Abstract
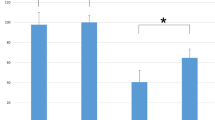
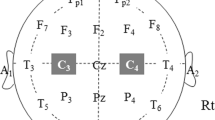
Objective. Transcranial Motor Evoked Poten- tials (TcMEPs) are sometimes used during lumbar spine surgery in order to detect and prevent an intraoperative nerve root injury. Typically, a fixed stimulus is applied, and one monitors for changes in response amplitude from several myotomes. Increased stimulating voltage may or may not alter the response after an acute injury. Methods. We suture ligated the dominant root innervating the tibialis anterior (TA) muscle in 7 experiments in swine monitored with TcMEPs. Injury to the root was confirmed by an increase in threshold current needed to evoke an EMG response in the TA (from 0.32 ± 0.10 to 2.3 ± 0.9 mA, P < 0.01). We recorded TcMEPs at baseline, after injury, and with incremental 25 V increases in stimulation up to 100 V. Results. After ligation, mean TcMEP amplitude in the TA decreased by 56% from baseline (P < 0.01). Adding voltage progressively restored mean amplitude to within 17% of baseline, but with wide variability in the response. In 1 experiment, there was no augmentation; 3 studies showed partial improvement toward baseline; and in 3 studies, the amplitude was augmented to levels above baseline. Conclusion. An acute nerve root injury may be detected by TcMEP monitoring. However, if the stimulating voltage is increased after injury, the response may or may not be affected. In complex spine procedures, adjustments to TcMEP stimulating parameters are often needed to maintain reproducible responses. However, if these changes are made during a period where injury might occur, this could mask the changes and lead to a false-negative interpretation.
Similar content being viewed by others
References
Pelosi L, Stevenson M, Hobbs GJ, Jardine A, Webb JK. Intraoperative motor evoked potentials to transcranial electrical stimulation during two anaesthetic regimens. Clin Neurophysiol. 2001;112:1076–87.
MacDonald DB, Al Zayed Z, Khoudeir I, Stigsby B. Monitoring scoliosis surgery with combined multiple pulse transcranial electric motor and cortical somatosensory-evoked potentials from the lower and upper extremities. Spine. 2003;28:194–203.
Calancie B, Harris W, Broton JG, Alexeeva N, Green BA. “Threshold-level” multipulse transcranial electrical stimulation of motor cortex for intraoperative monitoring of spinal motor tracts: description of method and comparison to somatosensory evoked potential monitoring. J Neurosurg. 1998;88:457–70.
Calancie B, Molano MR. Alarm criteria for motor-evoked potentials: what’s wrong with the “presence-or-absence” approach? Spine (Phila Pa 1976). 2008;33:406–14.
Langeloo DD, Lelivelt A, Louis Journee H, Slappendel R, de Kleuver M. Transcranial electrical motor-evoked potential monitoring during surgery for spinal deformity: a study of 145 patients. Spine (Phila Pa 1976). 2003;28:1043–50.
Sutter M, Eggspuehler A, Muller A, Dvorak J. Multimodal intraoperative monitoring: an overview and proposal of methodology based on 1, 017 cases. Eur Spine J. 2007;16(Suppl 2):S153–61.
Fan D, Schwartz DM, Vaccaro AR, Hilibrand AS, Albert TJ. Intraoperative neurophysiologic detection of iatrogenic C5 nerve root injury during laminectomy for cervical compression myelopathy. Spine (Phila Pa 1976). 2002;27:2499–502.
Lieberman JA, Lyon R, Feiner J, Hu SS, Berven SH. The efficacy of motor evoked potentials in fixed sagittal imbalance deformity correction surgery. Spine (Phila Pa 1976). 2008;33:E414–24.
Lyon R, Feiner J, Lieberman JA. Progressive suppression of motor evoked potentials during general anesthesia: the phenomenon of “anesthetic fade”. J Neurosurg Anesthesiol. 2005;17:13–9.
