Abstract
This randomized controlled trial tested the efficacy of an HIV prevention intervention to increase condom use and HIV testing among Spanish-speaking, heterosexually active immigrant Latino men. A community-based participatory research partnership developed the intervention and selected the study design. Following baseline data collection, 142 immigrant Latino men were randomized to the HIV prevention intervention or the cancer education intervention. Three-month follow-up data were collected from 139 participants, for a 98% retention rate. Mean age of participants was 31.6 years and 60% reported being from Mexico. Adjusting for baseline behaviors, relative to their peers in the cancer education comparison, participants in the HIV prevention intervention were more likely to report consistent condom use and receiving an HIV test. Community-based interventions for immigrant Latino men that are built on state of the art prevention science and developed in partnership with community members can greatly enhance preventive behaviors and may reduce HIV infection.
Resumen
Este estudio controlado y aleatorizado evaluó la eficacia de una intervención de prevención del VIH para incrementar el uso del condón y de pruebas del VIH entre inmigrantes latinos heterosexuales activos hispanohablantes. Una colaboración de investigación participativa basada en la comunidad desarrolló la intervención y seleccionó el diseño del estudio. De acuerdo a una recopilación inicial de datos, 142 hombres latinos inmigrantes fueron asignados de forma aleatoria a la intervención de prevención del VIH o a la intervención de educación sobre cáncer. Se realizó una recopilación de datos a los tres meses a 139 participantes, con un índice de retención de 98%. La edad promedio de los participantes fue de 31.6 años y 60% reportó ser originario de México. Tomando en consideración los comportamientos en la evaluación inicial, en relación con sus pares en la comparación con educación sobre cáncer, los participantes en la intervención de prevención del VIH reportaron más probabilidad de uso consistente del condón y pruebas de VIH. Intervenciones basadas en la comunidad para inmigrantes latinos hombres realizadas utilizando ciencia de última generación y desarrollada en colaboración con miembros de la comunidad pueden cuantiosamente incrementar comportamientos preventivos y reducir infección por el VIH.
Similar content being viewed by others
Introduction
Although Texas, California, New York, and Florida have experienced a large influx of Latino immigrants, recent trends in immigration patterns have resulted in changing demographics in the southeastern United States (US). Currently, North Carolina (NC) has one of the fastest growing Latino populations in the United States [1]. Immigrants to the Southeast are more likely from rural communities in southern Mexico and Central America, as opposed to those who traditionally immigrated to the US and were from northern regions of Mexico. Besides farmwork, including agriculture and poultry processing, many immigrants in the southeastern US work in furniture manufacturing, construction, and service industries [2–8].
Latinos in the US continue to be disproportionately impacted by the HIV/AIDS epidemic. Latinos have the second highest rate of AIDS diagnoses of all racial and ethnic groups. Latinos accounted for nearly 20% of the total number of new AIDS cases reported each year—over three times greater than that for non-Latino whites [9]. Rates of reportable sexually transmitted diseases (STDs) also are higher among Latinos than among non-Latino whites. Gonorrhea, chlamydia, and syphilis rates are two to four times higher among Latinos than among non-Latino whites [10]. Many southeastern states, including NC, consistently lead the nation in reported cases of AIDS, gonorrhea, chlamydia, and syphilis [6, 9, 10].
A complex combination of factors contribute immigrant Latinos’ HIV vulnerability, including language (not speaking English), a lack of understanding of HIV transmission and prevention strategies and of available healthcare services [3, 11–15], attitudes and beliefs that may not support safer sex [3, 4, 16–20], and discomfort with talking about sex among partners and with healthcare providers [3, 14, 21–23].
Gender role socialization prescribes that men must avoid “feminine behaviors,” be perceived as powerful, be and appear dominant, and prove their manhood by taking risks. This often is called “machismo” [24, 25]. Having multiple partners or sex with sex workers may imply masculinity. Engaging in risk may affirm some immigrant Latino men’s masculinity while using condoms may be perceived as being weak [3, 4]. Furthermore, poverty, harsh labor conditions, and racial discrimination may challenge Latino self-image and traditional values [5, 21, 25]. Immigrants must cope with conflicting cultural and social norms and expectations while attempting to adjust to life in a new country [4, 11, 26–29]. Norms and expectations, including those related to sexual behavior and gender roles (whether “positive” or “negative”, “healthy” or “unhealthy”) may be challenged [13, 30, 31], and for some, the subsequent stress and depression may result in higher rates of risk behavior and, as a consequence, increased rates of HIV and STDs [18, 20, 32, 33].
