Abstract
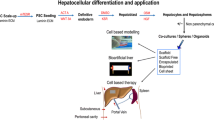
Although significant progress has been made in the field of orthotopic liver transplantation, cell-based therapies seem to be a promising alternative to whole-organ transplantation. The reasons are manifold but organ shortage is the main cause for this approach. However, many problems such as the question which cell type should be used or which application site is best for transplantation have been raised. In addition, some clinicians have had success by cultivating liver cells in bioreactors for temporary life support. Besides answering the question which cell type, which injection site or even which culture form should be used for liver support recent international harmonization of legal requirements is needed to be addressed by clinicians, scientists and companies dealing with cellular therapies. We here briefly summarize the possible cell types used to partially or temporarily correct liver diseases, the most recent development of bioreactor technology and important regulatory issues.



Similar content being viewed by others
References
Street CN, Rajotte RV, et al. Stem cells: a promising source of pancreatic islets for transplantation in type 1 diabetes. Curr Top Dev Biol. 2003;58:111–36.
Ehnert S, Glanemann M, et al. The possible use of stem cells in regenerative medicine: dream or reality? Langenbecks Arch Surg. 2009;394:985–97.
Sauer IM, Zeilinger K, et al. Extracorporeal liver support based on primary human liver cells and albumin dialysis—treatment of a patient with primary graft non-function. J Hepatol. 2003;39:649–53.
Strom S, Fisher R. Hepatocyte transplantation: new possibilities for therapy. Gastroenterology. 2003;124:568–71.
Nagata H, Ito M, et al. Route of hepatocyte delivery affects hepatocyte engraftment in the spleen. Transplantation. 2003;76:732–4.
Kobayashi N, Ito M, et al. Treatment of carbon tetrachloride and phenobarbital-induced chronic liver failure with intrasplenic hepatocyte transplantation. Cell Transplant. 2000;9:671–3.
Cai J, Ito M, et al. Treatment of liver failure in rats with end-stage cirrhosis by transplantation of immortalized hepatocytes. Hepatology. 2002;36:386–94.
Nagata H, Ito M, et al. Treatment of cirrhosis and liver failure in rats by hepatocyte xenotransplantation. Gastroenterology. 2003;124:422–31.
Mito M, Kusano M, et al. Hepatocyte transplantation in man. Transplant Proc. 1992;24:3052–3.
Strom SC, Chowdhury JR, et al. Hepatocyte transplantation for the treatment of human disease. Semin Liver Dis. 1999;19:39–48.
Sipe JD. Tissue engineering and reparative medicine. Ann N Y Acad Sci. 2002;961:1–9.
Barker JN, Wagner JE. Umbilical-cord blood transplantation for the treatment of cancer. Nat Rev Cancer. 2003;3:526–32.
Thomas ED. Bone marrow transplantation from bench to bedside. Ann N Y Acad Sci. 1995;770:34–41.
Flohr TR, Bonatti H Jr, et al. The use of stem cells in liver disease. Curr Opin Organ Transplant. 2009;14:64–71.
Sancho-Bru P, Najimi M, et al. Stem and progenitor cells for liver repopulation: can we standardise the process from bench to bedside? Gut. 2009;58:594–603.
Habibullah CM, Syed IH, et al. Human fetal hepatocyte transplantation in patients with fulminant hepatic failure. Transplantation. 1994;58:951–2.
Pietrosi G, Vizzini GB, et al. Clinical applications of hepatocyte transplantation. World J Gastroenterol. 2009;15:2074–7.
Puppi J, Dhawan A. Human hepatocyte transplantation overview. Methods Mol Biol. 2009;481:1–16.
Strom SC, Fisher RA, et al. Hepatocyte transplantation as a bridge to orthotopic liver transplantation in terminal liver failure. Transplantation. 1997;63:559–69.
Fox IJ, Chowdhury JR, et al. Treatment of the Crigler-Najjar syndrome type I with hepatocyte transplantation. N Engl J Med. 1998;338:1422–6.
