Abstract
Objectives
To assess the impact of cervical screening interval recommendations on cervical cancer incidence and mortality during periods of organized and opportunistic screening in Australia (2-yearly screening interval for organized screening), New Zealand (3 yearly interval for organized screening), and England (3/5 yearly interval for organized screening).
Methods
Changes in cervical cancer rates over two 10-year periods were assessed in each country among women aged 20–69 years using a standardized rate ratio (SRR). The SRR for opportunistic screening was calculated from 1973–1977 to 1983–1987 (mortality only), and for organized screening from 1993–1997 to 2003–2007 (mortality and incidence).
Results
During the period of opportunistic cervical screening, mortality reduced by 24 % in Australia and 10 % in England and Wales [Australia: SRR 0.76 (95 % CI 0.71–0.83); England and Wales: SRR 0.90 (95 % CI 0.87–0.93)]; no statistically significant reduction was observed in New Zealand [SRR 0.95 (95 % CI 0.82–1.11)]. After the introduction of organized screening, mortality reduced 39–45 % in each country [Australia: SRR 0.56 (95 % CI 0.51–0.62); New Zealand: SRR 0.53 (95 % CI 0.44–0.63); England and Wales: SRR 0.61 (95 % CI 0.58–0.64)], while incidence reduced 19–38 % [New Zealand: SRR 0.62 (95 % CI 0.56–0.69); Australia: SRR 0.64 (95 % CI 0.61–0.72); England: SRR 0.81 (95 % CI 0.78–0.83)].
Conclusion
In the era of opportunistic screening, some reductions were observed in cervical cancer mortality rates, but these were relatively modest and seen inconsistently between countries. After the introduction of organized cervical screening, cervical cancer mortality rates fell by a similar amount (~40 % or more) in all countries, and incidence fell by more than a third in Australia and New Zealand and by approximately one-fifth in England. Although several factors are likely to have influenced these observed reductions in cervical cancer rates, these findings do not support the more frequent 2-yearly cervical screening interval recommendation in Australia.
Similar content being viewed by others
Background
Organized screening was rolled out in England in 1998 and in Australia and in New Zealand in 1991 [1–3]. In these three countries, recent cervical cancer incidence and mortality rates are among the lowest worldwide. In 2007, the age-standardized incidence and mortality rates (all ages, standardized to the WHO world standard population) for Australia were 6.0 and 1.5 per 100,000, respectively, while for New Zealand they were 6.3 and 2.2 per 100,000, and for the United Kingdom (standardized to the European standard population) they were 7.5 (England alone) and 2.0 (England and Wales combined) [4–6]. These rates are lower than the GLOBOCAN estimated world average of 15.3 and 7.8 per 100,000 for incidence and mortality and also lower than the combined average rates of the more developed countries (9.1 and 3.1 per 100,000, respectively) [7].
In 1986, the International Agency for Research in Cancer (IARC) working group on Cervical Cancer Prevention synthesized data from eight countries [8]. Based on the analysis of the relative risk of invasive cervical cancer in screened versus unscreened women by time since last screen, the working group recommended that countries could safely adopt a 3-yearly rescreening interval for women aged between 20–30 and 60 years. Based on the results of an audit of cancer cases in England, this recommendation was updated in 2005, with an IARC working group concluding that a 3-yearly rescreening interval was safe for women aged 25–49 years, while the screening interval could be extended to 5-yearly rescreening for women aged 50–64 years [9, 10].
When the organized screening programs in New Zealand and the United Kingdom were implemented, a 3-yearly screening recommendation was adopted for women aged 20–69 and 20–64, respectively (and 5-yearly screening was also implemented in some regions in England), with England updating screening recommendations in 2003 to include age-dependent screening intervals, such that women aged 50–64 years had 5-yearly screening (as per the updated IARC recommendations) [1, 3, 11, 12]. By contrast, when Australia’s organized cervical screening program was introduced, a 2-yearly screening interval policy recommendation was adopted from 18 to 20 years (or from 1 to 2 years after sexual intercourse, whichever is later), up to age 69 years (conditional on the last two smears being negative in the previous 5 years) [2]. The Australian government recently announced a new review of the national cervical screening program, which will include a re-assessment of the recommended screening interval to ensure the policy is consistent with international best practice [13].
A previous study on cervical cancer incidence and mortality rates, which we published in 2007, reported relative reductions in the rate of cervical cancer incidence and mortality in the United Kingdom and Australia over two 7-year periods, before and after the introduction of organized screening in each country [14]. The findings suggested that the 2-yearly screening interval policy adopted in Australia had broadly similar effectiveness to the predominantly 3-yearly screening interval policy adopted in England, with both incidence and mortality rates falling by a third in the 7 years after the introduction of oranised screening in women aged 20–69 years in each setting. A subsequent modelled analysis of 2- versus 3-yearly screening concluded that these policies would have similar effectiveness in Australia [15]. The current study extends the previous analysis of incidence and mortality rates in two ways: firstly, by using new data to extend the period of time over which trends in cancer rates are assessed and secondly, by including data from an additional country, New Zealand. The aim was to confirm the findings of the prior analysis that 2- and 3-yearly screening policies have been associated with broadly similar reductions in cervical cancer incidence and mortality.