Loneliness associated with social isolation resulting from immigration also may contribute to risk behaviors, including increased alcohol consumption and episodic binge drinking that may lead to sexual risk. Many men leave their families and support networks and come to the US. Missing their families and communities coupled with finding themselves in challenging living situations may further lead to risk behavior [4, 17, 34–38].
Moreover, undocumented Latinos report fearing discovery and deportation and thus avoid formal systems of health care, which reduce the likelihood of exposure to preventive education and access to healthcare services [3, 4, 32, 39, 40]. They also may distrust the healthcare system and providers [3, 41]. Limited clinic hours, lack of bilingual and bicultural resources and insufficient public transportation also may adversely affect access to HIV prevention resources (e.g., condoms, counseling, testing, care, and treatment) [3, 17, 21, 32, 42].
Furthermore, immigrant Latinos coming to the southeastern US are arriving in communities that lack bilingual service provision and other infrastructures to meet their needs. These communities also have a history of anti-immigration sentiment [3, 11, 43, 44].
Although further research is needed to more fully understand the factors influencing HIV risk among immigrant Latinos, the current state of knowledge offers potential leverage points for intervention designed to reduce sexual HIV risk behaviors. These include (a) increasing knowledge of HIV/AIDS, effective prevention strategies, and how to access healthcare services in local communities; (b) recognizing, exploring, and addressing issues of sexual silence, gender role socialization and masculinity, and immigration; (c) building skills in communication, safer sex negotiation, and condom use; (d) building supportive networks within immigrant Latino communities; and (e) working with systems of health care to reduce barriers to access, build trust, and meet the healthcare needs of immigrant Latinos.
Despite the impact HIV and STDs are having on Latino populations, few resources exist to contribute to reducing and eliminating disparities in adverse sexual health outcomes experienced by this vulnerable population. Although interventions exist that provide insight into HIV prevention interventions for Latino men (e.g., VOICES/VOCES [45] and Modelo de Intervención Psicomédica (MIP; [46]), there are no community-based behavioral interventions with evidence of efficacy in reducing sexual risk of Spanish-speaking heterosexually active immigrant Latino men in the US. Most immigrant Latinos in the southeastern US are at sexual risk for HIV; injecting-drug use is not a prevalent mode of transmission [6, 47]. Thus, our community-based participatory research (CBPR) partnership in NC responded to the need and desire for HIV prevention interventions among immigrant Latino men living in rural NC. The objective of this study was to test whether participants randomized to a small-group HIV prevention intervention increased condom use and HIV testing when compared to their peers randomized to a cancer education comparison intervention.
Methods
Community-Based Participatory Research (CBPR)
CBPR has emerged as a viable approach to research to equitably involve community members, organizational representatives, and academic researchers in all phases of the research endeavor [48, 49]. Among CBPR’s benefits, the involvement of representatives from each group ensures more informed understanding of health-related phenomena from various perspectives and the development of interventions that are more likely to be effective.
Our CBPR partnership, which has been previously described [49–51], developed an intervention known as HoMBReS-2: Hombres Manteniendo Bienestar y Relaciones Saludables-2 (Men-2: Men Maintaining Wellbeing and Healthy Relationships-2). Based on the successes of the original HoMBReS intervention that used a lay health advisor (LHA) approach to HIV prevention, harnessing an existing soccer league in rural NC as a community resource [3, 52–54], HoMBReS-2 was designed as a small-group intervention with four modules designed to increase condom use and HIV testing among heterosexually active immigrant Latino men.
Study Design
During the process of implementing and evaluating the original HoMBReS intervention, members of the CBPR partnership increased their understanding of the power of scientific evidence to guide policy, specifically HIV prevention funding priorities. The dearth of interventions designed to meet the priorities and needs of immigrant Latinos in the Southeast motivated the CBPR partnership to develop HoMBReS-2 and test it using a randomized controlled trial (RCT) design. Thus, a two-arm RCT was conducted with baseline data collection and a single follow-up assessment 3 months after the intervention was delivered.