Mok JM, Lyon R, Lieberman JA, Cloyd JM, Burch S. Monitoring of nerve root injury using transcranial motor-evoked potentials in a pig model. Spine (Phila Pa 1976). 2008;33:E465–73.
Santiago-Perez S, Nevado-Estevez R, Aguirre-Arribas J, Perez-Conde MC. Neurophysiological monitoring of lumbosacral spinal roots during spinal surgery: continuous intraoperative electromyography (EMG). Electromyogr Clin Neurophysiol. 2007;47:361–7.
Quinones-Hinojosa A, Lyon R, Zada G, Lamborn KR, Gupta N, Parsa AT, McDermott MW, Weinstein PR. Changes in transcranial motor evoked potentials during intramedullary spinal cord tumor resection correlate with postoperative motor function. Neurosurgery 2005;56:982–93 (discussion-93).
Matsui H, Kanamori M, Kawaguchi Y, Kitagawa H, Nakamura H, Tsuji H. Clinical and electrophysiologic characteristics of compressed lumbar nerve roots. Spine (Phila Pa 1976). 1997;22:2100–5.
Lyon R, Lieberman JA, Feiner J, Burch S. Relative efficacy of transcranial motor evoked potentials, mechanically-elicited electromyography, and evoked EMG to assess nerve root function during sustained retraction in a porcine model. Spine (Phila Pa 1976). 2009;34:E558–64.
Liguori R, Krarup C, Trojaborg W. Determination of the segmental sensory and motor innervation of the lumbosacral spinal nerves. An electrophysiological study. Brain. 1992;115(Pt 3):915–34.
Mangun GR, Mulkey RM, Young BL, Goslow GE Jr. “Cross-talk” in electromyograms: contamination of EMGs recorded with bipolar fine-wire electrodes by volume conducted myoelectric activity from distant sources. Electromyogr Clin Neurophysiol. 1986;26:443–61.
Aminoff MJ, Goodin DS, Barbaro NM, Weinstein PR, Rosenblum ML. Dermatomal somatosensory evoked potentials in unilateral lumbosacral radiculopathy. Ann Neurol. 1985;17:171–6.
Tsai TM, Tsai CL, Lin TS, Lin CC, Jou IM. Value of dermatomal somatosensory evoked potentials in detecting acute nerve root injury: an experimental study with special emphasis on stimulus intensity. Spine (Phila Pa 1976). 2005;30:E540–6.
Kim DH, Zaremski J, Kwon B, Jenis L, Woodard E, Bode R, Banco RJ. Risk factors for false positive transcranial motor evoked potential monitoring alerts during surgical treatment of cervical myelopathy. Spine (Phila Pa 1976). 2007;32:3041–6.
Resnick DK, Anderson PA, Kaiser MG, Groff MW, Heary RF, Holly LT, Mummaneni PV, Ryken TC, Choudhri TF, Vresilovic EJ, Matz PG. Electrophysiological monitoring during surgery for cervical degenerative myelopathy and radiculopathy. J Neurosurg Spine. 2009;11:245–52.
Krammer MJ, Wolf S, Schul DB, Gerstner W, Lumenta CB. Significance of intraoperative motor function monitoring using transcranial electrical motor evoked potentials (MEP) in patients with spinal and cranial lesions near the motor pathways. Br J Neurosurg. 2009;23:48–55.
Author information
Authors and Affiliations
Corresponding author
Additional information
Lyon R, Gibson A, Burch S, Lieberman J. Increases in voltage may produce false-negatives when using transcranial motor evoked potentials to detect an isolated nerve root injury.
Rights and permissions
About this article
Cite this article
Lyon, R., Gibson, A., Burch, S. et al. Increases in voltage may produce false-negatives when using transcranial motor evoked potentials to detect an isolated nerve root injury. J Clin Monit Comput 24, 441–448 (2010). https://doi.org/10.1007/s10877-010-9269-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-010-9269-6