Abstract
To identify maternal, care provider, and institutional-level risk factors for early term (37–38 weeks) elective repeat cesarean delivery in a population-based cohort. Retrospective cohort study of women in the British Columbia (BC) Perinatal Data Registry, BC, Canada, 2008–2011, with an elective repeat cesarean delivery at term. Absolute percent differences (risk differences) in early term delivery rates were calculated according to maternal characteristics, type of care provider, calendar time (day of the week, time of year), and annual institutional obstetrical volume. Of the 7,687 elective repeat cesareans at term in BC, 55 % occurred before 39 + 0 weeks. Early term delivery was significantly more common with multiple previous cesareans [8.2 percentage points (95 % CI 5.5, 10.9) for 2 previous cesareans, 11.3 (95 % CI 5.1, 17.4) for 3 or more previous cesareans], obesity [6.7 percentage points (95 % CI 1.6, 11.7)], and a hospital obstetrical volume <2,500 deliveries per year. Type of care provider and calendar time were not significant risk factors for early term delivery. Early term elective repeat cesarean was common across a wide range of maternal, care provider, and institutional characteristics, suggesting that most obstetrical care settings would benefit from quality-improvement programs to reduce elective repeat cesarean deliveries before 39 weeks. A better understanding of the risks and benefits of early term delivery among obese women and women with multiple previous cesareans is needed given the higher rates of early term delivery observed in these women.
Similar content being viewed by others
Introduction
As a result of the rising rate of primary cesarean birth, elective (planned) repeat cesareans now account for close to 15 percent of cesarean deliveries performed in the United States [1]. For women undergoing an elective repeat cesarean, the gestational age at which the cesarean delivery is performed is an important healthcare quality indicator [2]. As risks of serious neonatal respiratory complications are significantly higher at early term ages (37–38 weeks) compared with late term ages (39–41 weeks) [3–8], clinical practice guidelines state that elective cesareans should not be scheduled before 39 weeks unless documented evidence of fetal lung maturity exists [9, 10]. Recent evidence suggests that even infants with documented fetal lung maturity at 36–38 weeks are at increased risk of respiratory morbidity compared with infants born at 39–40 weeks [11].
Despite evidence and clinical practice guidelines advocating against early term delivery, several studies suggest that elective repeat cesareans may commonly be performed before 39 weeks. A study from the National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network, a collaboration of 19 US academic centres, reported that 35.8 % of elective repeat cesareans were performed before 39 weeks [4]. Similarly, the Aarhus University Hospital in Denmark and a study from the Netherlands found that over 50 % of elective cesareans (for any indication) occurred at 37 or 38 weeks [3, 7]. These findings are concerning, given the increased burden of preventable serious neonatal complications this practice is believed to cause.
Our understanding of the reasons why current practice in timing of elective repeat cesarean delivery appears to be at odds with clinical guidelines is limited. Although often attributed to physician convenience or women’s desire to deliver once term has been reached, the extent to which patterns of early term elective repeat cesarean are influenced by maternal, care-provider, or institutional-level factors has not been well studied. In order to best target initiatives to reduce the number of elective repeat cesareans performed before 39 weeks, an understanding of current patterns of early term deliveries is needed. The primary goal of this study was to identify patient-, care giver-, and institutional-level risk factors for early term elective repeat cesarean delivery in a large, population-based cohort in British Columbia (BC), Canada.
Methods
Study Population
An analysis of birth records in the BC Perinatal Database Registry (BCPDR) between April 1, 2008 and March 31, 2011 was performed. The BCPDR is a quality-controlled database maintained by the provincial government agency Perinatal Services BC, and contains obstetrical and neonatal medical chart records on >98 % of births in the province [12]. Data quality is maintained by checks in the data entry software program, year-end checks and reports, and ongoing quality checks. The BCPDR contains over 130,000 birth records from 2008 to 2011. The study was approved by the Research Ethics Board of the BC Children’s & Women’s Hospital (CW11-0190/H11-01827).
The study population was restricted to women with a previous cesarean delivery who delivered a singleton, term (37 + 0 to 41 + 6 weeks) infant by cesarean delivery for a primary indication of “Repeat cesarean” or “VBAC declined/Maternal request”. In British Columbia, over 70 % of women with a singleton, cephalic fetus have a planned repeat cesarean delivery [13]. The indications for cesarean are obtained from the physician’s notes or the Labour & Birth Summary, which is a provincially-standardized form completed by the physician, nurse, or midwife. We further excluded pregnancies with documented comorbidities that may have influenced planned timing of delivery (suspected intrauterine growth restriction, maternal pre-existing or gestational diabetes, hypertension in pregnancy, cardiac disease, or renal disease), and women who presented in labour or with ruptured membranes prior to the cesarean. Stillbirths and pregnancies with congenital anomalies were also excluded.