Methods
Cervical cancer case definition and sources
We used the International Classification of Disease (ICD) classification codes (ICD 10 code C53, ICD 9 code 180). Cervical cancer incidence and mortality data for Australia were obtained from the Australian Institute of Health and Welfare’s Australian Cancer Incidence and Mortality books [4]. For New Zealand, mortality and incidence data were obtained from the New Zealand Ministry of Health [5]. Mortality data for the United Kingdom were obtained from the WHO Mortality Database, which reports combined data for England and Wales [16]. Incidence data for England for years other than 1992–1995 were obtained from the Office of National Statistics (ONS) [17]. Because the ONS data for 1992–1995 represent rates in England and Wales combined, specific data for England for this period were obtained by direct request [18] [personal communication: N Jakomis, ONS, 2010].
Analysis of trends in cervical cancer rates
We assessed changes in cervical cancer incidence and mortality rates during the periods of opportunistic and organized cervical screening in each country. A 10-year period was defined for each period of opportunistic screening and organized screening; opportunistic screening was assessed over the period from 1973 to 1977 (average rate) to 1983–1987, and organized screening was assessed over the period from 1993–1997 to 2003–2007. Within each 10-year period, changes in cervical cancer incidence and mortality were assessed using a standardized rate ratio (SRR), which is the ratio of the average aggregated incidence (or mortality) rate at the beginning of the period relative to the average aggregated incidence (or mortality) rate at the end of the period [19]. The rates at the beginning and the end of each period were calculated as the aggregated number of cancer cases over a 5-year period divided by the population within the selected age-groups over the same 5-year period. Rates were then age-standardized to the Segi world population [20]. SRRs and 95 % CI were calculated for women aged 20–69 years and for women aged 20–49 years and 50–69 years. The rationale for subdividing the 20–69-year age-group is that this division has been previously used for analysis of screening interval and development of interval recommendations [9, 10]. For the analysis of trends in cervical cancer incidence, only data from the organized screening period were examined due to the lack of reliable incidence data for earlier years during which opportunistic screening was conducted.
Screening participation
To provide context to the analysis of trends in cervical cancer incidence and mortality, screening participation was described over the period of organized screening, over 2 (Australia)-, 3-, and 5–6-year periods (Australia, New Zealand, and England). In Australia, data on 2-yearly participation were reported from 1997 to 2008 and 3- and 5-year participation rates were reported from 2006 to 2008 [21]. In New Zealand, 3- and 6-yearly participation was reported from 2000 to 2007. In England, 3- and 5-yearly participation was reported from 1995 to 2008 [22–32]. From 2001, England reported participation over 3.5 and 5 years rather than over 3 and 5 years to allow for slightly delayed rescreening uptake [33]. Participation data, as reported, were already adjusted for hysterectomy rates in all countries.
Results
Trends in cervical cancer rates during the period of opportunistic screening
Prior to the introduction of organized screening, cervical cancer mortality rates were higher in New Zealand and England and Wales compared with Australia (Fig. 1). During the period of opportunistic screening, cervical cancer mortality had fallen 24 % in Australia (SRR 0.76, 95 % CI 0.71–0.83) and 10 % in England and Wales (SRR 0.90, 95 % CI 0.87–0.93) among women aged 20–69 years. No statistically significant change was observed in the same age-group of women in New Zealand (SRR 0.95, 95 % CI 0.82–1.11).
However, the findings for trends in cervical cancer mortality during the period of opportunistic screening differed by age-group (Fig. 2). Specifically, in women aged 20–49 years, cervical cancer mortality SRR increased by 35 % in New Zealand (SRR 1.35, 95 % CI 1.07–1.70) and 22 % in England and Wales (SRR 1.22, 95 % CI 1.15–1.30), while no statistically significant change was observed in this age-group in Australia (SRR 1.03, 95 % CI 0.89–1.18). By contrast, in women aged 50–69 years, cervical cancer mortality had fallen by 25–34 % in all three countries (Australia: SRR 0.66, 95 % CI 0.60–0.72; New Zealand: SRR 0.72, 95 % CI 0.59–0.87; England and Wales: SRR 0.75, 95 % CI 0.72–0.78).