Bohnen NI, Charron M, et al. Use of indium-111-labeled hepatocytes to determine the biodistribution of transplanted hepatocytes through portal vein infusion. Clin Nucl Med. 2000;25:447–50.
Horslen SP, McCowan TC, et al. Isolated hepatocyte transplantation in an infant with a severe urea cycle disorder. Pediatrics. 2003;111:1262–7.
Muraca M, Gerunda G, et al. Hepatocyte transplantation as a treatment for glycogen storage disease type 1a. Lancet. 2002;359:317–8.
Sokal EM, Smets F, et al. Hepatocyte transplantation in a 4-year-old girl with peroxisomal biogenesis disease: technique, safety, and metabolic follow-up. Transplantation. 2003;76:735–8.
Dhawan A, Mitry RR, et al. Hepatocyte transplantation for inherited factor VII deficiency. Transplantation. 2004;78:1812–4.
Allen KJ, Mifsud NA, et al. Cell-mediated rejection results in allograft loss after liver cell transplantation. Liver Transplant. 2008;14:688–94.
Meyburg J, Schmidt J, et al. Liver cell transplantation in children. Clin Transplant. 2009;23(Suppl 21):75–82.
Ambrosino G, Varotto S, et al. Isolated hepatocyte transplantation for Crigler-Najjar syndrome type 1. Cell Transplant. 2005;14:151–7.
Meyburg J, Hoerster F, et al. Use of the middle colic vein for liver cell transplantation in infants and small children. Transplant Proc. 2008;40:936–7.
Meyburg J, Das AM, et al. One liver for four children: first clinical series of liver cell transplantation for severe neonatal urea cycle defects. Transplantation. 2009;87:636–41.
Puppi J, Tan N, et al. Hepatocyte transplantation followed by auxiliary liver transplantation—a novel treatment for ornithine transcarbamylase deficiency. Am J Transplant. 2008;8:452–7.
Kreymann B, Seige M, et al. Albumin dialysis: effective removal of copper in a patient with fulminant Wilson disease and successful bridging to liver transplantation: a new possibility for the elimination of protein-bound toxins. J Hepatol. 1999;31:1080–5.
Patzer JF II, Safta SA, et al. Slow continuous ultrafiltration with bound solute dialysis. ASAIO J. 2006;52:47–58.
Rifai K, Ernst T, et al. Prometheus—a new extracorporeal system for the treatment of liver failure. J Hepatol. 2003;39:984–90.
Stange J, Hassanein TI, et al. The molecular adsorbents recycling system as a liver support system based on albumin dialysis: a summary of preclinical investigations, prospective, randomized, controlled clinical trial, and clinical experience from 19 centers. Artif Organs. 2002;26:103–10.
Chan C, Berthiaume F, et al. Hepatic tissue engineering for adjunct and temporary liver support: critical technologies. Liver Transplant. 2004;10:1331–42.
Ting PP, Demetriou AA. Clinical experience with artificial liver support systems. Can J Gastroenterol. 2000;14(Suppl D):79D–84D.
Fiegel HC, Kaufmann PM, et al. Hepatic tissue engineering: from transplantation to customized cell-based liver directed therapies from the laboratory. J Cell Mol Med. 2008;12:56–66.
Gerlach JC, Zeilinger K, et al. Bioartificial liver systems: why, what, whither? Regen Med. 2008;3:575–95.
Kjaergard LL, Liu J, et al. Artificial and bioartificial support systems for acute and acute-on-chronic liver failure: a systematic review. JAMA. 2003;289:217–22.
van de Kerkhove MP, Hoekstra R, et al. Clinical application of bioartificial liver support systems. Ann Surg. 2004;240:216–30.
Ellis AJ, Hughes RD, et al. Pilot-controlled trial of the extracorporeal liver assist device in acute liver failure. Hepatology. 1996;24:1446–51.