Variables
Gestational age was calculated using the Society of Obstetricians and Gynecologists of Canada algorithm [14] in which gestational age is estimated using last menstrual period if it agrees with early ultrasound (within 5 days if ultrasound performed <14 weeks, 7 days if ultrasound performed 14–17 weeks, and 10 days if ultrasound performed 18–20 weeks) and the early ultrasound estimate is used otherwise. Early term was defined as a birth at 37 + 0 to 38 + 6 weeks, while late term was defined as a birth at 39 + 0 to 41 + 6 weeks.
Maternal level risk factors evaluated for a potential association with early term delivery included the number of previous cesarean deliveries (1, 2, 3 or more), maternal age (years), and maternal pre-pregnancy body mass index (BMI), categorized as underweight (BMI < 18.5 kg/m2), normal weight (BMI 18.5–24.9 kg/m2), overweight (BMI 25–29.9 kg/m2), and obese (BMI ≥ 30 kg/m2). Maternal heights and pre-pregnancy weights in the BCPDR can be either self-reported or measured at the time of a clinic visit. A maternal weight measured before 12 weeks’ gestation is accepted in the absence of a pre-pregnancy weight.
Type of health care provider was based on the individual who delivered the baby, classified as obstetrician/gynecologist, family doctor, or general surgeon. In British Columbia, family doctors and general surgeons (with additional training in cesarean sections) can perform cesarean deliveries, typically serving smaller centers with limited access to specialist obstetrical services. Hospital delivery volume was classified based on the total number of deliveries occurring at each institution on an annual basis, categorized as fewer than 500, 500–999, 1,000–1,499, 1,500–2,499, or ≥2,500 deliveries. We hypothesized that early term deliveries may be more likely immediately prior to a weekend or times of increased staff vacations, so variables indicating a Thursday or Friday delivery or a delivery during the summer months of July or August were created.
Statistical Analyses
The risk of early term delivery was defined as the number of cesarean deliveries performed at early term ages divided by the total number of cesarean deliveries at term. The overall risk of early term delivery was calculated with a 95 % CI. As early term delivery was not a rare outcome, risk factors for early term delivery were assessed using risk differences (RD) (i.e., the absolute difference in percentage points between groups in early term delivery rates) rather than odds ratios. Unlike calculation of odds ratio, this approach produces unbiased estimates of average risk with a common outcome when adjusted for covariates [15, 16]. A multivariable generalized linear model that simultaneously adjusted for other maternal and institutional determinants was built to identify independent risk factors for early term delivery. In this adjusted model, multiple imputation was used to retain women with missing pre-pregnancy BMI [17]. Missing heights and pre-pregnancy weights were imputed (to maximize the use of recorded data), then BMI was derived from these values. As recommended [17], we included the outcome variable (early term delivery) as well as other maternal, fetal, and institutional characteristics in our imputation models. Ten imputed datasets were created, and summary results produced using STATA SE version 11’s.mi estimate (College Station, TX, USA).
Results
A total of 12,406 women who delivered a singleton, term birth following a repeat cesarean delivery with a primary indication of ‘repeat cesarean’ or ‘VBAC declined/maternal request’ were eligible for inclusion. Excluding pregnancies with comorbidities (n = 1,878), pre-cesarean labour (n = 1,519) or rupture of membranes (n = 990) and infants with anomalies (n = 332) left 7,687 pregnancies for analysis. In our study population, the average (SD) maternal age was 33 years (5.0) and average pre-pregnancy BMI 25.6 kg/m2 (5.8). Seventy-one percent (71 %) of women had a parity of 1, 23.3 % had a parity of 2, and 5.6 % had a parity of 3 or higher. The average birth weight was 3,490 grams (437).