Trends in cervical cancer rates during the period of organized screening
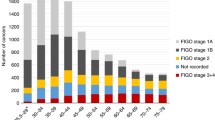
After the introduction of organized screening, the incidence of cervical cancer fell in all three countries (Fig. 3). Among women aged 20–69 years, the highest falls in incidence were observed in New Zealand (SRR 0.62; 95 % CI 0.56–0.69) and Australia (SRR 0.64, 95 % CI 0.61–0.72), compared to reductions in England (SRR 0.81; 95 % CI 0.78–0.83). In women aged 20–49 years, the fall in incidence was 36 % in New Zealand (SRR 0.64, 95 % CI 0.55–0.72) followed by 29 % in Australia (SRR 0.71, 95 % CI 0.67–0.76) and 13 % in the United Kingdom (SRR 0.87, 95 % CI 0.84–0.90). Among women aged 50–69 years, the fall in incidence was 43 % in Australia (SRR 0.57, 95 % CI 0.48–0.58), 41 % in New Zealand (SRR 0.59, 95 % CI 0.40–0.70), and 33 % in the United Kingdom (SRR 0.67, 95 % CI 0.64–0.71).
In contrast to the observed trends during the period of opportunistic screening, cervical cancer mortality fell by a similar magnitude across the overall age group in all three countries (Fig. 2). In women aged 20–69 years, cervical cancer mortality fell 44 % in Australia (95 % CI 0.51–0.62), 47 % in New Zealand (SRR 0.53, 95 % CI 0.44–0.63), and 39 % in England and Wales (SRR 0.61, 95 % CI 0.58–0.64). When the analysis was restricted to women aged 20–49 years, mortality fell 41 % in Australia (SRR 0.59, 95 % CI 0.51–0.69), 48 % in New Zealand (SRR 0.52, 95 % CI 0.39–0.69), and 41 % in England and Wales (SRR 0.59, 95 % CI 0.55–0.64). Similar patterns across countries were observed when the analysis was restricted to women aged 50–69 years; mortality fell in Australia by 47 % (SRR 0.53, 95 % CI 0.47–0.61), by 47 % in New Zealand (SRR 0.53, 95 % CI 0.41–0.69), and by 38 % in the United Kingdom (SRR 0.62, 95 % CI 0.58–0.66).
Screening participation
Figure 4 depicts the reported screening participation rates for each country. In Australia, the reported 2-yearly participation for women aged 20–69 years varied from 60 to 63 % over the period from 1991 to 2008; 3-yearly participation in the same age-group was recorded from 2006, and from 2006 to 2008 it varied from 73 to 74 %. In New Zealand, 3-yearly participation varied from 73 to 75 % from 2000 to 2007, and in England it varied from 69 to 70 % (over 3.5 years in age 25–64 years) from 2002 to 2008. In 2007, the reported 3/3.5-yearly participation was 74 %, 73 %, and 69 % in Australia, New Zealand, and England, respectively. In 2007, reported longer-term coverage rates were 86 % (5 years), 88 % (6 years), and 79 % (5 years) in Australia, New Zealand, and England, respectively. Overall, these data suggest that shorter (~3-yearly)- and longer (~5-yearly)-term screening participation rates have been broadly similar in Australia and New Zealand, with comparable but slightly lower participation rates observed in England.
a Shorter-term participation (2–3.5 years) in Australia, New Zealand, and England*. b Longer-term participation (5 and 6 years) in Australia, New Zealand, and England*. *Hysterectomy adjusted (Note that participation for England was calculated over 3.5 rather than over 3 years from 2001. Australian Institute of Health and Welfare has modified how it calculates the hysterectomy fraction from 2008 to 2009—see Appendix C of Cervical Screening in Australia 2009–2010. Method of calculating the fraction has changed from using self-report hysterectomy in 2001 to using National Hospital Morbidity Database)
Discussion
The aim of this analysis was to describe the trends in cervical cancer incidence and mortality in Australia, New Zealand, and England, over periods of time during which opportunistic and organized screening policies were in place. We sought to assess whether the relative reduction in cervical cancer incidence and mortality rates differed between Australia, which had a 2-yearly screening interval recommendation, and New Zealand and England, which had 3- or 3/5-yearly screening interval recommendations. We found that during the period of opportunistic screening (1973–1977 to 1983–1987), mortality rates decreased somewhat in women aged 20–69 years in Australia and England and Wales, but did not significantly change in New Zealand. However, it is notable that in the subset of women aged 20–49 years, mortality increased in New Zealand and in England and Wales, as previously reported [34]; this may have been due to several factors, potentially including increased exposure to human papillomavirus (HPV) infection in younger-age cohorts of women. In the period after the introduction of organized screening, we identified a more modest fall in cervical cancer incidence in women aged 20–49 years in England compared to the other two countries. This finding is consistent with that of Foley et al. [35], who recently examined incidence rates of cervical cancer in England over the period 1982–2006, concluding that from 1996 onwards, incidence rates were rising in 20–29-year-olds in most regions in England and incidence rates in women aged 30–39 years had mainly stabilised, and that in contrast, incidence declined markedly in those aged 40–79 years. However, trends in overall incidence rates include microinvasive cancers as well as frankly invasive disease, and importantly, we found that after the introduction of organized screening, mortality fell further in all three countries in the overall group of women aged 20–69 years, and in both younger and older groups of women (20–49 years; 50–69 years). The relative reduction in mortality rates over this period was similar in all three countries overall and in younger and older age-groups. The results of this study are broadly consistent with the findings of our prior analysis in which we found that cervical cancer incidence in women aged 20–69 years in Australia and the United Kingdom fell by 33 % in each country after the introduction of organized screening, between 1991–1993 and 1998–2000 (7 years) [14]. By including New Zealand in the comparison, as well as using a longer period of time to assess changes in incidence and mortality rates, the analysis presented here supports the conclusion of the prior study that the 2-yearly screening interval policy in Australia has had a broadly similar level of effectiveness as the predominantly 3-yearly screening interval policy in England and New Zealand.