Millis JM, Cronin DC, et al. Initial experience with the modified extracorporeal liver-assist device for patients with fulminant hepatic failure: system modifications and clinical impact. Transplantation. 2002;74:1735–46.
Sussman NL, Chong MG, et al. Reversal of fulminant hepatic failure using an extracorporeal liver assist device. Hepatology. 1992;16:60–5.
Mazariegos GV, Kramer DJ, et al. Safety observations in phase I clinical evaluation of the Excorp Medical Bioartificial Liver Support System after the first four patients. ASAIO J. 2001;47:471–5.
Mazariegos GV, Patzer JF II, et al. First clinical use of a novel bioartificial liver support system (BLSS). Am J Transplant. 2002;2:260–6.
Demetriou AA, Brown RS Jr, et al. Prospective, randomized, multicenter, controlled trial of a bioartificial liver in treating acute liver failure. Ann Surg. 2004;239:660–7. discussion 7-70.
Watanabe FD, Mullon CJ, et al. Clinical experience with a bioartificial liver in the treatment of severe liver failure. A phase I clinical trial. Ann Surg. 1997;225:484–91. discussion 91-4.
van de Kerkhove MP, Di Florio E, et al. Phase I clinical trial with the AMC-bioartificial liver. Int J Artif Organs. 2002;25:950–9.
Morsiani E, Pazzi P, et al. Early experiences with a porcine hepatocyte-based bioartificial liver in acute hepatic failure patients. Int J Artif Organs. 2002;25:192–202.
Gerlach JC, Botsch M, et al. Experimental evaluation of a cell module for hybrid liver support. Int J Artif Organs. 2001;24:793–8.
Irgang M, Sauer IM, et al. Porcine endogenous retroviruses: no infection in patients treated with a bioreactor based on porcine liver cells. J Clin Virol. 2003;28:141–54.
Morsiani E, Brogli M, et al. Biologic liver support: optimal cell source and mass. Int J Artif Organs. 2002;25:985–93.
Gerlach JC, Zeilinger K, et al. Extracorporeal liver support: porcine or human cell based systems? Int J Artif Organs. 2002;25:1013–8.
Tsiaoussis J, Newsome PN, et al. Which hepatocyte will it be? Hepatocyte choice for bioartificial liver support systems. Liver Transplant. 2001;7:2–10.
Kobayashi N, Westerman KA, et al. A reversibly immortalized human hepatocyte cell line as a source of hepatocyte-based biological support. Addict Biol. 2001;6:293–300.
Alison MR, Islam S, et al. Stem cells in liver regeneration, fibrosis and cancer: the good, the bad and the ugly. J Pathol. 2009;217:282–98.
Cantz T, Manns MP, et al. Stem cells in liver regeneration and therapy. Cell Tissue Res. 2008;331:271–82.
Dan YY, Yeoh GC. Liver stem cells: a scientific and clinical perspective. J Gastroenterol Hepatol. 2008;23:687–98.
Haridass D, Narain N, et al. Hepatocyte transplantation: waiting for stem cells. Curr Opin Organ Transplant. 2008;13:627–32.
Kakinuma S, Nakauchi H, et al. Hepatic stem/progenitor cells and stem-cell transplantation for the treatment of liver disease. J Gastroenterol. 2009;44:167–72.
Weiss TS, Lichtenauer M, et al. Hepatic progenitor cells from adult human livers for cell transplantation. Gut. 2008;57:1129–38.
Souza BS, Nogueira RC, et al. Current status of stem cell therapy for liver diseases. Cell Transplant. 2009;18:1261–79.
Quante M, Wang TC. Stem cells in gastroenterology and hepatology. Nat Rev Gastroenterol Hepatol. 2009;6:724–37.
Schmelzer E, Wauthier E, et al. The phenotypes of pluripotent human hepatic progenitors. Stem Cells. 2006;24:1852–8.
