Abstract
Background
Hemostasis at the femoral venous access site after atrial fibrillation (AF) ablation is often prolonged because of aggressive anticoagulation and the use of several large-sized sheaths. A newly developed hemostatic pad containing a natural mineral called kaolin causes blood to clot quickly. We evaluated the efficacy of this pad for hemostasis at the venous access site after AF ablation.
Methods
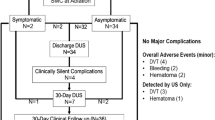
Patients who were scheduled to undergo AF ablation were randomized to be treated with manual compression with (n = 59) or without kaolin-impregnated pads (n = 59) as hemostatic approaches at the femoral venous access site following sheath removal. Hemostasis time, rebleeding frequency, massive hematoma, device-related complications, and deep venous thrombosis (DVT) were compared between the two groups.
Results
Hemostasis time in the patients treated with kaolin-impregnated pads was significantly shorter than in those treated without (6.1 ± 2.3 vs. 14.5 ± 4.0 min; p < 0.0001). Multiple linear regression analysis revealed that the use of kaolin-impregnated pads was the only independent variable reducing hemostasis time (β = −0.78; p < 0.0001). However, rebleeding rates of the two groups were similar (37% with vs. 46% without kaolin-impregnated pads; p = 0.35). Only one patient had a massive groin hematoma, and no patient had device-related complications or DVT.
Conclusions
Kaolin-impregnated hemostatic pads safely and effectively decreased hemostasis time for the femoral venous access site in patients undergoing AF ablation. However, whether its use allows earlier postprocedural ambulation is difficult to predict.



Similar content being viewed by others
References
Kannel, W. B., Abbott, R. D., Savage, D. D., & McNamara, P. M. (1982). Epidemiologic features of chronic atrial fibrillation: the Framingham study. The New England Journal of Medicine, 306, 1018–1022.
Haïssaguerre, M., Jaïs, P., Shah, D. C., Takahashi, A., Hocini, M., Quiniou, G., et al. (1998). Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. The New England Journal of Medicine, 339, 659–666.
Pappone, C., Rosanio, S., Oreto, G., Tocchi, M., Gugliotta, F., Vicedomini, G., et al. (2000). Circumferential radiofrequency ablation of pulmonary vein ostia: A new anatomic approach for curing atrial fibrillation. Circulation, 102, 2619–2628.
Wyse, D. G., Waldo, A. L., DiMarco, J. P., Domanski, M. J., Rosenberg, Y., Schron, E. B., et al. (2002). A comparison of rate control and rhythm control in patients with atrial fibrillation. The New England Journal of Medicine, 347, 1825–1833.
Ouyang, F., Bänsch, D., Ernst, S., Schaumann, A., Hachiya, H., Chen, M., et al. (2004). Complete isolation of left atrium surrounding the pulmonary veins: new insights from the double-Lasso technique in paroxysmal atrial fibrillation. Circulation, 110, 2090–2096.
Cappato, R., Calkins, H., Chen, S. A., Davies, W., Iesaka, Y., Kalman, J., et al. (2005). Worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation, 111, 1100–1105.
Bertaglia, E., Zoppo, F., Tondo, C., Colella, A., Mantovan, R., Senatore, G., et al. (2007). Early complications of pulmonary vein catheter ablation for atrial fibrillation: a multicenter prospective registry on procedural safety. Heart Rhythm, 4, 1265–1271.
Dagres, N., Hindricks, G., Kottkamp, H., Sommer, P., Gaspar, T., Bode, K., et al. (2009). Complications of atrial fibrillation ablation in a high-volume center in 1, 000 procedures: still cause for concern? Journal of Cardiovascular Electrophysiology, 20, 1014–1019.
Ellis, E. R., Culler, S. D., Simon, A. W., & Reynolds, M. R. (2009). Trends in utilization and complications of catheter ablation for atrial fibrillation in Medicare beneficiaries. Heart Rhythm, 6, 1267–1273.
Kapadia, S. R., Raymond, R., Knopf, W., Jenkins, S., Chapekis, A., Ansel, G., et al. (2001). The 6Fr Angio-Seal arterial closure device: results from a multimember prospective registry. The American Journal of Cardiology, 87, 789–791.
Bhatt, D. L., Raymond, R. E., Feldman, T., Braden, G. A., Murphy, B., Strumpf, R., et al. (2002). Successful “pre-closure” of 7Fr and 8Fr femoral arteriotomies with a 6Fr suture-based device (the Multicenter Interventional Closer Registry). The American Journal of Cardiology, 89, 777–779.