Over the period of opportunistic screening, a reduction in cervical cancer mortality in women aged 20–69 years was observed in Australia and in England and Wales, but not in New Zealand. In European countries with opportunistic or more locally organized screening, reductions in cervical cancer mortality have been observed in France, Germany, Austria, Belgium, and Luxemburg [36]. After adjusting for uterine cancer deaths of unspecified origin in these settings, between 1970–1974 and 2000–2004 it was estimated that the age-standardized (world standard population) mortality rate fell from 6.3 to 2.0 per 100,000 in France, 7.4 to 2.2 per 100,000 in Germany, 10.3 to 2.2 per 100,000 in Austria, 6.1 to 2.6 per 100,000 in Belgium, and 8.4 to 1.5 per 100,000 in Luxemburg [37]. Therefore, in the European context, and as observed here for Australia and England and Wales, opportunistic screening resulted in some decrease in cervical cancer mortality. However, it has been noted that the reduction in mortality is highly dependent on participation and the quality of screening [37]. In our analysis, we observed that more substantial falls in cervical cancer mortality occurred after the introduction of organized screening, and these falls were more consistent across countries and across age-groups.
This ecological analysis has some limitations. Firstly, because organized screening began slightly earlier in England (1988) than in the other two countries (1991), there was a 3-year difference in the timing between the commencement of organized screening and the assessment of subsequent changes in England compared to the other two countries. In order to assess whether the delay had an impact on the findings, we conducted a sensitivity analysis that involved estimating rate reductions in the period from 1990–1992 to 2000–2002 (3 years earlier than the main analysis) [38]. As previously reported [14], we used data for five regional registries (Merseyside and Cheshire, North Western, Birmingham and West Midlands, Oxford, and Yorkshire) as a proxy for England as a whole [14]. In this analysis the SRR for incidence fell 42 % among women aged 20–69 years over this ‘shifted’ 10-year period, 37 % in women aged 20–49 years, and 52 % in women aged 50–69 years, similar to the observed rates over 10 years of organized screening in Australia and New Zealand. These findings therefore reinforce and strengthen the conclusion that the relative reductions in cervical cancer rates during the period of organized screening were similar in the three countries.
A second limitation of the current analysis was that we could not explicitly consider factors other than cervical cancer screening that may have influenced the observed cervical cancer incidence and/or mortality rates. Much of the analysis was based on grouped data, as the availability of individual unit record data is not in the public domain. Moreover, individual unit record data on factors that could affect observed incidence and mortality have not been collected at the national population level. With respect to mortality, other relevant factors may include differences in cervical cancer treatment practices [39], which may have varied over time and between countries, but the consistency of our findings for the similar levels of reduction in mortality across age-groups and in all countries after the introduction of organized screening strongly suggests that screening was a major driver. In this analysis, we also did not explicitly consider a potential change in exposure to HPV infection over time, or potential differences in the prevalence of cofactors that increase the risk of progression of HPV infection to invasive cervical cancer, such as long-term use of hormonal oral contraceptives (5+ years) [40], high parity and increased age at first full-term pregnancy [41], and tobacco smoking [42]. However, the overall rates of any contraceptive use in women aged 15–49 years in each country are available and have been reported as over 70 % in all three countries (82 % (1993) and 84 % (2002) in the United Kingdom; 76 % (1986) and 71 % (2002) in Australia; and 75 % in New Zealand (1995) [43]). The estimated fertility rate in each country was comparable and ranged between 1.8 and 2.2 in 1991, and 1.9 and 2.2 in 2008 [44, 45]. Reductions in tobacco consumption among males and females aged 15 years or older were observed between 1983 and 2003 in all countries, from 35 to 17 % in Australia, 35 to 27 % in the United Kingdom, and 33 to 25 % in New Zealand [46]. Although these data suggest some differences in the absolute levels of exposure to HPV cofactors, it is unlikely that these had a substantive impact on the relative reductions in cervical cancer incidence and mortality observed after the introduction of organized screening in all three settings.
