Abstract
Background
Hyper-immunoglobulin E recurrent infection syndromes (HIES) has characteristic features and identified mutations. This study investigated clinical features and causal candidate mutations in Taiwanese patients with the HIES phenotype on referral base over 23 million inhabitants.
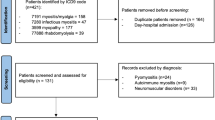
Patients and Methods
Clinical manifestations of the HIES phenotype, severity scoring, immunological functions and candidate genes of signal transducer and activator of transcription 3 (STAT3), tyrosine kinase 2 (TYKZ), and dedicator of cytokineses 8 (DOCK8) were analyzed.
Results
Between 1985 and 2009, six sporadic and two siblings met HIES criteria (onset age: 2–54 months; severity score: 31–65) out of 187 patients with primary immunodeficiencies. Five patients with the autosomal dominant (AD)-HIES phenotype presented as pneumatocoele, bronchiectasis, retained primary teeth, minor trauma fracture, scoliosis, coronary aneurysm, and lymphoma. Three with the autosomal recessive (AR)-HIES phenotype and impaired lymphocyte proliferation function had herpes simplex virus infection, molluscum contagiosum, and cerebral vasculitis. Notably in one patient with the AR-HIES phenotype, unintentional lead component in traditional application herbs for accelerating wound healing deposited in basal ganglia and aggravated involuntary movement relative to cerebral vacculitis. Those with mildly elevated memory T cells and decreased memory B cells trended to develop arteritis. Of five AD-HIES patients, three were mortalities from acute myocardial infarction, Proteus mirabilis, and Staphylococcus aureus sepsis. Only one had de novo novel STAT3 (Gln 469 Arg) mutation with “relative” lower HIES STAT3 score.
Conclusions
Known genetic defects responsible for the HIES phenotype are not so common in Taiwan. This may infer genetic variations in different ethnicities although selection bias and under-diagnosis for HIES with known genetic defects could be contribution factors.




Similar content being viewed by others
References
Grimbacher B, Holland SM, Gallin JI, Greenberg F, Hill SC, Malech HL, et al. Hyper-IgE syndrome with recurrent infections—an autosomal dominant multisystem disorder. N Engl J Med. 1999;340:692–702.
Renner ED, Puck JM, Holland SM, Schmitt M, Weiss M, Frosch M, et al. Autosomal recessive hyperimmunoglobulin E syndrome: a distinct disease entity. J Pediatr. 2004;144:93–9.
Minegishi Y, Saito M, Morio T, Watanabe K, Agematsu K, Tsuchiya S, et al. Human tyrosine kinase 2 deficiency reveals its requisite roles in multiple cytokine signals involved in innate and acquired immunity. Immunity. 2006;25:745–55.
Davis SD, Schaller J, Wedgwood RJ. Job’s syndrome. Recurrent, “cold”, staphylococcal abscesses. Lancet. 1966;1:1013–5.
Buckley RH, Wray BB, Belmaker EZ. Extreme hyperimmunoglobulinemia E and undue susceptibility to infection. Pediatrics. 1972;49:59–70.
Renner ED, Torgerson TR, Rylaarsdam S, Añover-Sombke S, Golob K, LaFlam T, et al. STAT3 mutation in the original patient with Job’s syndrome. N Engl J Med. 2007;357:1667–8.
Minegishi Y, Saito M, Tsuchiya S, Tsuge I, Takada H, Hara T, et al. Dominant-negative mutations in the DNA-binding domain of STAT3 cause hyper-IgE syndrome. Nature. 2007;448:1058–62.
Holland SM, DeLeo FR, Elloumi HZ, Hsu AP, Uzel G, Brodsky N, et al. STAT3 mutations in the hyper-IgE syndrome. N Engl J Med. 2007;357:1608–919.
Minegishi Y. Hyper-IgE syndrome. Curr Opin Immunol. 2009;21:487–92.
Zhang Q, Davis JC, Lamborn IT, Freeman AF, Jing H, Favreau AJ, et al. Combined immunodeficiency associated with DOCK8 mutations. N Engl J Med. 2009;361:2046–55.
Engelhardt KR, McGhee S, Winkler S, Sassi A, Woellner C, Lopez-Herrera G, et al. Large deletions and point mutations involving the dedicator of cytokinesis 8 (DOCK8) in the autosomal-recessive form of hyper-IgE syndrome. J Allergy Clin Immunol. 2009;124:1289–302.
Minegishi Y, Karasuyama H. Defects in Jak-STAT-mediated cytokine signals cause hyper-IgE syndrome: lessons from a primary immunodeficiency. Int Immunol. 2009;21:105–12.
Grimbacher B, Schäffer AA, Holland SM, Davis J, Gallin JI, Malech HL, et al. Genetic linkage of hyper-IgE syndrome to chromosome 4. Am J Hum Genet. 1999;65:735–44.
Grimbacher B, Holland SM, Puck JM. Hyper-IgE syndromes. Immunol Rev. 2005;203:244–50.
Woellner C, Gertz EM, Schäffer AA, Lagos M, Perro M, Glocker EO, et al. Mutations in STAT3 and diagnostic guidelines for hyper-IgE syndrome. J Allergy Clin Immunol. 2010;125:424–32. e8.