Human subject oversight was provided by the Institutional Review Board of Wake Forest University Health Sciences.
Participants and Recruitment
Inclusion criteria for study participants were: self-identifying as Latino or Hispanic; being native Spanish speaking; being ≥18 years of age; self-identifying as male; and providing informed consent. Exclusion criterion was having participated in HIV prevention interventions (e.g., the original HoMBReS intervention [52]) previously. Study team members distributed recruitment materials and approached and screened Latino men for eligibility in tiendas (small Latino community-focused grocers), laundromats, businesses that employ large numbers of Latinos (such as poultry plants, construction sites, and hotels), sports leagues, English as a Second Language (ESL) classes, housing communities and apartment complexes, and Latino restaurants throughout rural central NC.
After potential participants were identified and screened, study team members scheduled a meeting to complete informed consent procedures and baseline assessments. Participants entered the study in waves that averaged 20 participants per wave rather than the entire cohort to avoid delays between recruitment, randomization, and intervention delivery. Each participant was randomized by his selecting an envelope that contained an appointment card including the date(s), time(s), and location of their intervention (either HIV prevention intervention or cancer education intervention); 15 HIV prevention intervention cards and 15 cancer education cards were included in each wave because recruitment occurred in the community and sometimes with groups of men.
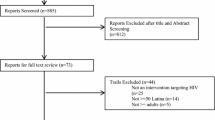
A sample size of 120 was determined a priori based on condom use power calculations established using previously reported condom use among immigrant Latino in NC [55]. However, because of community interest in participating in both the HIV prevention intervention and the cancer education comparison, a sixth wave was implemented for a total of 142 study participants. Of the 145 men screened, all met inclusion criteria and 142 elected to enroll in the study, yielding a 98% participation rate. See Fig. 1 for participant allocation and retention.
Data Collection
Data were collected privately in the offices of CBPR partners and in the homes of participants by native Spanish-speaking male study team members. All data were collected using the interviewer-administered assessment. Audio Computer Assisted Self-Interview (ACASI) was not used given formative data [3, 56, 57] and feedback from partnership members that suggested that participants were more likely to engage with a well-trained interviewer who could establish rapport and trust. This approach was thought to be culturally congruent given that some Latinos value personalismo, which is a cultural feature that tends to stress the importance of warm and friendly interactions and interpersonal engagement [58]. Furthermore, utilizing an interviewer-administered assessment overcame both poor literacy and vision (resulting from lack of access to vision services). Participants were paid $35.00 for the baseline and $55.00 for the 3-month follow-up assessments.
Measures
The assessment was comprised of 262 items based on self-report and required about 45–60 min to complete, depending on the skip patterns of each participant. Most items had predefined response options with binary, categorical, or Likert-scale response options to facilitate administration. Socio-demographic characteristics were assessed, including age, country of origin, educational attainment, employment status (employed year round, employed in seasonal work but not year round, and unemployed), income, and sexual identity. These items have been successfully used with immigrant Latinos in rural NC [52, 59].
Acculturation was measured using the Short Acculturation Scale for Hispanics, a 12-item scale with three subscales: respondent language use (alpha = 0.76); respondent media use (alpha = 0.85); and respondent ethnic social relations (alpha = 0.68) [60].
Knowledge of HIV transmission and prevention was assessed through the summation of correct responses to 18 true–false items [55] and knowledge of STD transmission and prevention was assessed through the summation of correct responses to 10 true–false items [55]. Other psychosocial mediators were assessed included mastery ([61]; alpha = 0.56), male role attitude ([62]; alpha = 0.67), condom use self-efficacy ([63]; alpha = 0.97), and condom use expectancies ([64]; alpha = 0.95).
Perceived AIDS-related stigma was measured using an established measure that has been found reliable in English, Xhosa, and Afrikaans [65]. The scale also had satisfactory internal reliability (alpha = 0.89) in this sample. Items were reverse coded as necessary so that higher scores indicated higher knowledge, mastery, male role attitude, condom use self efficacy and expectancies, acculturation, and AIDS-related stigma.
