Abstract
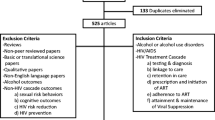
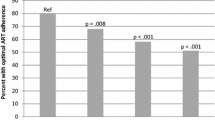
In a cohort of patients receiving care for HIV, we examined longitudinally the impact of past 30-day frequency of heavy drinking (consuming 5+ drinks on one occasion) on HIV-related (detectable viral load and CD4+ T cell count) and non-HIV-related (hemoglobin and biomarkers of kidney function and liver fibrosis) clinical outcomes and the extent to which these effects were due to reduced antiretroviral therapy (ART) adherence. Data came from the Study to Understand the Natural History of HIV/AIDS in the Era of Effective Therapy. Between March 2004 and June 2006, 533 individuals receiving ART were recruited and followed every 6 months for six years. Using longitudinal mediation analysis, we estimated natural direct effects (NDE) of heavy drinking frequency (never, 1–3 times, or 4+ times in the past 30 days) on clinical outcomes and natural indirect effects (NIE) mediated via ART adherence. A one-level increase in heavy drinking frequency had a significant negative NDE on CD4+ T-cell counts (-10.61 cells/mm3; 95 % CI [-17.10, -4.12]) and a significant NIE through reduced ART adherence of -0.72 cells/mm3 (95 % CI [-1.28, -0.15]), as well as a significant NIE on risk of detectable viral load (risk ratio = 1.03; 95 % CI [1.00, 1.05]). Heavy drinking had a significant detrimental NIE on a combined index of 5-year mortality risk and detrimental NDE and total effect on a biomarker of liver fibrosis. Heavy drinking has deleterious effects on multiple clinical outcomes in people living with HIV, some of which are mediated through reduced ART adherence.



Similar content being viewed by others
References
Centers for Disease Control and Prevention. Behavioral and clinical characteristics of persons receiving medical care for HIV infection—medical monitoring project, United States, 2013 cycle (June 2013–May 2014). HIV Surveillance Special Report 16. Jan 2016.
DeLorenze GN, Weisner C, Tsai AL, et al. Excess mortality among HIV-infected patients diagnosed with substance use dependence or abuse receiving care in a fully integrated medical care program. Alcohol Clin Exp Res. 2011;35:203–10.
Justice AC, McGinnis KA, Tate JP, et al. Risk of mortality and physiologic injury evident with lower alcohol exposure among HIV infected compared with uninfected men. Drug Alcohol Depend. 2016;161:95–103.
Chander G, Lau B, Moore RD. Hazardous alcohol use: a risk factor for non-adherence and lack of suppression in HIV infection. J Acquir Immune Defic Syndr. 2006;43:411–7.
Hendershot CS, Stoner SA, Pantalone DW, et al. Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr. 2009;52(2):180–202.
Braithwaite RS, McGinnis KA, Conigliaro J, et al. A temporal and dose response association between alcohol consumption and medication adherence among veterans in care. Alcohol Clin Exp Res. 2005;29(7):1190–7.
Cohn SE, Jiang H, McCutchan JA, et al. Association of ongoing drug and alcohol use with non-adherence to antiretroviral therapy and higher risk of AIDS and death: results from ACTG 362. AIDS Care. 2011;23(6):775–85.
Kalichman SC, Grebler T, Amaral CM, et al. Intentional non-adherence to medications among HIV positive alcohol drinkers: prospective study of interactive toxicity beliefs. J Gen Intern Med. 2013;28(3):399–405.
Samet JH, Cheng DM, Libman H, et al. Alcohol consumption and HIV disease progression. J Acquir Immune Defic Syndr. 2008;46(2):194–9.
Azar MM, Springer SA, Meyer JP, et al. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2010;112(3):178–93.
Shacham E, Agbebi A, Stamm K, et al. Alcohol consumption is associated with poor health in HIV clinic patient population: a behavioral surveillance study. AIDS Behav. 2011;15(1):209–13.
Marcellin F, Lions C, Winnock M, et al. Self-reported alcohol abuse in HIV-HCV co-infected patients: a better predictor of HIV virological rebound than physician’s perceptions (HEPAVIH ARNS CO13 cohort). Addiction. 2013;108(7):1250–8.
