatic deep vein thrombosis on admission in a medical unit among elderly patients. Thromb Haemost 88(4):592–597
Lederle FA, Zylla D, MacDonald R, Wilt TJ (2011) Venous thromboembolism prophylaxis in hospitalized medical patients and those with stroke: a background review for an American college of physicians clinical practice guideline. Ann Intern Med 155:602–615
Qaseem A, Chou R, Humphrey LL, Starkey M, Shekelle P (2011) Physicians. ftCGCotACo. Venous thromboembolism prophylaxis in hospitalized patients: a clinical practice guideline from the American college of physicians. Ann Intern Med 155:625–632
Vaitkus PT, Leizorovicz A, Cohen AT, Turpie AG, Olsson CG, Goldhaber SZ et al (2005) Mortality rates and risk factors for asymptomatic deep vein thrombosis in medical patients. Thromb Haemost 93:76–79
Engelke C, Rummeny EJ, Marten K (2006) Pulmonary embolism at multi–detector row CT of chest: one year survival of treated and untreated patients. Radiology 239(2):246–255
den Exter PL, Hooijer J, Dekkers OM, Huisman MV (2011) Risk of recurrent venous thromboembolism and mortality in patients with cancer incidentally diagnosed with pulmonary embolism: a comparison with symptomatic patients. J Clin Oncol 29(17):2405–2409
Cohen AT, Tapson VF, Bergmann JF, Goldhaber SZ, Kakkar AK, Deslandes B et al (2008) Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet 371(9610):387–394
Barbar S, Noventa F, Rossetto V, Ferrari A, Brandolin B, Perlati M et al (2010) A risk assessment model for the identification of hospitalized medical patients at risk for venous thromboembolism: the Padua prediction score. J Thromb Haemost 8:2450–2457
National Institute for Health and Clinical Excellence—venous thromboembolism: reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to hospital. Methods, evidence, and guidance: National Clinical Guideline Centre—acute and chronic conditions2010
Alikhan R, Cohen AT, Combe S, Samama MM, Desjardins L, Eldor A et al (2003) Prevention of venous thromboembolism in medical patients with enoxaparin: a subgroup analysis of the MEDENOX study. Blood Coagul Fibrinolysis 14(4):341–346
Andrade Ede O, Binda FA, Silva AM, Costa TD, Fernandes MC, Fernandes MC (2009) Risk factors and prophylaxis for venous thromboembolism in hospitals in the city of Manaus, Brazil. J Bras Pneumol 35(2):114–121
Weill-Engerer S, Meaume S, Lahlou A, Piette F, Saint-Jean O, Sachet A et al (2004) Risk factors for deep vein thrombosis in inpatients aged 65 and older: a case-control multicenter study. J Am Geriatr Soc 52(8):1299–1304
Buller HR, Cohen AT, Davidson B, Decousus H, Gallus AS, Gent M et al (2007) Extended prophylaxis of venous thromboembolism with idraparinux. N Engl J Med 357(11):1105–1112
Li XY, Fan J, Cheng YQ, Wang Y, Yao C, Zhong NS (2011) Incidence and prevention of venous thromboembolism in acutely ill hospitalized elderly Chinese. Chin Med J 124(3):335–340
Mahe I, Bergmann JF, D’Azemar P, Vaissie JJ, Caulin C (2005) Lack of effect of a low-molecular-weight heparin (nadroparin) on mortality in bedridden medical in-patients: a prospective randomised double-blind study. Eur J Clin Pharmacol 61(5–6):347–351
Bergmann JF, Neuhart E (1996) A multicenter randomized double-blind study of enoxaparin compared with unfractionated heparin in the prevention of venous thromboembolic disease in elderly in-patients bedridden for an acute medical illness. Thromb Haemost 76(4):529–534
Conflict of interest
The authors declare no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vardi, M., Steinberg, M., Haran, M. et al. Benefits versus risks of pharmacological prophylaxis to prevent symptomatic venous thromboembolism in unselected medical patients revisited. Meta-analysis of the medical literature. J Thromb Thrombolysis 34, 11–19 (2012). https://doi.org/10.1007/s11239-012-0730-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-012-0730-x