Abstract
Background
Radiofrequency atrial fibrillation ablation (AFA) is commonly performed in patients with atrial fibrillation. It is imperative to develop a strategy for the early detection of esophageal lesions secondary to AFA. The current protocol is to obtain cross-sectional imaging before and immediately after the procedure. If patients have evidence of esophageal inflammation, they undergo esophagogastroduodenoscopy (EGD). We hypothesized that esophageal abnormalities seen on imaging immediately post-ablation are a poor predictor of the damage seen during EGD.
Methods
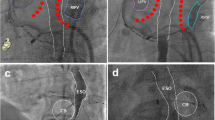
Patients referred for EGD following AFA from 1/2009 to 11/2010 were included. Two endoscopists reviewed and scored the EGD images. Two radiologists reviewed the post-AFA imaging studies. For computed tomography (CT) scans, esophageal inflammation was scored from 0 to 2. For T2 and delayed magnetic resonance imaging (MRI) pictures, esophageal enhancement was scored from 0 to 2, with the circumference involved as 0, <50%, or >50%, and the length of esophageal enhancement in mm.
Results
In total, 76 patients were included; 22 patients had only endoscopic images and 54 had both endoscopic and radiologic images for review. Of the post-AFA imaging studies, 16 were CTs and 60 were MRIs. The kappa score for the inter-rater agreement of esophageal inflammation on EGD was 0.4584 (moderate). For MRIs, the kappa scores for T2 images were 0.1980 and 0.2857 for edema and circumference, respectively. For delayed images, the kappa scores were 0.2687 and 0.3101 for edema and circumference, respectively. The kappa scores were negative between EGD score by T2 edema (−0.2104) and circumference (−0.2212), and between EGD score and delayed edema (−0.0588) and circumference (−0.0446). When measures were treated as dichotomous, the overall agreement between CT measures and EGD scores was kappa = 0, for T2 measures and EGD kappa = −0.2963, 95% confidence interval (CI) (−0.5643, −0.0282), and between delayed measures kappa = −0.0244, 95% CI (−0.1420, −0.0932).
Conclusions
There was no agreement between immediate imaging and the endoscopic findings of esophageal inflammation after AFA. A longer period of time between AFA and obtaining an imaging study may be useful in detecting patients with significant esophageal injury who should undergo EGD to assess for complications of AFA. Further studies are needed in order to determine the best modalities and optimal timing to detect post-AFA esophageal damage in an attempt to prevent the formation of atrial-esophageal fistulas.



Similar content being viewed by others
References
Rich MW. Epidemiology of atrial fibrillation. J Interv Card Electrophysiol. 2009;25:3–8.
Kneeland PP, Fang MC. Trends in catheter ablation for atrial fibrillation in the United States. J Hosp Med. 2009;4:E1–E5.
Cappato R, Calkins H, Chen SA, et al. Worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation. 2005;111:1100–1105.
Spragg DD, Dalal D, Cheema A, et al. Complications of catheter ablation for atrial fibrillation: incidence and predictors. J Cardiovasc Electrophysiol. 2008;19:627–631.
Takahashi A, Kuwahara T, Takahashi Y. Complications in the catheter ablation of atrial fibrillation: incidence and management. Circ J. 2009;73:221–226.
Ghia KK, Chugh A, Good E, et al. A nationwide survey on the prevalence of atrioesophageal fistula after left atrial radiofrequency catheter ablation. J Interv Card Electrophysiol. 2009;24:33–36.
Bunch TJ, Nelson J, Foley T, et al. Temporary esophageal stenting allows healing of esophageal perforations following atrial fibrillation ablation procedures. J Cardiovasc Electrophysiol. 2006;17:435–439.
Bahnson TD. Strategies to minimize the risk of esophageal injury during catheter ablation for atrial fibrillation. Pacing Clin Electrophysiol. 2009;32:248–260.
Martinek M, Bencsik G, Aichinger J, et al. Esophageal damage during radiofrequency ablation of atrial fibrillation: impact of energy settings, lesion sets, and esophageal visualization. J Cardiovasc Electrophysiol. 2009;20:726–733.
Halm U, Gaspar T, Zachäus M, et al. Thermal esophageal lesions after radiofrequency catheter ablation of left atrial arrhythmias. Am J Gastroenterol. 2010;105:551–556.
Badger TJ, Adjei-Poku YA, Burgon NS, et al. Initial experience of assessing esophageal tissue injury and recovery using delayed-enhancement MRI after atrial fibrillation ablation. Circ Arrhythm Electrophysiol. 2009;2:620–625.
Cappato R, Calkins H, Chen SA, et al. Prevalence and causes of fatal outcome in catheter ablation of atrial fibrillation. J Am Coll Cardiol. 2009;53:1798–1803.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gorman, D.R., Peterson, K.A., Fang, J. et al. Cross-Sectional Imaging Obtained Immediately Following Radiofrequency Atrial Fibrillation Ablation Does Not Predict Endoscopic Evidence of Esophageal Injury. Dig Dis Sci 56, 3453–3458 (2011). https://doi.org/10.1007/s10620-011-1829-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-011-1829-1