A third limitation of the analysis is that although we found that recent participation rates in cervical screening were broadly comparable across the three countries, we could not explicitly account for differences in participation over time or other differences in cervical screening programs between countries and over time. These include differences in the management of women with abnormal screening results, variations in the screening technologies used, and differences in the organization of screening. In all three countries, women with high-grade cytology results were recommended for immediate referral to diagnostic evaluation, but there was some variation in the management of low-grade cytology between countries and over time. During the period under consideration, some changes in screening technology were implemented—liquid-based cytology (LBC) was introduced in England in 2003 (with HPV triage testing for low-grade cytology also recently implemented in 2011), and LBC with HPV triage testing was implemented in New Zealand from 2009 [47], whereas Australia continues to recommend the use of conventional cytology. However, because evidence to support increased sensitivity of LBC over conventional cytology in detecting high-grade CIN is limited [48], it is unlikely that the introduction of LBC in the United Kingdom and New Zealand had a substantial impact on the observed rates of invasive cervical cancer and mortality. We also did not explicitly consider the impact of the 2004 change to the recommended age of starting screening to 25 years in England, since our analysis considered broader age groups and trends over longer periods of time. However, other work has suggested that incidence trends in the youngest group (20–29 years) in England over the decade prior to 2009 are not related to the change to the age of starting screening [49].
With respect to the organization of screening, Australia and New Zealand have used a reminder-based letter system to indicate when a cytology test is overdue. In the United Kingdom, a call-and-recall invitation system is used in which proactive invitations to attend screening are sent to women. A previous study used data that suggested that in Australia and New Zealand, in which a reminder-based system is used, a higher proportion of women are screened before the recommended interval compared with a call-and-recall invitation system used in England [15]. Based on these findings, a modelled analysis predicted that if Australia adopted a 3-yearly screening interval, cervical cancer cases numbers and deaths would be similar under either a recommended 2- or 3-yearly screening interval. The current analysis found that 3/3.5- and 5/6-yearly participation was broadly similar between the three countries. Therefore, even though attendance at screening may have been somewhat less ‘efficient' in Australia and New Zealand in the past (and it should be noted that rates of early rescreening have reduced over time in both countries), similar rates of attendance over 3 and 5 years are likely to have driven similar effects on the observed trends in incidence and mortality rates for cervical cancer.
A final limitation of the analysis is that we did not explicitly consider the impact of treatment. However, in a prior ecological analysis by Taylor et al., the impact of primary and secondary prevention on trends in cervical cancer incidence, mortality, and survival was assessed in the context of New South Wales, Australia [50]. During the 1980s, access to free health care was thought to be associated with a shift in the stage of cervical cancers being detected, characterized by an increase in the proportion of localized cervical cancers. The stage shift in cervical cancer to more localized disease appeared to be associated with a decrease in mortality of 7 %. During the 1990s, organized cervical screening was rolled out. The period was characterized with stable overall survival between 1987 and 1991 (72 %) and 1994 and 2000 (73 %). However, organized screening led to an increase in the screening participation. With access to primary prevention and a concerted effort to target women at risk, an associated reduction in both cervical cancer incidence and mortality was observed. The reduction in cervical cancer incidence led to a further 20 % decrease in mortality, while survival remained stable. The main conclusion that can be drawn from the analysis by Taylor et al. is that the introduction of organized screening in New South Wales (as a proxy for Australia) resulted in concomitant reductions in both incidence and mortality, during a period of relatively stable survival.
Organized cervical screening programs in each of the three countries may undergo significant change over the next decade as a result of the introduction of prophylactic HPV vaccination, which was implemented in Australia in 2007 and in New Zealand and England in 2008. HPV vaccination will decrease the lifetime risk of invasive cervical cancer in vaccinated cohorts and will thus make current screening strategies less cost-effective; optimization of cervical screening in the post-vaccination era may eventually involve the introduction of primary HPV test technologies, further extension of the screening interval, and more targeted screening to women aged 25–30 years and older. Primary HPV testing is currently being considered in Australia as part of a current review (or ‘Renewal’) of the national cervical screening program [13], and primary HPV screening pilot evaluations are being configured in England [51] following the publication of the results of the ARTISTIC trial [52]. The results of several randomized controlled trials internationally have shown higher rates of detection of prevalent CIN2+ and CIN3+ in the initial round of screening with HPV compared to cytology, with lower rates of high grade precancerous disease detected in HPV-screened women in subsequent rounds [52–57]. The results suggest that screening intervals for HPV testing can be safely extended to at least 5 years, and this will be an important driver of the cost-effectiveness of future screening strategies in partially vaccinated populations. The current study has highlighted that screening more frequently than is optimal (as appears to be the case in Australia) does not deliver substantial marginal gains in effectiveness. The implementation and effective maintenance of even longer screening intervals in the context of primary HPV screening will be an important future challenge for screening policy-makers and programs.
