Abstract
Purpose
To discover drugs lowering PrPSc in prion-infected cultured neuronal cells that achieve high concentrations in brain to test in mouse models of prion disease and then treat people with these fatal diseases.
Methods
We tested 2-AMT analogs for EC50 and PK after a 40 mg/kg single dose and 40–210 mg/kg/day doses for 3 days. We calculated plasma and brain AUC, ratio of AUC/EC50 after dosing. We reasoned that compounds with high AUC/EC50 ratios should be good candidates going forward.
Results
We evaluated 27 2-AMTs in single-dose and 10 in 3-day PK studies, of which IND24 and IND81 were selected for testing in mouse models of prion disease. They had high concentrations in brain after oral dosing. Absolute bioavailability ranged from 27–40%. AUC/EC50 ratios after 3 days were >100 (total) and 48–113 (unbound). Stability in liver microsomes ranged from 30–>60 min. Ring hydroxylated metabolites were observed in microsomes. Neither was a substrate for the MDR1 transporter.
Conclusions
IND24 and IND81 are active in vitro and show high AUC/EC50 ratios (total and unbound) in plasma and brain. These will be evaluated in mouse models of prion disease.











Similar content being viewed by others
Abbreviations
- 2-AMT:
-
2-aminothiazole scaffold
- AUC:
-
area under the drug concentration time curve
- C3-day :
-
drug concentration after 3 days of dosing
- CJD:
-
Creutzfeldt-Jakob disease
- Cl:
-
clearance (total, intrinsic, hepatic, or otherwise)
- Cmax :
-
maximum drug concentration
- dpi:
-
days postinoculation with prions
- EC50 :
-
potency; drug concentration producing 50% of the maximal effect
- FaSSIF:
-
fasted-state simulated intestinal fluid
- HTS:
-
high-throughput screening
- IV:
-
intravenous
- MDCK-MDR1:
-
Madin Darby canine kidney cells transfected with MDR1 gene
- MDR1:
-
multidrug resistance protein 1, ATP-binding cassette sub-family B member 1
- MIC:
-
minimum inhibitory concentration
- P-gp:
-
p-glycoprotein
- PK:
-
pharmacokinetics
- PO:
-
oral
- PrPC :
-
benign normally occurring prion protein on cell surface or inside cell
- PrPSc :
-
abnormal, misfolded, pathogenic form of PrPC
- RML:
-
Rocky Mountain Laboratory
- SAR:
-
structure-activity relationship
- ScN2a-cl3:
-
scrapie (RML)-infected neuroblastoma cells that overexpress PrPC
- V:
-
volume of distribution (steady-state or otherwise)
References
Prusiner SB. Novel proteinaceous infectious particles cause scrapie. Science. 1982;216:136–44.
Weissmann C. Spongiform encephalopathies - the prion’s progress. Nature. 1991;349:569–71.
Collinge J. Prion diseases of humans and animals: their causes and molecular basis. Annu Rev Neurosci. 2001;24:519–50.
Prusiner SB. Prions and neurodegenerative diseases. N Engl J Med. 1987;317:1571–81.
Hsiao K, Baker HF, Crow TJ, Poulter M, Owen F, Terwilliger JD, et al. Linkage of a prion protein missense variant to Gerstmann-Sträussler syndrome. Nature. 1989;338:342–5.
Alpers M, Gajdusek DC. Changing patterns of kuru: epidemiological changes in the period of increasing contact of the Fore people with western civilization. Am J Trop Med Hyg. 1965;14:852–79.
Prusiner SB. Shattuck lecture — neurodegenerative diseases and prions. N Engl J Med. 2001;344:1516–26.
Frost B, Diamond MI. Prion-like mechanisms in neurodegenerative diseases. Nat Rev Neurosci. 2010;11:155–9.
Caughey B, Baron GS, Chesebro B, Jeffrey M. Getting a grip on prions: oligomers, amyloids, and pathological membrane interactions. Annu Rev Biochem. 2009;78:177–204.