Baum MK, Rafie C, Lai S, et al. Alcohol use accelerates HIV disease progression. AIDS Res Hum Retrovir. 2010;26(5):511–8.
Justice AC, McGinnis KA, Skanderson M, et al. Towards a combined prognostic index for survival in HIV infection: the role of ‘‘non-HIV’’biomarkers. HIV Med. 2009;11:143–51.
Tate JP, Justice AC, Hughes MD, et al. An internationally generalizable risk index for mortality after one year of antiretroviral therapy. AIDS. 2013;27(4):563–72.
Justice, AC, Freiberg, MS, Tracy, R, the VACS Project team et al. Does an index composed of clinical data reflect effects of inflammation, coagulation, and monocyte activation on mortality among those aging with HIV? Clin Infect Dis. 2012;54(7):984–94.
Justice AC, Modur SP, Tate JP, et al. Predictive accuracy of the Veterans Aging Cohort Study index for mortality with HIV infection: a North American cross cohort analysis. J Acquir Immune Defic Syndr. 2013;62(2):149–63.
Wang EA, McGinnis KA, Long JB, et al. Incarceration and health outcomes in HIV-infected patients: the impact of substance use, primary care engagement, and antiretroviral adherence. Am J Addiction. 2015;24(2):178–84.
Carton JA, Collazos J, de la Fuente B, et al. Factors associated with liver fibrosis in intravenous drug users coinfected with HIV and HCV. Antivir Ther. 2011;16(1):27–35.
Fuster D, Tsui JI, Cheng DM, et al. Impact of lifetime alcohol use on liver fibrosis in a population of HIV-infected patients with and without hepatitis C coinfection. Alcohol Clin Exp Res. 2013;37(9):1527–35.
Muga R, Sanvisens A, Fuster D, et al. Unhealthy alcohol use, HIV infection and risk of liver fibrosis in drug users with hepatitis C. PLoS One. 2012;7(10):e46810.
Lim JK, Tate JP, Fultz SL, et al. Relationship between alcohol use categories and noninvasive markers of advanced hepatic fibrosis in HIV-infected, chronic hepatitis C virus-infected, and uninfected patients. Clin Infect Dis. 2014;58(10):1449–58.
Chaudhry AA, Sulkowski MS, Chander G, et al. Hazardous drinking is associated with an elevated aspartate aminotransferase to platelet ratio index in an urban HIV-infected clinical cohort. HIV Med. 2009;10(3):133–42.
Tsui JI, Cheng DM, Libman H, et al. Risky alcohol use and serum aminotransferase levels in HIV-infected adults with and without hepatitis C. J Stud Alcohol Drugs. 2013;74(2):266–70.
Blackard JT, Welge JA, Taylor LE, et al. HIV mono-infection is associated with FIB-4—A noninvasive index of liver fibrosis—in women. Clin Infect Dis. 2011;52(5):674–80.
Schaeffner ES, Kurth T, de Jong PE, et al. Alcohol consumption and the risk of renal dysfunction in apparently healthy men. Arch Intern Med. 2005;165:1048–53.
Funakoshi Y, Omori H, Onoue A, et al. Association between frequency of drinking alcohol and chronic kidney disease in men. Environ Health Prev Med. 2012;17(3):199–204.
Milman N, Pedersen AN. Blood haemoglobin concentrations are higher in smokers and heavy alcohol consumers than in non-smokers and abstainers: should we adjust the reference range? Ann Hematol. 2009;88(7):687–94.
Whitehead TP, Clarke CA, Bayliss RI, et al. Mean red cell volume as a marker of alcohol intake. J R Soc Med. 1985;78(10):880–1.
Vellozzi C, Brooks J, Bush T, and the SUN Study Investigators et al. The study to understand the natural history of HIV and AIDS in the era of effective therapy (SUN.Study). Am J Epidemiol. 2009;169(5): 642–52.
Sterling RK, Lissen E, Clumeck N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43:1317–25.
Vallet-Pichard A, Mallet V, Nalpas B, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. Comparison with liver biopsy and fibrotest. Hepatology. 2007;46:32–6.