Conclusion
In the era of opportunistic screening, some reductions were observed in cervical cancer mortality rates, but these were relatively modest and seen inconsistently between countries. After the introduction of organized cervical screening, cervical cancer mortality rates fell by a similar amount (~40 % or more) in all countries, and incidence fell by more than a third in Australia and New Zealand and by approximately one-fifth in England. Although several factors are likely to have influenced these observed reductions in cervical cancer rates, these findings do not support the more frequent 2-yearly cervical screening interval recommendation in Australia.
References
National Screening Unit (2011) National Cervical Screening Programme. New Zealand Government National Screening Unit. http://www.nsu.govt.nz/current-nsu-programmes/908.asp. Accessed 5th Feb 2011
Australian Government Department of Health and Ageing (2009) National Cervical Screening Program. Australian Government Department of Health and Ageing. http://www.cervicalscreen.health.gov.au/internet/screening/publishing.nsf/Content/cervical-about. Accessed 5th Feb 2011
Patnick J (2000) Cervical cancer screening in England. Eur J cancer (Oxford, England: 1990) 36(17):2205–2208
ACIM (Australian Cancer Incidence and Mortality) Books (2010) AIHW. http://www.aihw.gov.au/cancer/data/acim_books/index.cfm. Accessed 7th Feb 2011
Ministry of health data and statistics cancer: historical summary 1948–2007. Ministry of Health. http://www.moh.govt.nz/moh.nsf/indexmh/dataandstatistics-subjects-cancer-historicalsummary-1948-2007. Accessed Feb 2011
Office of National Statistics (2009) Cancer Statistics Registrations: registrations of cancer diagnosed in 2007, England. Series MB1 No. 38. Office of National Statistics, London, UK
GLOBOCAN 2008, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 10 [Internet] (2010) International agency for research on cancer. http://globocan.iarc.fr. Accessed 8th Aug 2010
IARC Working Group on Evaluation of Cervical Cancer Screening Programmes (1986) Screening for squamous cervical cancer: duration of low risk after negative results of cervical cytology and its implication for screening policies. IARC Working Group on evaluation of cervical cancer screening programmes. Br Med J (Clin Res Ed) 293 (6548):659–664
Cervix cancer screening/IARC Working Group on the Evaluation of Cancer Preventive Strategies (2005) Chapters 5–8: effectiveness of screening in populations; Summary; Evaluation; Recommendations. In, vol 10. IARC Press, Lyon, France, pp 201–241
Sasieni P, Adams J, Cuzick J (2003) Benefit of cervical screening at different ages: evidence from the UK audit of screening histories. Br J Cancer 89(1):88–93
Anttila A, Ronco G, (2009) Working Group on the Registration and Monitoring of Cervical Cancer Screening Programmes in the European Union within the European Network for Information on Cancer (EUNICE) Description of the national situation of cervical cancer screening in the member states of the European Union. Eur J cancer (Oxford, England: 1990) 45(15): 2685–2708
Anttila A, von Karsa L, Aasmaa A, Fender M, Patnick J, Rebolj M, Nicula F, Vass L, Valerianova Z, Voti L, Sauvaget C, Ronco G (2009) Cervical cancer screening policies and coverage in Europe. Eur J cancer (Oxford, England: 1990) 45(15):2649–2658
Australian Government: Department of Health and Ageing (2012) National Cervical Screening Program Renewal. Australian Government: Department of Health and Ageing. Accessed 2012
Canfell K, Sitas F, Beral V (2006) Cervical cancer in Australia and the United Kingdom: comparison of screening policy and uptake, and cancer incidence and mortality. Med J Aust 185(9):482–486
Creighton P, Lew JB, Clements M, Smith M, Howard K, Dyer S, Lord S, Canfell K (2010) Cervical cancer screening in Australia: modelled evaluation of the impact of changing the recommended interval from two to three years. BMC Public Health 10:734
World Health Organization (2010) WHO Mortality Database. WHO Statistical Information System. http://www.who.int/whosis/mort/download/en/index.html. Accessed Feb 2010
Office of National Statistics (1998–2008) Cancer Statistics: Registrations: Registrations of cancer diagnosed in 1992; 1993;1994; 1995-1997; 1998; 1999; 2003; 2004; 2005; 2006, England and Wales. vol Series MB1 No.: 25–30; 34–37 Office of National Statistics
Jakomis N (2010) Cancer incidences ENGLAND 1992–1994. Office of National Statistics, London