DeArmond SJ, McKinley MP, Barry RA, Braunfeld MB, McColloch JR, Prusiner SB. Identification of prion amyloid filaments in scrapie-infected brain. Cell. 1985;41:221–35.
Petkova AT, Leapman RD, Guo Z, Yau WM, Mattson MP, Tycko R. Self-propagating, molecular-level polymorphism in Alzheimer’s beta-amyloid fibrils. Science. 2005;307:262–5.
Kordower JH, Chu Y, Hauser RA, Freeman TB, Olanow CW. Lewy body-like pathology in long-term embryonic nigral transplants in Parkinson’s disease. Nat Med. 2008;14:504–6.
Desplats P, Lee HJ, Bae EJ, Patrick C, Rockenstein E, Crews L, et al. Inclusion formation and neuronal cell death through neuron-to-neuron transmission of alpha-synuclein. Proc Natl Acad Sci USA. 2009;106:13010–5.
Nekooki-Machida Y, Kurosawa M, Nukina N, Ito K, Oda T, Tanaka M. Distinct conformations of in vitro and in vivo amyloids of huntingtin-exon1 show different cytotoxicity. Proc Natl Acad Sci USA. 2009;106:9679–84.
Sydow A, Mandelkow EM. ‘Prion-Like’ propagation of mouse and human tau aggregates in an inducible mouse model of tauopathy. Neurodegener Dis. 2010;7:28–31.
Caughey B, Lansbury PT. Protofibrils, pores, fibrils, and neurodegeneration: separating the responsible protein aggregates from the innocent bystanders. Annu Rev Neurosci. 2003;26:267–98.
Novitskaya V, Bocharova OV, Bronstein I, Baskakov IV. Amyloid fibrils of mammalian prion protein are highly toxic to cultured cells and primary neurons. J Biol Chem. 2006;281:13828–36.
Race RE, Fadness LH, Chesebro B. Characterization of scrapie infection in mouse neuroblastoma cells. J Gen Virol. 1987;68:1391–9.
Kocisko DA, Baron GS, Rubenstein R, Chen J, Kuizon S, Caughey B. New inhibitors of scrapie-associated prion protein formation in a library of 2000 drugs and natural products. J Virol. 2003;77:10288–94.
Kocisko DA, Caughey B, Morrey JD, Race RE. Enhanced antiscrapie effect using combination drug treatment. Antimicrob Agents Chemother. 2006;50:3447–9.
Trevitt CR, Collinge J. A systematic review of prion therapeutics in experimental models. Brain. 2006;129:2241–65.
Sim VL, Caughey B. Recent advances in prion chemotherapeutics. Infect Disord Drug Targets. 2009;9:81–91.
Korth C, May BCH, Cohen FE, Prusiner SB. Acridine and phenothiazine derivatives as pharmacotherapeutics for prion disease. Proc Natl Acad Sci USA. 2001;98:9836–41.
May BCH, Witkop J, Sherrill J, Anderson MO, Madrid PB, Zorn JA, et al. Structure-activity relationship study of 9-aminoacridine compounds in scrapie-infected neuroblastoma cells. Bioorg Med Chem Lett. 2006;16:4913–6.
Kempster S, Bate C, Williams A. Simvastatin treatment prolongs the survival of scrapie-infected mice. NeuroReport. 2007;18:479–82.
Kimata A, Nakagawa H, Ohyama R, Fukuuchi T, Ohta S, Doh-ura K, et al. New series of antiprion compounds: pyrazolone derivatives have the potent activity of inhibiting protease-resistant prion protein accumulation. J Med Chem. 2007;50:5053–6.
Thompson MJ, Borsenberger V, Louth JC, Judd KE, Chen B. Design, synthesis, and structure–activity relationship of indole-3-glyoxylamide libraries possessing highly potent activity in a cell line model of prion disease. J Med Chem. 2009;52:7503–11.
Kawasaki Y, Kawagoe K, Chen CJ, Teruya K, Sakasegawa Y, Doh-ura K. Orally administered amyloidophilic compound is effective in prolonging the incubation periods of animals cerebrally infected with prion diseases in a prion strain-dependent manner. J Virol. 2007;81:12889–98.