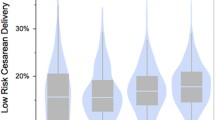
In British Columbia, 55 % of elective repeat cesarean deliveries (95 % CI 54, 56 %) were performed at early term ages (4,199/7,687). As shown in Fig. 1, the majority of these early term deliveries occurred at 38 weeks. In Table 1, the risk of elective repeat cesareans performed at early term delivery is shown according to maternal, care giver, and institutional characteristics, while the corresponding differences in percentage points between categories (i.e., the absolute risk difference) are shown in Figs. 2 and 3, both crude and after adjusting for confounders. The figures show the increased or decreased risk in each category as compared with the reference categories of: one previous cesarean (number of previous cesareans), maternal age 20–24 (maternal age), and pre-pregnancy body mass index 18.5–24.9 kg/m2 (BMI), obstetrician/gynecologist (type of care provider), ≥2,500 deliveries (obstetrical volume),and times other than July/August or Thursday/Friday delivery (calendar time).
Differences in risk of early term elective repeat cesarean delivery according to maternal characteristics in British Columbia, Canada, 2008–2011, compared with the reference groups of 1 previous cesarean (number of previous cesareans), maternal age 20–24 (maternal age), and pre-pregnancy body mass index 18.5–24.9 kg/m2 (BMI). Multiple imputation was used to address missing pre-pregnancy BMI values
Differences in risk of early term elective repeat cesarean delivery according to institutional and care provider characteristics in British Columbia, Canada, 2008–2011, compared with the reference groups of obstetrician/gynecologist (type of care provider), ≥2,500 deliveries (obstetrical volume),and times other than July/August or Thursday/Friday delivery (calendar time). Multiple imputation was used to address missing pre-pregnancy BMI values
The risk of early term delivery was higher among women with a greater number of previous cesareans. Compared with women with a single previous cesarean, women with two previous cesareans had a risk of early term delivery that was nine percentage points higher [RD = 8.9 (95 % CI 6.2, 11.6), reflecting crude risks of 61 vs. 52 %]. Adjustment for other maternal and institutional characteristics had minimal impact on this risk factor [adjusted RD = 8.2 (95 % CI 5.5, 11.0)]. The risk of early term delivery was even higher among women with three or more previous cesareans, with an estimated risk 11.3 percentage points higher than women with only a single previous cesarean (95 % CI 5.1, 17.4) after adjusting for potential confounders.
Maternal age was not a strong risk factor for early term delivery. Although women under 25 were less likely to have an early term repeat cesarean delivery than women aged 25–29 [adjusted RD = −6.1 (−10.7, −1.5)], no significant differences were seen in women aged 30–34, 35–39, or older than 40 years compared with women aged 25–29. There were no significant differences in the risks of early term delivery in underweight or overweight women compared with normal weight women, but among obese women, the risk of early term delivery was significantly higher than in normal weight women [crude risks of 61 % among obese women and 54 % among normal weight women; adjusted risk difference of 6.7 (95 % 1.6, 11.7)].
Risks of early term delivery varied significantly according to hospital obstetrical volume. In hospitals with an obstetrical volume of 2,500 or more deliveries per year, 50.3 % of elective repeat cesareans were performed at early term ages, compared with rates close to 60 % in hospitals with fewer than 1,500 deliveries per year. These differences remained significant after adjusting for differences in maternal and care giver characteristics between sites. Risks of early term delivery did not differ between obstetrician/gynecologists, family doctors, and general surgeons. We also found no evidence to suggest that scheduling issues influenced rates of early term delivery. Rates of early term delivery on Thursdays or Fridays and during summer months were not significantly different than at other times.
Sensitivity analyses using a Huber-White sandwich estimator to account for the potential correlation from inclusion of repeated pregnancies in our population produced virtually identical results (data available upon request). We also obtained similar results when multivariable models were restricted to women with documented BMI (i.e., excluding women with missing BMI), with the exception of the estimate for hospitals with 1,500–2,499 births, which was attenuated and no longer statistically significant [RD = 0.4 (−3.3, 4.1)].
Discussion
Despite the known risks of elective delivery before 39 weeks’ gestation, this study found that in a large population-based cohort, 55 % of term elective repeat cesarean deliveries were performed at 37 or 38 weeks. Women with multiple previous cesareans, obese women, and women delivering in medium–low obstetrical volume hospital were at elevated risk of early term delivery.