Schmelzer E, Zhang L, et al. Human hepatic stem cells from fetal and postnatal donors. J Exp Med. 2007;204:1973–87.
Wohlers I, Stachelscheid H, et al. The characterization tool: a knowledge-based stem cell, differentiated cell, and tissue database with a web-based analysis front-end. Stem Cell Res. 2009;3:88–95.
Kinoshita T, Sekiguchi T, et al. Hepatic differentiation induced by oncostatin M attenuates fetal liver hematopoiesis. Proc Natl Acad Sci USA. 1999;96:7265–70.
Stachelscheid H, Urbaniak T, et al. Isolation and characterization of adult human liver progenitors from ischemic liver tissue derived from therapeutic hepatectomies. Tissue Eng A. 2009;15:1633–43.
Ruhnke M, Nussler AK, et al. Human monocyte-derived neohepatocytes: a promising alternative to primary human hepatocytes for autologous cell therapy. Transplantation. 2005;79:1097–103.
Ruhnke M, Ungefroren H, et al. Differentiation of in vitro-modified human peripheral blood monocytes into hepatocyte-like and pancreatic islet-like cells. Gastroenterology. 2005;128:1774–86.
Shen CN, Slack JM, et al. Molecular basis of transdifferentiation of pancreas to liver. Nat Cell Biol. 2000;2:879–87.
Tosh D, Shen CN, et al. Conversion of pancreatic cells to hepatocytes. Biochem Soc Trans. 2002;30:51–5.
Banas A, Teratani T, et al. Adipose tissue-derived mesenchymal stem cells as a source of human hepatocytes. Hepatology. 2007;46:219–28.
Najimi M, Khuu DN, et al. Adult-derived human liver mesenchymal-like cells as a potential progenitor reservoir of hepatocytes? Cell Transplant. 2007;16:717–28.
Lee HS, Crane GG, et al. Clonal expansion of adult rat hepatic stem cell lines by suppression of asymmetric cell kinetics (SACK). Biotechnol Bioeng. 2003;83:760–71.
Schwartz RE, Reyes M, et al. Multipotent adult progenitor cells from bone marrow differentiate into functional hepatocyte-like cells. J Clin Invest. 2002;109:1291–302.
Miyazaki M, Hardjo M, et al. Isolation of a bone marrow-derived stem cell line with high proliferation potential and its application for preventing acute fatal liver failure. Stem Cells. 2007;25:2855–63.
Aurich H, Sgodda M, et al. Hepatocyte differentiation of mesenchymal stem cells from human adipose tissue in vitro promotes hepatic integration in vivo. Gut. 2009;58:570–81.
Aurich I, Mueller LP, et al. Functional integration of hepatocytes derived from human mesenchymal stem cells into mouse livers. Gut. 2007;56:405–15.
Glanemann M, Gaebelein G, et al. Transplantation of monocyte-derived hepatocyte-like cells (NeoHeps) improves survival in a model of acute liver failure. Ann Surg. 2009;249:149–54.
Ehnert S, Nussler AK, et al. Blood monocyte-derived neohepatocytes as in vitro test system for drug metabolism. Drug Metab Dispos. 2008;36:1922–9.
Lysy PA, Smets F, et al. Human skin fibroblasts: from mesodermal to hepatocyte-like differentiation. Hepatology. 2007;46:1574–85.
Tosh D, Shen CN, et al. Differentiated properties of hepatocytes induced from pancreatic cells. Hepatology. 2002;36:534–43.
Burke ZD, Shen CN, et al. Characterization of liver function in transdifferentiated hepatocytes. J Cell Physiol. 2006;206:147–59.
Sasaki K, Kon J, et al. Proliferation of hepatocyte progenitor cells isolated from adult human livers in serum-free medium. Cell Transplant. 2008;17:1221–30.
Gerlach JC, Mutig K, et al. Use of primary human liver cells originating from discarded grafts in a bioreactor for liver support therapy and the prospects of culturing adult liver stem cells in bioreactors: a morphologic study. Transplantation. 2003;76:781–6.