Supattapone S, Wille H, Uyechi L, Safar J, Tremblay P, Szoka FC, et al. Branched polyamines cure prion-infected neuroblastoma cells. J Virol. 2001;75:3453–61.
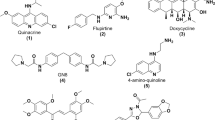
Ghaemmaghami S, May BCH, Renslo AR, Prusiner SB. Discovery of 2-aminothiazoles as potent antiprion compounds. J Virol. 2010;84:3408–12.
Gallardo-Godoy A, Gever J, Fife KL, Silber BM, Prusiner SB, Renslo AR. 2-Aminothiazoles as therapeutic leads for prion diseases. J Med Chem. 2011;54:1010–21.
Craig WA. The role of pharmacodynamics in effective treatment of community-acquired pathogens. Johns Hopkins Adv Stud Med. 2002;2:126–34.
Ambrose PG, Bhavnani SM, Rubino CM, Louie A, Gumbo T, Forrest A, et al. Pharmacokinetics-pharmacodynamics of antimicrobial therapy: it’s not just for mice anymore. Clin Infect Dis. 2007;44:79–86.
Jonen HG, Werringloer J, Prough RA, Estabrook RW. The reaction of phenylhydrazine with microsomal cytochrome P-450. Catalysis of heme modification. J Biol Chem. 1982;257:4404–11.
Ghaemmaghami S, Ullman J, Ahn M, St. Martin S, Prusiner SB. Chemical induction of misfolded prion protein conformers in cell culture. J Biol Chem. 2010;285:10415–23.
Obach RS. Prediction of human clearance of twenty-nine drugs from hepatic microsomal intrinsic clearance data: an examination of in vitro half-life approach and nonspecific binding to microsomes. Drug Metab Dispos. 1999;27:1350–9.
Hilgers AR, Conradi RA, Burton PS. Caco-2 cell monolayers as a model for drug transport across the intestinal mucosa. Pharm Res. 1990;7:902–10.
Kalvass JC, Maurer TS. Influence of nonspecific brain and plasma binding on CNS exposure: implications for rational drug discovery. Biopharm Drug Dispos. 2002;23:327–38.
Gibaldi M, Perrier D. Pharmacokinetics. 2nd ed. New York: Marcel Dekker, Inc; 1982.
Ha-Duong NT, Dijols S, Macherey AC, Goldstein JA, Dansette PM, Mansuy D. Ticlopidine as a selective mechanism-based inhibitor of human cytochrome P450 2C19. Biochemistry. 2001;40:12112–22.
Korth C, Kaneko K, Groth D, Heye N, Telling G, Mastrianni J, et al. Abbreviated incubation times for human prions in mice expressing a chimeric mouse–human prion protein transgene. Proc Natl Acad Sci USA. 2003;100:4784–9.
Ghaemmaghami S, Ahn M, Lessard P, Giles K, Legname G, DeArmond SJ, et al. Continuous quinacrine treatment results in the formation of drug-resistant prions. PLoS Pathog. 2009;5:e1000673.
Acknowledgments AND DISCLOSURES
The authors thank Ms. Ana Serban, Ms. Julia Becker, and Mr. Frederic Letessier for D13 and D18 antibodies; Mr. Phillip Benner and the staff of the Hunter’s Point animal facility for expert animal studies; Dr. Sina Ghaemmaghami for many helpful discussions; and Ms. Hang Nguyen for editorial assistance. This work was supported by grants from the National Institutes of Health (AG002132, AG010770, AG031220, and AG021601) as well as by gifts from the Sherman Fairchild Foundation, Rainwater Charitable Foundation, Lincy Foundation, Fight for Mike Homer Program, and Robert Galvin. MPJ is a consultant to Schrodinger LLC.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 97 kb)
Rights and permissions
About this article
Cite this article
Silber, B.M., Rao, S., Fife, K.L. et al. Pharmacokinetics and Metabolism of 2-Aminothiazoles with Antiprion Activity in Mice. Pharm Res 30, 932–950 (2013). https://doi.org/10.1007/s11095-012-0912-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-012-0912-4