Abstract
Background
Thrombocytopenia in chronic liver disease (CLD) typically reflects disease severity and may indicate an increased risk for bleeding.
Aims
To describe the longitudinal course of thrombocytopenia and risks for bleeding in veteran patients with non-hepatitis C-related CLD.
Methods
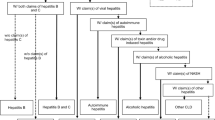
We identified 2,349 patients with non-hepatitis C-related CLD from databases of the New England Veterans Healthcare System between 1999 and 2008. The cohort was stratified by baseline platelet counts of <50,000, 50–100,000, > 100,000–150,000, and >150,000/μl. Primary outcomes were the incidence and hazard rates for bleeding episodes requiring hospitalization and incident severe thrombocytopenia (<50,000/μl).
Results
Over a median follow-up of 3.3 years (IQR 1.2, 6.3), incident major bleeds, predominantly gastrointestinal, occurred in 254 patients (10.8 % of the cohort) and in 19.9 % of those with baseline platelets <50,000/μl. Incident severe thrombocytopenia occurred in 315 patients (13.4 % of cohort) and in 40.7 % of those with baseline platelet counts between 50,000 and 100,000/μl. Baseline platelet counts between 50,000 and 100,000/μl independently predicted bleeding [adjusted HR 2.89 (1.76, 4.73) p < 0.001] as did esophageal varices, hemoglobin ≤9.9 g %, and INR 1.4–2.0. Incident severe thrombocytopenia and minimum platelet counts <25,000/μl each associated with bleeding episodes, but the average of minimum platelet counts recorded for those who bled was 76,000/μl.
Conclusions
Among veteran patients with non-hepatitis C-related CLD, baseline platelet counts of 50,000 to 100,000/μl increased subsequent risks for both incident severe thrombocytopenia and major bleeding events. Whereas associations between severe thrombocytopenia and bleeding most likely reflect CLD severity, liver-related coagulopathies, and co-morbid bleeding risks, interventions to enhance platelet production may be beneficial for such patients.



Similar content being viewed by others
References
Giannini EG. Review article: thrombocytopenia in chronic liver disease and pharmacologic treatment options. Aliment Pharmacol Ther. 2006;23:1055–1065.
Poordad F. Review article: thrombocytopenia in chronic liver disease. Aliment Pharmacol Ther. 2007;26(Suppl 1):5–11.
Afdhal N, McHutchison J, Brown R, et al. Review: thrombocytopenia associated with chronic liver disease. J Hepatol. 2008;48:1000–1010.
Udell JA, Wang CS, Tinmouth J, et al. Does this patient with liver disease have cirrhosis? JAMA. 2012;307:832–842.
Aster R. Pooling of platelets in the spleen: role in the pathogenesis of “hypersplenic” thrombocytopenia. J Clin Invest. 1966;45:645–657.
Bashour FN, Teran JC, Mullen KD. Prevalence of peripheral blood cytopenias (hypersplenism) in patients with nonalcoholic chronic liver disease. Am J Gastroenterol. 2000;95:2936–2939.
Giannini E, Botta F, Borro P, et al. Platelet count/spleen diameter ratio: proposal and validation of a non-invasive parameter to predict the presence of oesophageal varices in patients with liver cirrhosis. Gut. 2003;52:1200–1205.
Sorensen HT, Thulstrup AM, Mellemkjar L, et al. Long-term survival and cause-specific mortality in patients with cirrhosis of the liver: a nationwide cohort study in Denmark. J Clin Epidemiol. 2003;56:88–93.
D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217–231.
Peck-Radosavljevic M. Review article: coagulation disorder in chronic liver disease. Aliment Pharmacol Ther. 2007;26(Suppl 1):21–28.
Tripodi A, Mannucci PM. The coagulopathy of chronic liver disease. N Engl J Med. 2011;365:147–156.
Borowsky SA, Strome S, Lott E. Continued heavy drinking and survival in alcoholic cirrhotics. Gastroenterology. 1981;80:1405–1409.
Hermos JA. Drinking by alcoholic cirrhotic patients under medical care: a literature survey. Alcohol: Clin Exp Res. 1984;8:314–318.
Jepsen P, Ott P, Andersen PK, Sorensen HT, Vilstrup H. Clinical course of alcoholic liver cirrhosis: a Danish population-based study. Hepatology. 2010;51:1675–1682.
Vazali E, Aghemo A, Colombo M. A review of the treatment of chronic hepatitis C virus infection in cirrhosis. Clin Ther. 2010;32:2117–2138.
Louis KS, Micallef JM, Pimenta JM, Forssen UM. Prevalence of thrombocytopenia among patients with chronic hepatitis C: a systematic review. J Viral Hepatitis. 2011;18:1–7.
Lo Re V, Lim JK, Goetz MB, Tate J, Bathulapalli H, Klein MB et al. Validity of diagnostic codes and liver-related laboratory abnormalities to identify hepatic decompensation events in the Veterans Aging Cohort Study. Phamacoepidemiol Drug Safety 2011;20:689–699.
Pluta A, Gutkowski K, Sawka D. Thrombocytopenia in hepatitic C infection and chronic liver disease. Exp Clin Hepatol. 2009;5:15–19.
Roomer R, Hansen BE, Janssen HLA, de Knegt RJ. Thrombocytopenia and the risk of bleeding during treatment with peginterferon alfa and ribavirin for chronic hepatitis C. J Hepatol. 2010;53:455–459.
Nachnani JS, Rao GA, Bulchandani D, Pandya PK, Alba LM. Predictors of hematological abnormalities in patients with chronic hepatitis C treated with interferon and ribavirin. Ann Hematol. 2012;89:121–125.
Lin K-H, Hsu P-I, Kin C-K, et al. Factors linked to severe thrombocytopenia during antiviral therapy in patients with chronic hepatis C and pretreatment low platelet counts. BMC Gastroenterol. 2012;12:7.
McHutchison JG, Dusheiko G, Shiffman ML, et al. Eltrombopag for thrombocytopenia in patients with cirrhosis associated with hepatitis C. N Engl J Med. 2007;357:2227–2236.
Alverex GC, Gomez-Galicia D, Rodriguez-Fragoso L, et al. Danazol improves thrombocytopenia in HCV patients treated with peginterferon and ribavirin. Ann Hepatol. 2011;10:458–468.
Brown RS Jr. Review article: a pharmacoeconomic analysis of thrombocytopenia in chronic liver disease. Aliment Pharmacol Ther. 2007;26:41–48.
Poordad F, Theodore D, Sullivan J, Grotzinger K. Medical resource utilization in healthcare costs in patients with chronic hepatitis C viral infection and thrombocytopenia. J Med Econ. 2011;14:194–206.
Acknowledgments
The authors acknowledge the programming support of Galena Sokolovskaya. The study was supported by core funds of the VA Cooperative Studies Program, Massachusetts Veterans Epidemiologic Research and Information Center (MAVERIC), VA Boston Healthcare System, Boston, MA, and from GlaxoSmithKline, Philadelphia, PA.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hermos, J.A., Altincatal, A., Christian Weber, H. et al. Thrombocytopenia and Bleeding in Veterans with Non-hepatitis C-related Chronic Liver Disease. Dig Dis Sci 58, 562–573 (2013). https://doi.org/10.1007/s10620-012-2404-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2404-0