Schmelzer E, Mutig K, et al. Effect of human patient plasma ex vivo treatment on gene expression and progenitor cell activation of primary human liver cells in multi-compartment 3D perfusion bioreactors for extra-corporeal liver support. Biotechnol Bioeng. 2009;103:817–27.
Ring A, Gerlach J, et al. Hepatic maturation of human fetal hepatocytes in four-compartment three-dimensional perfusion culture. Tissue Eng C. 2010;16:835–45.
Mummery C, Ward-van Oostwaard D, et al. Differentiation of human embryonic stem cells to cardiomyocytes: role of coculture with visceral endoderm-like cells. Circulation. 2003;107:2733–40.
Nir SG, David R, et al. Human embryonic stem cells for cardiovascular repair. Cardiovasc Res. 2003;58:313–23.
Rubart M, Field LJ. Cardiac repair by embryonic stem-derived cells. Handb Exp Pharmacol. 2006;174:73–100.
Agarwal S, Holton KL, et al. Efficient differentiation of functional hepatocytes from human embryonic stem cells. Stem Cells. 2008;26:1117–27.
D’Amour KA, Agulnick AD, et al. Efficient differentiation of human embryonic stem cells to definitive endoderm. Nat Biotechnol. 2005;23:1534–41.
Hay DC, Zhao D, et al. Efficient differentiation of hepatocytes from human embryonic stem cells exhibiting markers recapitulating liver development in vivo. Stem Cells. 2008;26:894–902.
Nakagawa M, Koyanagi M, et al. Generation of induced pluripotent stem cells without Myc from mouse and human fibroblasts. Nat Biotechnol. 2008;26:101–6.
Ohnuki M, Takahashi K, et al., Generation and characterization of human induced pluripotent stem cells. Curr Protoc Stem Cell Biol 2009;Chapter 4:Unit 4A 2.
Takahashi K, Tanabe K, et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–72.
Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–76.
Okita K, Ichisaka T, et al. Generation of germline-competent induced pluripotent stem cells. Nature. 2007;448:313–7.
Yu J, Vodyanik MA, et al. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318:1917–20.
Huangfu D, Osafune K, et al. Induction of pluripotent stem cells from primary human fibroblasts with only Oct4 and Sox2. Nat Biotechnol. 2008;26:1269–75.
Wernig M, Meissner A, et al. In vitro reprogramming of fibroblasts into a pluripotent ES-cell-like state. Nature. 2007;448:318–24.
Feng B, Jiang J, et al. Reprogramming of fibroblasts into induced pluripotent stem cells with orphan nuclear receptor Esrrb. Nat Cell Biol. 2009;11:197–203.
Park IH, Zhao R, et al. Reprogramming of human somatic cells to pluripotency with defined factors. Nature. 2008;451:141–6.
Lowry WE, Richter L, et al. Generation of human induced pluripotent stem cells from dermal fibroblasts. Proc Natl Acad Sci USA. 2008;105:2883–8.
Park IH, Lerou PH, et al. Generation of human-induced pluripotent stem cells. Nat Protoc. 2008;3:1180–6.
Kim JB, Sebastiano V, et al. Oct4-induced pluripotency in adult neural stem cells. Cell. 2009;136:411–9.
Kim JB, Zaehres H, et al. Pluripotent stem cells induced from adult neural stem cells by reprogramming with two factors. Nature. 2008;454:646–50.
Carey BW, Markoulaki S, et al. Reprogramming of murine and human somatic cells using a single polycistronic vector. Proc Natl Acad Sci USA. 2009;106:157–62.
Ishii T, Fukumitsu K, et al. Effects of extracellular matrixes and growth factors on the hepatic differentiation of human embryonic stem cells. Am J Physiol Gastrointest Liver Physiol. 2008;295:G313–21.