Applegate, R. J., Grabarczyk, M. A., Little, W. C., Craven, T., Walkup, M., Kahl, F. R., et al. (2002). Vascular closure devices in patients treated with anticoagulation and IIb/IIIa receptor inhibitors during percutaneous revascularization. Journal of the American College of Cardiology, 40, 78–83.
Jaff, M. R., Hadley, G., Hermiller, J. B., Simonton, C., Hinohara, T., Cannon, L., et al. (2006). The safety and efficacy of the StarClose Vascular Closure System: the ultrasound substudy of the CLIP study. Catheterization and Cardiovascular Interventions, 68, 684–689.
Bangalore, S., Arora, N., & Resnic, F. S. (2009). Vascular closure device failure: frequency and implications: a propensity-matched analysis. Circulation. Cardiovascular Interventions, 2, 549–556.
Coto, H. A. (2002). Closure of the femoral vein puncture site after transcatheter procedures using Angio-Seal. Catheterization and Cardiovascular Interventions, 55, 16–19.
Mahadevan, V. S., Jimeno, S., Benson, L. N., McLaughlin, P. R., & Horlick, E. M. (2008). Pre-closure of femoral venous access sites used for large-sized sheath insertion with the Perclose device in adults undergoing cardiac intervention. Heart, 94, 571–572.
Kinnaird, T. D., Stabile, E., Mintz, G. S., Lee, C. W., Canos, D. A., Gevorkian, N., et al. (2003). Incidence, predictors, and prognostic implications of bleeding and blood transfusion following percutaneous coronary interventions. The American Journal of Cardiology, 92, 930–935.
Pristipino, C., Pelliccia, F., Granatelli, A., Pasceri, V., Roncella, A., Speciale, G., et al. (2007). Comparison of access-related bleeding complications in women versus men undergoing percutaneous coronary catheterization using the radial versus femoral artery. The American Journal of Cardiology, 99, 1216–1221.
Bertrand, O. F., Larose, E., Rodés-Cabau, J., Gleeton, O., Taillon, I., Roy, L., et al. (2009). Incidence, predictors, and clinical impact of bleeding after transradial coronary stenting and maximal antiplatelet therapy. American Heart Journal, 157, 164–169.
Cox, N., Resnic, F. S., Popma, J. J., Simon, D. I., Eisenhauer, A. C., & Rogers, C. (2004). Comparison of the risk of vascular complications associated with femoral and radial access coronary catheterization procedures in obese versus nonobese patients. The American Journal of Cardiology, 94, 1174–1177.
Byrne, J., Spence, M. S., Fretz, E., Mildenberger, R., Chase, A., Berry, B., et al. (2009). Body mass index, periprocedural bleeding, and outcome following percutaneous coronary intervention (from the British Columbia Cardiac Registry). The American Journal of Cardiology, 103, 507–511.
Chew, D. P., Bhatt, D. L., Lincoff, A. M., Moliterno, D. J., Brener, S. J., Wolski, K. E., et al. (2001). Defining the optimal activated clotting time during percutaneous coronary intervention: aggregate results from 6 randomized, controlled trials. Circulation, 103, 961–966.
Hillegass, W. B., Brott, B. C., Chapman, G. D., Phillips, H. R., Stack, R. S., Tcheng, J. E., et al. (2002). Relationship between activated clotting time during percutaneous intervention and subsequent bleeding complications. American Heart Journal, 144, 501–507.
Brener, S. J., Moliterno, D. J., Lincoff, A. M., Steinhubl, S. R., Wolski, K. E., & Topol, E. J. (2004). Relationship between activated clotting time and ischemic or hemorrhagic complications: analysis of 4 recent randomized clinical trials of percutaneous coronary intervention. Circulation, 110, 994–998.
Levey, A. S., Bosch, J. P., Lewis, J. B., Greene, T., Rogers, N., & Roth, D. (1999). A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Annals of Internal Medicine, 130, 461–470.
Margolis, J. (1958). The kaolin clotting time; a rapid one-stage method for diagnosis of coagulation defects. Journal of Clinical Pathology, 11, 406–409.
Sugo, T., Kato, H., Iwanaga, S., Takada, K., & Sakakibara, S. (1985). Kinetic studies on surface-mediated activation of bovine factor XII and prekallikrein. Effects of kaolin and high-Mr kininogen on the activation reactions. European Journal of Biochemistry, 146, 43–50.