Stevens LA, Coresh J, Greene T, et al. Assessing kidney function-measured and estimated glomerular filtration rate. N Engl J Med. 2006;354:2473–83.
Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. 1999;282(18):1737–44.
Valeri L, VanderWeele TJ. Mediation analysis allowing for exposure–mediator interactions and causal interpretation: Theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2):137–50.
Lange T, Hansen JV. Direct and indirect effects in a survival context. Epidemiology. 2011;22(4):575–81.
Imai K, Keele L, Yamamoto T. Identification, inference and sensitivity analysis for causal mediation effects. Stat Sci. 2010;25(1):51–71.
VanderWeele TJ. Marginal structural models for the estimation of direct and indirect effects. Epidemiology. 2009;20(1):18–26.
Pearl, J. Direct and indirect effects. In: Proceedings of the seventeenth conference on uncertainty in artificial intelligence. 2001: pp. 411–20.
Robins JM, Greenland S. Identifiability and exchangeability for direct and indirect effects. Epidemiology. 1992;13(2):143–55.
Little RJ, Rubin DB. Statistical analysis with missing data. Hoboken: Wiley; 2002.
Daniels MJ, Hogan JW. Missing data in longitudinal studies: Strategies for Bayesian modeling and sensitivity analysis. Boca Raton: Chapman and Hall/CRC Press; 2008.
Pellowski JA, Kalichman SC, Kalichman MO, Cherry C. Alcohol-antiretroviral therapy interactive toxicity beliefs and daily medication adherence and alcohol use among people living with HIV. AIDS Care. 2016:1–8.
Eken A, Ortiz V, Wands JR. Ethanol inhibits antigen presentation by dendritic cells. Clin Vaccine Immunol. 2011;18(7):1157–66.
Szabo G, Mandrekar P, Dolganiuc A, Catalano D, Kodys K. Reduced alloreactive T-cell activation after alcohol intake is due to impaired monocyte accessory cell function and correlates with elevated IL-10, IL-13, and decreased IFNgamma levels. Alcohol Clin Exp Res. 2001;25(12):1766–72.
Barr T, Helms C, Grant K, Messaoudi I. Opposing effects of alcohol on the immune system. Prog Neuropsychopharmacol Biol Psychiatry. 2016;65:242–51.
Fuster D, Cheng DM, Quinn EK, et al. Chronic hepatitis C virus infection is associated with all-cause and liver-related mortality in a cohort of HIV-infected patients with alcohol problems. Addiction. 2014;109(1):62–70.
Skjelbakken T, Wilsgaard T, Forde OH, et al. Haemoglobin predicts total mortality in a general young and middle-aged male population. The Tromso Study. Scand J Clin Lab Invest. 2006;66(7):567–76.
Hasin DS, Aharonovich E, O’Leary A, et al. Reducing heavy drinking in HIV primary care: a randomized trial of brief intervention, with and without technological enhancement. Addiction. 2013;108(7):1230–40.
Chander G, Hutton HE, Lau B, Xu XQ, McCaul ME. Brief intervention decreases drinking frequency in hiv-infected, heavy drinking women: Results of a randomized controlled trial. JAIDS. 2015;70(2):137–45.
Funding
This work was supported by the Centers for Disease Control and Prevention contract numbers 200-2002-00,610, 200-2002-00611, 200-2002-00612, 200-2002-00613, 200-2007-23633, 200-2007-23634, 200-2007-23635, and 200-2007-23636. Additional support was provided by grant number P01 AA019072 from the National Institute on Alcohol Abuse and Alcoholism, grant number T32 DA016184 from the National Institute on Drug Abuse, and the Lifespan/Tufts/Brown Center for AIDS Research (CFAR) grant number P30 AI042853.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Disclaimer
The findings and conclusions from this review are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Nur Onen—Deceased.
Rights and permissions
About this article
Cite this article
Kahler, C.W., Liu, T., Cioe, P.A. et al. Direct and Indirect Effects of Heavy Alcohol Use on Clinical Outcomes in a Longitudinal Study of HIV Patients on ART. AIDS Behav 21, 1825–1835 (2017). https://doi.org/10.1007/s10461-016-1474-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1474-y