Hay DC, Fletcher J, et al. Highly efficient differentiation of hESCs to functional hepatic endoderm requires ActivinA and Wnt3a signaling. Proc Natl Acad Sci USA. 2008;105:12301–6.
Momose Y, Matsunaga T, et al. Differentiation of monkey embryonic stem cells into hepatocytes and mRNA expression of cytochrome p450 enzymes responsible for drug metabolism: comparison of embryoid body formation conditions and matrices. Biol Pharm Bull. 2009;32:619–26.
Sullivan GJ, Hay DC, et al. Generation of functional human hepatic endoderm from human induced pluripotent stem cells. Hepatology. 2009;51:329–35.
MacDonald JM, Wolfe SP, et al. Effect of flow configuration and membrane characteristics on membrane fouling in a novel multicoaxial hollow-fiber bioartificial liver. Ann N Y Acad Sci. 2001;944:334–43.
De Bartolo L, Jarosch-Von Schweder G, et al. A novel full-scale flat membrane bioreactor utilizing porcine hepatocytes: cell viability and tissue-specific functions. Biotechnol Prog. 2000;16:102–8.
Shito M, Kim NH, et al. In vitro and in vivo evaluation of albumin synthesis rate of porcine hepatocytes in a flat-plate bioreactor. Artif Organs. 2001;25:571–8.
Shito M, Tilles AW, et al. Efficacy of an extracorporeal flat-plate bioartificial liver in treating fulminant hepatic failure. J Surg Res. 2003;111:53–62.
Flendrig LM, la Soe JW, et al. In vitro evaluation of a novel bioreactor based on an integral oxygenator and a spirally wound nonwoven polyester matrix for hepatocyte culture as small aggregates. J Hepatol. 1997;26:1379–92.
Bhatia SN, Yarmush ML, et al. Controlling cell interactions by micropatterning in co-cultures: hepatocytes and 3T3 fibroblasts. J Biomed Mater Res. 1997;34:189–99.
Kim SS, Utsunomiya H, et al. Survival and function of hepatocytes on a novel three-dimensional synthetic biodegradable polymer scaffold with an intrinsic network of channels. Ann Surg. 1998;228:8–13.
Powers MJ, Domansky K, et al. A microfabricated array bioreactor for perfused 3D liver culture. Biotechnol Bioeng. 2002;78:257–69.
Powers MJ, Janigian DM, et al. Functional behavior of primary rat liver cells in a three-dimensional perfused microarray bioreactor. Tissue Eng. 2002;8:499–513.
Ambrosino G, Varotto S, et al. ALEX (artificial liver for extracorporeal xenoassistance): a new bioreactor containing a porcine autologous biomatrix as hepatocyte support. Preliminary results in an ex vivo experimental model. Int J Artif Organs. 2002;25:960–5.
Linti C, Zipfel A, et al. Cultivation of porcine hepatocytes in polyurethane nonwovens as part of a biohybrid liver support system. Int J Artif Organs. 2002;25:994–1000.
Gerlach JC, Kloppel K, et al. Hepatocyte aggregate culture technique for bioreactors in hybrid liver support systems. Int J Artif Organs. 1993;16:843–6.
Gerlach JC, Schnoy N, et al. Improved hepatocyte in vitro maintenance in a culture model with woven multicompartment capillary systems: electron microscopy studies. Hepatology. 1995;22:546–52.
Zeilinger K, Holland G, et al. Time course of primary liver cell reorganization in three-dimensional high-density bioreactors for extracorporeal liver support: an immunohistochemical and ultrastructural study. Tissue Eng. 2004;10:1113–24.
Gerlach JC, Brayfield C, et al. Lidocaine/monoethylglycinexylidide test, galactose elimination test, and sorbitol elimination test for metabolic assessment of liver cell bioreactors. Artif Organs. 2010;34:462–72.