Behaviors related to HIV and STDs also were measured, including gender of sexual partners, type of sexual activity (vaginal and anal), and condom use. The first dependent variable for this evaluation was consistent condom use during vaginal or anal sex during the past 3 months. Participants were asked to report their frequency of condom use during the past 3 months with all partners on an ordinal scale of “always”, “most of the time”, “about half the time”, “once in awhile”, and “never” for vaginal and anal sex. Consistent condom use was coded as “always”. The second dependent variable was HIV testing during the past 12 months. These items have been successfully used with immigrant Latinos in rural NC [52, 59, 66].
Items that did not already exist in Spanish were translated into Spanish using a committee approach to translation that focuses on meaning and provides a process for iterative revision throughout the development process [67, 68]. A group of individuals with complementary skills, including translators (including native Spanish speakers from Mexico and Central America), a translation reviewer, content specialists, and a questionnaire design expert was convened. The translation was completed by multiple translators independently. The committee met to discuss versions of the translation; a reconciled version was created and reviewed and approved by the CBPR partnership.
Prior to administration, the assessment was pre-tested and revised to enhance comprehension, personal relevance, credibility, and acceptability.
Intervention Methods
The intervention was a small-group intervention designed to be interactive and activity-based. It included rapport and trusting building activities; didactic teaching; DVD segments that served as role modeling and triggers for discussion; role plays; group discussion; and skills building, practice, and feedback. It was based on social cognitive theory [69] and empowerment education [70], blended locally collected data on risk among heterosexually active Latino men [3, 4, 12, 52–54, 71], and addressed the priorities established by the CBPR partnership, including [1] increasing awareness of the magnitude of HIV and STD infections among Latinos in the US and NC; [2] providing information on types of infections, modes of transmission, sign and symptoms, and local counseling, testing, care, and treatment options; [3] increasing condom use; [4] bolstering the positive and reframe the negative aspects of what it means to be a man, a Latino man, and an immigrant Latino man; and [5] increasing the use of health care within an environment that lacks bilingual and bicultural services and within communities in which anti-immigration sentiment often is high [3]. The intervention is designed to build a foundation of knowledge about HIV, given that these immigrant Latinos have had very limited exposure to HIV information and have high levels of misconceptions [3, 4, 12, 14, 38, 52, 53]. The intervention also addresses the challenges immigrants face in the Southeast, a part of the country that lacks an established history of Latino immigration and the infrastructure to meet their needs. The abbreviated intervention modules and learning objectives are outlined in Table 1.
The intervention was peer led; three Latino men from rural NC were recruited and trained to serve as peer educators known as compañeros de salud. They were natural leaders within the community [72]. They were committed to developing their skills and positively impacting the health and wellbeing of immigrant Latino men like them within their communities; two had been former lay health advisors who had worked with soccer teams to promote condom use and HIV testing [52, 56]. All were native Spanish speakers; only one of the three spoke English, although limited. They were trained to implement the intervention by the study team.
The compañeros de salud were trained in four sessions. The training included the epidemiology of HIV and health disparities, HIV transmission, risk behavior, cultural and social influences on sexual health, access to healthcare services, predictors of behavior change, and group facilitation. The training was didactic and interactive and included role-playing exercises to provide opportunities to practice skills and receive feedback and suggestions to enhance their facilitation and communication skills.
One session also reviewed the study design and basic research concepts, including fidelity, bias, and evaluation, and human subjects protection. The compañeros de salud were evaluated pre- and post-training, and the results of these evaluations were used to tailor the training to their needs. The project coordinator and an observer were present during all intervention sessions to ensure fidelity.
A fourth compañero de salud was similarly selected and trained to implement the cancer education comparison intervention that was developed for this study by the CBPR partnership. To reduce potential contamination, he was not trained in the components of the HIV prevention intervention. The cancer education comparison intervention was delivered in one 2-h session and focused on prevention of cancers particularly relevant to men: prostate, lung, and colorectal cancers.
The HIV prevention and cancer education comparison interventions were implemented on Saturday and Sunday mornings within the community.