Boyle P, Parkin, DM (1991) Chapter 11: Statistical Methods for Registries. In: Jensen OM, Parkin, DM, MacLennan, R., Muir, CS., Skeet, RG. (ed) Cancer Registration: Principles and Methods. IARC Press, Lyon, France
Doll R, Payne P, Waterhouse JAH (1966) Cancer Incidence in five continents, vol I. Union Internationale Contre le Cancer, Geneva
Australian Institute of Health and Welfare (2009) Cervical Screening in Australia 2006–2007. Australian Institute of Health and Welfare Cat. No. CAN 43 Cancer Series Number 47, Canberra
Brewer N, McKenzie F, Wong KC, Ellison-Loschmann L (2009) National cervical screening programme annual monitoring report 2007, vol 26. Centre for Public Health Research, Massey University, NZ, Wellington, New Zealand
Brewer N, McKenzie F, Wong KC, Eillison-Loschmann L (2008) NCSP Annual Monitoring Report 2006, Centre for Public Health Research. Massey University, Wellington, New Zealand
Brewer N, McKenzie F, Wong KC, Eillison-Loschmann L (2007) NCSP annual monitoring report 2005. Centre for Public Health Research, Massey University, Wellington, New Zealand
Brewer N, McKenzie F, Travier N, Jeffreys M (2007) NCSP annual monitoring report 2004. Centre for Public Health Research, Massey University, Wellington, New Zealand
Coppell K (2003) NCSP annual monitoring report 2003. Wellington, New Zealand
Coppell K (2003) NCSP annual monitoring report 2002. Wellington, New Zealand
Coppell K, Cox B (2002) National cervical screening programme October–December 2001. Hugh Adam Cancer Epidemiology Unit University of Otago, Dunedin, New Zealand
Coppell K, Cox B (2001) National Cervical Screening Programme October–December 2000. Hugh Adam Cancer Epidemiology Unit University of Otago, Dunedin, New Zealand
Cervical Screening Programme, England 2009–10 (2010) http://www.ic.nhs.uk/statistics-and-data-collections/screening/cervical-screening/cervical-screening-programme-england-2009-10. Accessed Feb 2011
National Health Service Cancer Screening Programmes (2000) Reducing the risk: cervical screening programme 2000. NHS Cervical Screening Programme, National Health Service, Sheffield
Cervical Screening Programme, England 2004–5 (2005) The Health and Social Care Information Centre,. http://www.ic.nhs.uk/statistics-and-data-collections/screening/cervical-cancer/cervical-screening-programme-england-2004-05. Accessed Feb 2011
National Health Service Cancer Screening Programmes (2002) Building on experience: cervical screening programme 2002. NHS Cervical Screening Programme, National Health Service, Sheffield
Quinn M, Babb P, Jones J, Allen E (1999) Effect of screening on incidence of and mortality from cancer of cervix in England: evaluation based on routinely collected statistics. BMJ 318(7188):904–908
Foley G, Alston R, Geraci M, Brabin L, Kitchener H, Birch J (2011) Increasing rates of cervical cancer in young women in England: an analysis of national data 1982–2006. Br J Cancer 105(1):177–184
Arbyn M, Rebolj M, De Kok IM, Fender M, Becker N, O’Reilly M, Andrae B (2009) The challenges of organising cervical screening programmes in the 15 old member states of the European Union. Eur J cancer (Oxford, England: 1990) 45(15):2671–2678
Arbyn M, Raifu AO, Weiderpass E, Bray F, Anttila A (2009) Trends of cervical cancer mortality in the member states of the European Union. Eur J cancer (Oxford, England: 1990) 45(15):2640–2648
Ferlay J, Parkin, DM., Curado, MP., Bray, F., Edwards, B., Shin, HR., Forman, D (2010) Cancer Incidence in Five Continents, Volumes I to IX: IARC CancerBase No. 9. Accessed Feb 2011
Taylor RJ, Morrell SL, Mamoon HA, Wain GV (2001) Effects of screening on cervical cancer incidence and mortality in New South Wales implied by influences of period of diagnosis and birth cohort. J Epidemiol Commun Health 55(11):782–788
Appleby P, Beral V, Berrington de González A, Colin D, Franceschi S, Goodhill A, Green J, Peto J, Plummer M, Sweetland S, Cancer ICoESoC (2007) Cervical cancer and hormonal contraceptives: collaborative reanalysis of individual data for 16,573 women with cervical cancer and 35,509 women without cervical cancer from 24 epidemiological studies. Lancet 370 (9599):1609–1621
The International Collaboration of Epidemiological Studies of Cervical Cancer (2006) Cervical carcinoma and reproductive factors: collaborative reanalysis of individual data on 16,563 women with cervical carcinoma and 33,542 women without cervical carcinoma from 25 epidemiological studies. Int J Cancer 119(5):1108–1124