A study from the Netherlands reported that women with elective cesareans before 39 weeks were more likely to be older, of Western origin, and multiparous [7]. We found that younger maternal age (<25) was associated with a lower rate of early term delivery, but rates were not significantly higher among women of advanced age. The higher rate of early term delivery among multiparous women in the Dutch study agrees with our finding that women with multiple previous cesareans were significantly more likely to have an early term delivery, as these two factors are likely highly correlated. We additionally found that obese women were more likely to have an early term delivery. Taken together, these results suggest that concerns over potential obstetrical complications associated with delayed delivery (such as the increased risk of stillbirth among obese women [18], increased difficulties associated with performing an emergent cesarean for an obese women, or increased risk of uterine rupture among women with multiple cesarean scars following onset of spontaneous labour [19] may be important factors behind the high rates of early term elective cesareans in these groups. As with all clinical practice guidelines, guidelines on timing of repeat cesarean delivery are intended to promote best practice for the population of women undergoing a repeat cesarean delivery, but should not replace clinical judgment. Consideration of available resources and each woman’s individual circumstances is critical for identifying exceptional cases where delaying delivery until 39 weeks may not be appropriate. Research to quantify the risks and benefits of early term delivery in these groups of women would be valuable in determining whether obesity and multiple previous cesareans should be considered to be indications for early term delivery.
Several explanations for our finding that the risk of early term delivery was lowest in high volume hospitals are possible. As preliminary evidence suggests that hospital policies to delay elective cesarean delivery until 39 weeks may increase the probability that a woman will go into spontaneous labour prior to her scheduled surgery date and require an emergency-timing cesarean [20], the lower rate at high volume hospitals may reflect increased confidence and/or ability to perform emergency-timing cesareans and manage potential complications arising from pre-cesarean labour as a result of better access to specialist services (obstetrics, anesthesia). Alternatively, performing a higher volume of elective repeat cesareans may create more of an incentive to develop and implement specific policies to reduce deliveries before 39 weeks.
We are unaware of other studies that have examined if patterns of early term elective cesarean delivery differ according to care-giver or institutional factors. Although we had hypothesized that scheduling issues (such as times of high staff vacation or wish to avoid a weekend delivery) may be an important reason why deliveries were performed before 39 weeks, our hypothesis was not supported by our data. Likewise, rates of early term delivery did not differ according to the type of care provider.
Strengths of this study include its use of a database that contains a representative, population-based study sample with detailed obstetrical and neonatal medical chart information. Our population-based sample means that results are generalizable to women who deliver outside tertiary care teaching hospitals (where much of the work on timing of elective cesarean delivery has previously been done) [3, 4], and we were additionally able to examine the influence of factors such as hospital obstetrical volume on rates of early term delivery.
Although we excluded women with documented comorbid conditions and pregnancies with suspected intrauterine growth restriction, a portion of the elective repeat cesareans at early term gestation could have been precipitated by additional medical or obstetrical indications not included in our database. Further, documentation of risk factors in the medical chart may have been lacking for some women, resulting in a true indication for early term delivery. Nevertheless, given that undocumented or additional comorbidities likely only constitute a small fraction of the population of women undergoing a term repeat cesarean delivery (documented comorbities accounted for 15 percent of our total population, and we speculate that undocumented comorbidities are less common than this), and that early term delivery was very common on our population (55 percent), such cases are unlikely to explain away the observed rate of early term delivery. We also did not have data on the type of incision used in the previous cesarean, which may be an important determinant of timing of delivery. Further work to understand the role of this potential risk factor would be valuable.
Conclusions
Although early term elective repeat cesarean delivery was most common among women with multiple previous cesareans, obese women, and women delivering in small or mid volume hospitals, the risk of early term delivery was high even in non-obese women with a single previous cesarean delivering in high volume hospitals. Given the large numbers of planned repeat cesarean deliveries performed each year in British Columbia and elsewhere, the high rates of early term delivery in this group could have an important impact on the burden of neonatal respiratory morbidity at the population level. Initiatives to reduce the number of repeat cesarean deliveries performed before 39 weeks appear to be needed in most obstetrical care settings, rather than only in certain institution types, care providers, or groups of women. Higher rates of early term delivery among obese women and women with multiple previous cesareans suggest that practice guidelines should clarify whether obesity and multiple previous cesareans are possible indications for an early term delivery.
References
Barber, E. L., Lundsberg, L. S., Belanger, K., Pettker, C. M., Funai, E. F., & Illuzzi, J. L. (2011). Indications contributing to the increasing cesarean delivery rate. Obstetrics and Gynecology, 118, 29–38.
Joint Commission National Quality Measures. (2011). Specifications manual for joint commission national quality measures (v2011A). Available from: http://manual.jointcommission.org/releases/TJC2011A/PerinatalCare.html.
Hansen, A. K., Wisborg, K., Uldbjerg, N., & Henriksen, T. B. (2008). Risk of respiratory morbidity in term infants delivered by elective cesarean section: cohort study. British Medical Journal, 336, 85–87.