Data Analysis
Analyses were performed using an intent-to-treat protocol with participants analyzed in their assigned study arms from randomization irrespective of the number of sessions attended [73]. Six participants attended the incorrect arm, and again according to the intent-to-treat protocol, analyses were conducted based on the arm to which they were originally randomized. At baseline, descriptive statistics summarized demographic characteristics, psychosocial mediators, and risk behaviors between intervention and comparison arms. Differences between arms at baseline were assessed using Student’s t-tests or Wilcoxon rank sum tests for continuous variables and Chi-square or Fisher’s exact tests for categorical variables. Intervention differences were assessed using logistic regression on follow-up outcome measures after adjusting for baseline characteristics. Additional covariates were considered in multivariable modeling for increased precision of intervention effects. Included covariates in the multivariable model were chosen a priori based on theoretical considerations and literature review regarding factors that might affect condom use and HIV testing. Interaction effects were checked first after centering continuous variables and none were significant at the 0.10 level [74].
For sensitivity analyses regarding missing data, multiple imputation was used to impute missing data and compare these results to those in the complete-case analysis [75, 76]. We performed multiple imputation using chained equations (MICE) [77, 78]. Twenty imputed datasets were created and then pooled to account for the within and between imputation variation. All analyses were performed using SAS v9.2 (SAS Institute, Cary, NC) and Stata v11.1 (StataCorp, Inc, College Station, TX). A two-sided P-value <0.05 was considered to be statistically significant.
Results
Baseline
Of the 142 participants, 72 were randomized to the HIV prevention intervention and 70 to the cancer education intervention. All participants reported being from outside the US; all were Spanish speaking with limited English-language use. Mean age and consistent condom use differed between the intervention and comparison arms at baseline. No other differences between the arms were observed at baseline (see Table 2).
Quality Assurance and Attrition
Trained observers attended all study sessions to assess fidelity; 100% of the intervention activities were implemented with fidelity. Participant attendance was high; 80% (n = 58) of participants randomized to the HIV prevention intervention sessions attended all of the HIV prevention intervention sessions, and 91% of participants randomized to the cancer education intervention attended the one-session cancer education comparison intervention (n = 64). A total of three participants were lost to 3-month follow-up, two in the HIV prevention arm and one in the cancer prevention arm.
Intervention Effects
Intervention effects are presented in Table 3. At follow-up, participants in the HIV prevention intervention had significantly higher consistent condom use and HIV testing relative to participants in the cancer education arm. Specifically, adjusting only for baseline condom use, intervention participants had higher condom use during the past 3 months than those in the comparison arm (adjusted odds ratio [AOR] = 3.52; 95% confidence interval [CI] = 1.29–9.63; P = 0.014). Adjusting for baseline condom use and covariates, intervention participants had higher condom use during the past 3 months than those in the comparison arm (AOR = 11.2; 95% CI = 1.2–101.8; P = 0.032). Using multiple imputation to examine sensitivity of results to missing data, intervention participants had higher condom use during the past 3 months than those in the comparison arm when adjusting only for baseline condom use (AOR = 2.61; 95% CI = 1.07–6.34; P = 0.035), and when adjusting for baseline condom use and covariates (AOR = 3.87; 95% CI = 1.31–11.5; P = 0.015).
Adjusting only for baseline HIV testing, intervention participants had higher HIV testing during the past 12 months than those in the comparison arm (AOR = 5.18; 95% CI = 2.26–11.9; P < 0.001). Adjusting for baseline testing and covariates, intervention participants had higher HIV testing during the past 12 months than those in the comparison arm (AOR = 18.3; 95% CI = 3.59–92.9; P < 0.001). Again, examining sensitivity using multiple imputation, intervention participants had higher HIV testing during the past 12 months than those in the comparison arm when adjusting only for baseline HIV testing (AOR = 6.2; 95% CI = 2.83–13.6; P < 0.001), and when adjusting for baseline HIV testing and covariates (AOR = 9.51; 95% CI = 3.52–25.6; P < 0.001).
Discussion
This is the first RCT of a community-based small-group intervention designed to reduce sexual risk behaviors among heterosexually active immigrant Latino men to demonstrate efficacy. Analysis of self-reported data indicated that compared to their cancer education comparison peers, participants in the HIV prevention interventions were significantly more likely to report consistent condom use during the past 3 months and HIV testing during the past 12 months.