Politi, L., Aprile, A., Paganelli, C., Amato, A., Zoccai, G.B., Sgura, F., et al. (2010). Randomized clinical trial on short-time compression with kaolin-filled pad: a new strategy to avoid early bleeding and subacute radial artery occlusion after percutaneous coronary intervention. Journal of Interventional Cardiology, Aug 29. [Epub ahead of print].
Sena, M. J., Larson, S., Piovesan, N., & Vercruysse, G. (2010). Surgical application of kaolin-impregnated gauze (Combat Gauze) in severe hemorrhagic gastritis. The American Surgeon, 76, 774–775.
Nguyen, N., Hasan, S., Caufield, L., Ling, F. S., & Narins, C. R. (2007). Randomized controlled trial of topical hemostasis pad use for achieving vascular hemostasis following percutaneous coronary intervention. Catheterization and Cardiovascular Interventions, 69, 801–807.
Balzer, J. O., Schwarz, W., Thalhammer, A., Eichler, K., Schmitz-Rixen, T., & Vogl, T. J. (2007). Postinterventional percutaneous closure of femoral artery access sites using the Clo-Sur PAD device: initial findings. European Radiology, 17, 693–700.
Mlekusch, W., Minar, E., Dick, P., Sabeti, S., Bartok, A., Haumer, M., et al. (2008). Access site management after peripheral percutaneous transluminal procedures: Neptune pad compared with conventional manual compression. Radiology, 249, 1058–1063.
Palareti, G., Leali, N., Coccheri, S., Poggi, M., Manotti, C., D’Angelo, A., et al. (1996). Bleeding complications of oral anticoagulant treatment: an inception-cohort, prospective collaborative study (ISCOAT). Italian Study on Complications of Oral Anticoagulant Therapy. Lancet, 348, 423–428.
Patel, A. A., Clyne, C. A., Henyan, N. N., White, C. M., Zembrowski, B. F., Migeed, M., et al. (2007). The use of protamine after radiofrequency catheter ablation: a pilot study. Journal of Interventional Cardiac Electrophysiology, 18, 155–158.
Gianakos, S., Keeling, A. W., Haines, D., & Haugh, K. (2004). Time in bed after electrophysiological procedures (TIBS IV): a pilot study. American Journal of Critical Care, 13(56–58), 87.
Strandness, D. E., & Summer, D. S. (1975). Hemodynamics for Surgeons (pp. 120–157). New York: Grune & Stratton Inc.
Wazni, O. M., Beheiry, S., Fahmy, T., Barrett, C., Hao, S., Patel, D., et al. (2007). Atrial fibrillation ablation in patients with therapeutic international normalized ratio: comparison of strategies of anticoagulation management in the periprocedural period. Circulation, 116, 2531–2534.
Hussein, A. A., Martin, D. O., Saliba, W., Patel, D., Karim, S., Batal, O., et al. (2009). Radiofrequency ablation of atrial fibrillation under therapeutic international normalized ratio: a safe and efficacious periprocedural anticoagulation strategy. Heart Rhythm, 6, 1425–1429.
Schmidt, M., Segerson, N. M., Marschang, H., Akoum, N., Rittger, H., Clifford, S. M., et al. (2009). Atrial fibrillation ablation in patients with therapeutic international normalized ratios. Pacing and Clinical Electrophysiology, 32, 995–999.
Calkins, H., Brugada, J., Packer, D. L., Cappato, R., Chen, S. A., Crijns, H. J., et al. (2007). HRS/EHRA/ECAS expert Consensus Statement on catheter and surgical ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. A report of the Heart Rhythm Society (HRS) Task Force on catheter and surgical ablation of atrial fibrillation. Heart Rhythm, 4, 816–861.
Meyerovitz, M. F. (1990). How to maximize the safety of coronary and pulmonary angiography in patients receiving thrombolytic therapy. Chest, 97, 132S–135S.
Acknowledgments
We are grateful to the staff of the electrophysiological laboratory at Hiroshima University Hospital.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sairaku, A., Nakano, Y., Oda, N. et al. Rapid hemostasis at the femoral venous access site using a novel hemostatic pad containing kaolin after atrial fibrillation ablation. J Interv Card Electrophysiol 31, 157–164 (2011). https://doi.org/10.1007/s10840-011-9552-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-011-9552-6