Pless G, Steffen I, et al. Evaluation of primary human liver cells in bioreactor cultures for extracorporeal liver support on the basis of urea production. Artif Organs. 2006;30:686–94.
Zeilinger K, Sauer IM, et al. Three-dimensional co-culture of primary human liver cells in bioreactors for in vitro drug studies: effects of the initial cell quality on the long-term maintenance of hepatocyte-specific functions. Altern Lab Anim. 2002;30:525–38.
Sauer IM, Zeilinger K, et al. Primary human liver cells as source for modular extracorporeal liver support—a preliminary report. Int J Artif Organs. 2002;25:1001–5.
McCuskey RS. Morphological mechanisms for regulating blood flow through hepatic sinusoids. Liver. 2000;20:3–7.
McCuskey RS. The hepatic microvascular system in health and its response to toxicants. Anat Rec (Hoboken). 2008;291:661–71.
Saxena R, Theise ND, et al. Microanatomy of the human liver-exploring the hidden interfaces. Hepatology. 1999;30:1339–46.
Kamegaya Y, Oda M, et al., Evidence for the spontaneous contractility of ITO cells by time-lapse cinematographic and computerized image analysis. In: Wisse E, et al., editors, Cells of the hepatic sinusoid. Leiden: Kupffer Cell Foundation; 1995.
Van Der Smissen P, Breat F, et al., The cytoskeleton of the liver sieve in situ: a TEM study. In: Wisse E, et al., editors, Cells of the hepatic sinusoid. Leiden: Kupffer Cell Foundation; 1995.
Tiniakos DG, Lee JA, et al. Innervation of the liver: morphology and function. Liver. 1996;16:151–60.
Halme DG, Kessler DA. FDA regulation of stem-cell-based therapies. N Engl J Med. 2006;355:1730–5.
von Tigerstrom BJ. The challenges of regulating stem cell-based products. Trends Biotechnol. 2008;26:653–8.
Schneider CK, Salmikangas P, et al. Challenges with advanced therapy medicinal products and how to meet them. Nat Rev Drug Discov. 2010;9:195–201.
Schneider CK, Schaffner-Dallmann G. Typical pitfalls in applications for marketing authorization of biotechnological products in Europe. Nat Rev Drug Discov. 2008;7:893–9.
Rayment EA, Williams DJ. Concise review: mind the gap: challenges in characterizing and quantifying cell- and tissue-based therapies for clinical translation. Stem Cells. 2010;28:996–1004.
Daar AS, Bhatt A, et al. Stem cell research and transplantation: science leading ethics. Transplant Proc. 2004;36:2504–6.
Daar J. Sliding the slope toward human cloning. Am J Bioeth. 2001;1:23–4.
Daar JF. The prospect of human cloning: improving nature or dooming the species? Seton Hall Law Rev. 2003;33:511–72.
Daar AS. Paid organ procurement: pragmatic and ethical viewpoints. Transplant Proc. 2004;36:1876–7.
de Vries RB, Oerlemans A, et al. Ethical aspects of tissue engineering: a review. Tissue Eng B. 2008;14:367–75.
Thasler WE, Weiss TS, et al. Charitable state-controlled foundation human tissue and cell research: ethic and legal aspects in the supply of surgically removed human tissue for research in the academic and commercial sector in Germany. Cell Tissue Bank. 2003;4:49–56.
Acknowledgments
The present work has been partially supported by BMBF—0315208E (EmbryoTox, AKN), BMBF—01GN0984 (RegMed, AKN), BMBF—0315741 (Virtual Liver, AKN/MG), BMBF—0315753 (Virtual Liver, TSW), supported grant from the Medical Faculty of the University of Regensburg (ReForM-C, TSW).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nussler, A.K., Zeilinger, K., Schyschka, L. et al. Cell therapeutic options in liver diseases: cell types, medical devices and regulatory issues. J Mater Sci: Mater Med 22, 1087–1099 (2011). https://doi.org/10.1007/s10856-011-4306-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-011-4306-7