The HoMBReS-2 intervention was designed to be culturally congruent and gender specific. It was based on locally collected formative data; previous experiences with developing, implementing, and evaluating HIV prevention interventions; sound health behavior theories; and the real, lived experiences of immigrant Latinos living in rural NC. Although the intervention used language that could imply either female or male sexual partners, it was designed specifically for immigrant Latino men who had sex with female partners. However, it is noteworthy that although all participants reported sex with females in the previous 3 months, three self-identified as “gay/homosexual.” In discussions with the interventionists and review of observer’s notes, discussions of same-sex behavior by participants were not common; they were not completely absent either. Because the intervention was designed to address notions related to masculinity, there was some discussion of same-sex behavior.
Although a dismantling study would help identify the possible reasons the HoMBReS-2 intervention was efficacious, this intervention built on what is currently known about efficacious and effective HIV prevention interventions including [1] incorporating locally collected ethnographic data and tailoring to the defined audience (i.e., heterosexually active immigrant Latino men) to meet locally identified needs, [2] being gender specific (e.g., targeting men not both men and women), [3] having solid theoretical foundations (i.e., social cognitive theory and empowerment education), [5] discussing barriers to, and facilitators of, condom use and HIV testing, [6] exploring gender norms and expectations, [7] increasing awareness, knowledge, and positive attitudes and beliefs about risk reduction, [8] increasing risk reduction norms and social support for protection, [9] providing positive reinforcement for healthy behavior change, [10] skills building through role plays and practice, and [11] guidance on how to utilize available services [8, 79–84].
It has been suggested that four or more sessions may be key to HIV prevention interventions reducing risk; however, although this intervention included four modules and multiple sessions, it did not include four separate sessions. The success of this intervention may be attributable to a combination of factors, including the careful inclusion of what is known about HIV prevention interventions [79–86] as well as several other factors.
First, Latino men, who represent a new trend in immigration to the US, have identified HIV and STDs as health priorities. They want to learn about sexual health given the higher rates of disease when compared to other health concerns [3]. Cancer has been identified as a concern as well by immigrant Latino men in rural NC given the frequency cancer is mentioned within popular media. Second, the intervention was developed by a CBPR partnership that included community members (e.g., immigrant Latino men), organizational representatives, and academic researchers—all of whom worked together through an iterative and systematic intervention development process that helped to ensure that the intervention blended sound science with the lived experiences of immigrant Latino men. The development of the intervention and the study design were not imposed by academic researchers; rather, the intervention, its content and activities, and the study design were based on iterative negotiation among CBPR partners. Third, this CBPR partnership had successful experiences developing and implementing other HIV prevention interventions for Latinos and was able to build on lessons learned from these experiences to develop HoMBReS-2 [52, 54, 56]. For example, DVD segments were developed to add to the teaching modalities that the intervention harnessed. Fourth, HoMBReS-2 focused heavily on building condom use skills and included multiple activities to allow for skill development, practice, and correction. For example, condom use errors during initial condom skills activities were high; because this intervention did not focus on other risks (e.g., injecting-drug use), intervention content focused on activities to develop these skills. Fifth, an important component to the intervention included acknowledging the challenges that Latino men face in using condoms and being HIV tested. For example, a DVD segment followed a Spanish-speaking Latino man as he went through the actual testing process at a local health department. It showed the difficulties of getting an interpreter, the embarrassment of having a female interpreter and nurse, and types of questions that one is asked and the rationale behind the data that the health department or other testing sites collect.
Sixth, the HoMBReS-2 intervention was implemented by well-trained peer leaders from the community itself. Natural helper-led interventions, including those led by peers, are an important approach in health promotion and disease prevention [15, 72]. Peers can teach skills, model health-promoting behaviors, and serve as credible role models because they are from the community and they speak the same “language”. They understand the “real world”, practical challenges of change, and the risks individuals take when changing. Peers also can help change norms and expectations that influence behavior. They can offer social support for performance of desired behaviors and for avoidance of health-compromising behaviors. Little has been published about using a peer-led approach for HIV prevention among Latino men; another study using a peer approach was found to reduce risk indices using a one-sample pretest–posttest design [87]. This study offers evidence that immigrant Latino men can be effective serving as peer educators.