Tita, A. T., Landon, M. B., Spong, C. Y., Lai, Y., Leveno, K. J., Varner, M. W., et al. (2009). Timing of elective repeat cesarean delivery at term and neonatal outcomes. New England Journal of Medicine, 360, 111–120.
Morrison, J. J., Rennie, J. M., & Milton, P. J. (1995). Neonatal respiratory morbidity and mode of delivery at term: Influence of timing of elective cesarean section. British Journal of Obstetrics and Gynaecology, 102, 101–106.
Oshiro, B. T., Henry, E., Wilson, J., Branch, D. W., & Varner, M. W. (2009). Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstetrics and Gynecology, 113, 804–811.
Wilmink, F. A., Hukkelhoven, C. W., Lunshof, S., Mol, B. W., & van der Post, J. A. (2010). Papatsonis DN. Neonatal outcome following elective cesarean section beyond 37 weeks of gestation: A 7-year retrospective analysis of a national registry. American Journal of Obstetrics and Gynecology, 202, 250 e1–250 e8.
Yee, W., Amin, H., & Wood, S. (2008). Elective cesarean delivery, neonatal intensive care unit admission, and neonatal respiratory distress. Obstetrics and Gynecology, 111, 823–828.
American College of Obstetricians and Gynecologists. (2007). ACOG Committee Opinion No. 394, December 2007. Cesarean delivery on maternal request. Obstetrics and Gynecology 110, 1501.
American College of Obstetricians and Gynecologists. (1992). Fetal maturity assessment prior to elective repeat cesarean delivery. International Journal of Gynaecology and Obstetrics, 38, 327.
Bates, E., Rouse, D. J., Mann, M. L., Chapman, V., Carlo, W. A., & Tita, A. T. (2010). Neonatal outcomes after demonstrated fetal lung maturity before 39 weeks of gestation. Obstetrics and Gynecology, 116, 1288–1295.
British Columbia Reproductive Care Program. (2003). British Columbia perinatal database registry overview, Vancouver.
Perinatal Services British Columbia. (2011). Pregnancy outcomes of women with a previous cesarean delivery in British Columbia, Canada, 2001–2010, Perinatal Services BC Surveillance Special Report, Vancouver, Canada.
Delaney, M., Roggensack, A., Leduc, D. C., Ballermann, C., Biringer, A., Delaney, M., et al. (2008). Guidelines for the management of pregnancy at 41 + 0 to 42 + 0 weeks. Journal of Obstetrics and Gynaecology Canada, 30, 800–823.
Axelson, O., Fredriksson, M., & Ekberg, K. (1994). Use of the prevalence ratio v the prevalence odds ratio as a measure of risk in cross sectional studies. Occupational and Environmental Medicine, 51, 574.
Greenland, S. (1987). Interpretation and choice of effect measures in epidemiologic analyses. American Journal of Epidemiology, 125, 761–768.
Sterne, J. A., White, I. R., Carlin, J. B., Spratt, M., Royston, P., Kenward, M. G., et al. (2009). Multiple imputation for missing data in epidemiological and clinical research: Potential and pitfalls. British Medical Journal, 338, b2393.
Salihu, H. M., Dunlop, A. L., Hedayatzadeh, M., Alio, A. P., Kirby, R. S., & Alexander, G. R. (2007). Extreme obesity and risk of stillbirth among black and white gravidas. Obstetrics and Gynecology, 110, 552–557.
Caughey, A. B., Shipp, T. D., Repke, J. T., Zelop, C. M., Cohen, A., & Lieberman, E. (1999). Rate of uterine rupture during a trial of labor in women with one or two prior cesarean deliveries. American Journal of Obstetrics and Gynecology, 181, 872–876.
Hutcheon, J. A. et al. (2012). Maternal and neonatal risks following emergency-timing repeat cesarean delivery (abstract). In Proceedings of the 25th annual meeting of the society for paediatric and perinatal epidemiology. Minneapolis, MN.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this license, visit (http://creativecommons.org/licenses/by-nc-nd/2.0/)
About this article
Cite this article
Hutcheon, J.A., Joseph, K.S., Kinniburgh, B. et al. Maternal, Care Provider, and Institutional-Level Risk Factors for Early Term Elective Repeat Cesarean Delivery: A Population-Based Cohort Study. Matern Child Health J 18, 22–28 (2014). https://doi.org/10.1007/s10995-013-1229-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-013-1229-6