Appleby P, Beral V, Berrington de Gonzalez A, Colin D, Franceschi S, Goodill A, Green J, Peto J, Plummer M, Sweetland S (2006) Carcinoma of the cervix and tobacco smoking: collaborative reanalysis of individual data on 13,541 women with carcinoma of the cervix and 23,017 women without carcinoma of the cervix from 23 epidemiological studies. Int J Cancer 118(6):1481–1495
The World Bank (2011) The world bank data indicators: contraceptive prevalence (% of women ages 15–49). http://data.worldbank.org/indicator/SP.DYN.CONU.ZS. 2011
United Nations (2008) World Population Prospects: the 2008 revision and World Urbanization Prospects: the 2008 revision. http://esa.un.org/unpp/index.asp?panel=2
The World Bank (2011) The world bank data indicators: fertility rate, total (births per woman). http://data.worldbank.org/indicator/SP.DYN.TFRT.IN. 2011
Australian Institute of Health (2005) statistics on drug use in Australia 2004. Department of health and ageing, drug statistics series no. 15, Canberra
Legood R, Wolstenholme J, Gray A (2009) From cost-effectiveness information to decision-making on liquid-based cytology: mind the gap. Health Policy 89(2):193–200
Cervix cancer screening/IARC Working Group on the Evaluation of Cancer Preventive Strategies (2005) Chapter 2: Screening tests. In. IARC Handbooks of Cancer Prevention, vol 2, 10 edn. IARC Press, pp 59–117
Patel A, Galaal K, Burnley C, Faulkner K, Martin-Hirsch P, Bland MJ, Leeson S, Beer H, Paranjothy S, Sasieni P, Naik R (2012) Cervical cancer incidence in young women: a historical and geographic controlled UK regional population study. Br J Cancer 106(11):1753–1759
Taylor R, Morrell S, Mamoon H, Wain G, Ross J (2006) Decline in cervical cancer incidence and mortality in New South Wales in relation to control activities (Australia). Cancer causes control: CCC 17(3):299–306
Wise J (2012) Pilot study will assess whether HPV test should replace smears to screen for cervical cancer. BMJ 344:e3744
Kitchener HC, Gilham C, Sargent A, Bailey A, Albrow R, Roberts C, Desai M, Mather J, Turner A, Moss S, Peto J (2011) A comparison of HPV DNA testing and liquid based cytology over three rounds of primary cervical screening: extended follow up in the ARTISTIC trial. Eur J cancer (Oxford, England: 1990) 47(6):864–871
Mayrand MH, Duarte-Franco E, Rodrigues I, Walter SD, Hanley J, Ferenczy A, Ratnam S, Coutlee F, Franco EL (2007) Human papillomavirus DNA versus Papanicolaou screening tests for cervical cancer. N Engl J med 357(16):1579–1588
Anttila A, Kotaniemi-Talonen L, Leinonen M, Hakama M, Laurila P, Tarkkanen J, Malila N, Nieminen P (2010) Rate of cervical cancer, severe intraepithelial neoplasia, and adenocarcinoma in situ in primary HPV DNA screening with cytology triage: randomised study within organised screening programme. BMJ 340:c1804
Bulk S, Bulkmans NW, Berkhof J, Rozendaal L, Boeke AJ, Verheijen RH, Snijders PJ, Meijer CJ (2007) Risk of high-grade cervical intra-epithelial neoplasia based on cytology and high-risk HPV testing at baseline and at 6-months. Int J Cancer 121(2):361–367
Bulkmans NW, Berkhof J, Rozendaal L, van Kemenade FJ, Boeke AJ, Bulk S, Voorhorst FJ, Verheijen RH, van Groningen K, Boon ME, Ruitinga W, van Ballegooijen M, Snijders PJ, Meijer CJ (2007) Human papillomavirus DNA testing for the detection of cervical intraepithelial neoplasia grade 3 and cancer: 5-year follow-up of a randomised controlled implementation trial. Lancet 370(9601):1764–1772
Ronco G, Giorgi-Rossi P, Carozzi F, Confortini M, Dalla Palma P, Del Mistro A, Ghiringhello B, Girlando S, Gillio-Tos A, De Marco L, Naldoni C, Pierotti P, Rizzolo R, Schincaglia P, Zorzi M, Zappa M, Segnan N, Cuzick J (2010) Efficacy of human papillomavirus testing for the detection of invasive cervical cancers and cervical intraepithelial neoplasia: a randomised controlled trial. Lancet oncol 11(3):249–257
Acknowledgments
We thank Naomi Jakomis from the Office of National Statistics for provision of data on England incidence data.
Conflict of interest
KC is configuring a new trial of primary HPV screening in Australia which involves partial support from Roche Molecular Diagnostics, USA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Simonella, L., Canfell, K. The impact of a two- versus three-yearly cervical screening interval recommendation on cervical cancer incidence and mortality: an analysis of trends in Australia, New Zealand, and England. Cancer Causes Control 24, 1727–1736 (2013). https://doi.org/10.1007/s10552-013-0250-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-013-0250-9