Lee WI, Kuo ML, Huang JL, Lin SJ, Wu CJ. Distribution and clinical aspects of primary immunodeficiencies in a Taiwan pediatric tertiary hospital during a 20-year period. J Clin Immunol. 2005;25:162–73.
Lee WI, Zhu Q, Gambineri E, Jin Y, Welcher AA, Ochs HD. Inducible CO-stimulator molecule, a candidate gene for defective isotype switching, is normal in patients with hyper-IgM syndrome of unknown molecular diagnosis. J Allergy Clin Immunol. 2003;112:958–64.
Lee WI, Torgerson TR, Schumacher MJ, Yel L, Zhu Q, Ochs HD. Molecular analysis of a large cohort of patients with the hyper immunoglobulin M (IgM) syndrome. Blood. 2005;105:1881–90.
Lee WI, Jaing TH, Hsieh MY, Kuo ML, Lin SJ, Huang JL. Distribution, infections, treatments and molecular analysis in a large cohort of patients with primary immunodeficiency diseases (PIDs) in Taiwan. J Clin Immunol. 2006;26:274–83.
Liang FC, Wei YC, Jiang TH, Hsiehi MY, Wen YC, Chiou YS, et al. Current classification and status of primary immunodeficiency diseases in Taiwan. Acta Paediatr Taiwan. 2008;49:3–8.
Schur PH. IgG subclasses—a review. Ann Allergy. 1987;58:89–96.
Dohil M, Prendiville JS. Treatment of molluscum contagiosum with oral cimetidine: clinical experience in 13 patients. Pediatr Dermatol. 1996;13:310–2.
Kilic SS, Kilicbay F. Interferon-alpha treatment of molluscum contagiosum in a patient with hyperimmunoglobulin E syndrome. Pediatrics. 2006;117:e1253–1255.
Wolach B, Eliakim A, Pomeranz A, Cohen AH, Nusbacher J, Metzker A. Cyclosporin treatment of hyperimmunoglobulin E syndrome. Lancet. 1996;347:67.
Etzioni A, Shehadeh N, Brecher A, Yorman S, Pollack S. Cyclosporin A in hyperimmunoglobulin E syndrome. Ann Allergy Asthma Immunol. 1997;78:413–4.
Young TY, Jerome D, Gupta S. Hyperimmunoglobulinemia E syndrome associated with coronary artery aneurysms: deficiency of central memory CD4+ T cells and expansion of effector memory CD4+ T cells. Ann Allergy Asthma Immunol. 2007;98:389–92.
Freeman AF, Kleiner DE, Nadiminti H, Davis J, Quezado M, Anderson V, et al. Causes of death in hyper-IgE syndrome. J Allergy Clin Immunol. 2007;119:1234–40.
Nester TA, Wagnon AH, Reilly WF, Spitzer G, Kjeldsberg CR, Hill HR. Effects of allogeneic peripheral stem cell transplantation in a patient with job syndrome of hyperimmunoglobulinemia E and recurrent infections. Am J Med. 1998;105:162–4.
Gennery AR, Flood TJ, Abinun M, Cant AJ. Bone marrow transplantation does not correct the hyper IgE syndrome. Bone Marrow Transplant. 2000;25:1303–5.
Goussetis E, Peristeri I, Kitra V, Traeger-Synodinos J, Theodosaki M, Psarra K, et al. Successful long-term immunologic reconstitution by allogeneic hematopoietic stem cell transplantation cures patients with autosomal dominant hyper-IgE syndrome. J Allergy Clin Immunol. 2010;126:392–4.
Gatz SA, Benninghoff U, Schütz C, Schulz A, Hönig M, Pannicke U, Holzmann KH, Schwarz K, Friedrich W. Curative treatment of autosomal-recessive hyper-IgE syndrome by hematopoietic cell transplantation. Bone Marrow Transplant (2010) (in press)
Xie L, Hu X, Li Y, Zhang W, Chen L. Hyper-IgE syndrome with STAT3 mutation: a case report in Mainland China. Clin Dev Immunol. 2010;2010:289873.
Farkas LG. Anthropometry of the head and face in medicine. 2nd ed. New York: Raven Press; 1994. p. 286.
Renner ED, Rylaarsdam S, Anover-Sombke S, Rack AL, Reichenbach J, Carey JC, et al. Novel signal transducer and activator of transcription 3 (STAT3) mutations, reduced T(H)17 cell numbers, and variably defective STAT3 phosphorylation in hyper-IgE syndrome. J Allergy Clin Immunol. 2008;122:181–7.
Acknowledgments
The authors wish to thank all of the patients and their families for their kind cooperation, as well as their physicians for the referrals. This study was supported by the Chang Gung Medical Research Progress Grant CMRPG 490011 and the National Science Council (Grants NSC 99-2314-B-182-003-MY3 and NMRPD190315).
Conflict of interest
All of the authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Lee, WI., Huang, JL., Lin, SJ. et al. Clinical Aspects and Genetic Analysis of Taiwanese Patients with the Phenotype of Hyper-Immunoglobulin E Recurrent Infection Syndromes (HIES). J Clin Immunol 31, 272–280 (2011). https://doi.org/10.1007/s10875-010-9479-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-010-9479-1