The Use of CBPR
This study was successful in recruiting a sample of 142 immigrant Latino men (participation rate = 98%) and retaining 98% of them at 3-month follow-up within communities in which publicity over partnerships between local law enforcement and US Immigration and Customs Enforcement and recent allegations that public health department records had been used in deportation proceedings have contributed to fears and general distrust among many immigrant Latinos. Within this socio-political environment, this population is even more difficult to access and suspicious of research [3, 44]. However, the trust that this CBPR partnership had in the local community, the prioritization of sexual health among Latino men, insights of the community partners, and the recruitment skills of the study team enabled this study to overcome these challenges. In fact, a sixth recruitment wave was implemented due to the local Latino community’s interest in both the HIV prevention and cancer education interventions.
Limitations
This study was conducted in NC among immigrant Latino men. Generalization of the findings to other Latino populations or contexts may not be appropriate. Although the demographics of Latinos immigrating to NC tend to represent those coming to the southeastern US more broadly, these assumptions have not been well tested particularly given the heterogeneity within Latino communities. Furthermore, the intervention was designed to reduce sexual risk given that injecting-drug use is not a prevalent mode of transmission among immigrant Latino men in NC [6, 47]. It was not designed to reduce risk through injecting-drug use. This study also relied on self-reported sexual behavior. However, self-reported behavior has been found to be reliable if collected carefully [88, 89]. Further research with a larger sample size could use biological outcomes to evaluate the intervention. This study also had a short follow-up period; longer studies must be initiated to explore maintenance and decay of behavior change over time.
The comparison intervention was not equivalent in the length, and future tests of this intervention should implement a comparison intervention that is more comparable in length. Furthermore, although the comparison compañero de salud was not trained in the HIV prevention intervention in order to reduce potential contamination, possible interventionist effects were not controlled using this approach. Similarly, data were not blinded, and despite randomization two significant baseline differences were observed (i.e., age and consistent condom use). These differences may reflect the small sample size and were controlled for statistically in evaluating intervention differences.
Finally, because they could not attend the intervention to which they were assigned and did not call the study telephone number to reschedule, six participants decided to go with someone they knew who had a session at a different day and/or time. Thus, they attended a different study arm from which they had been randomized. When these participants presented themselves to attend a session for the incorrect arm, study staff decided that it was better to maintain smooth community relations than turn them away, particularly given the need to maintain trust within this community. Participants did not prefer one study arm over the other; rather, they were relying on informal social networks to help them problem-solve when they had complications to study participation, just as they rely on informal networks to solve other problems they face, such as getting a car without documentation or finding a job [3, 53].
Conclusions
Glaring gaps exist in the current intervention arsenal available to reduce the risk of HIV among some vulnerable populations, including Latino populations [20, 80]. There is a dearth of culturally congruent interventions to prevent HIV. The HoMBReS-2 intervention is promising; it was found efficacious in increasing consistent condom use and HIV testing among a community-based sample of immigrant Latino men.
More rigorous study designs (e.g., a comparison intervention that is equivalent in length) and longer follow-up periods are necessary to explore the affects of the HIV prevention intervention and the maintenance of condom use and HIV testing behaviors. Moreover, determining whether this type of intervention can impact HIV-related behaviors of other Latino communities deserves exploration. For example, could this intervention serve as a foundation for other targeted or enhanced interventions to reduce risk among within other communities of heterosexually active Latino men, Latino farmworkers, Latino MSM, and/or Latina women.
References
US Census Bureau. 2008 American community survey data profile highlights: North Carolina fact sheet. Washington, DC: United States Department of Commerce; 2009.
Kasarda JD, Johnson JH. The economic impact of the Hispanic population on the state of North Carolina. Chapel Hill, NC: Frank Hawkins Kenan Institute of Private Enterprise; 2006.
Rhodes SD, Eng E, Hergenrather KC, Remnitz IM, Arceo R, Montano J, et al. Exploring Latino men’s HIV risk using community-based participatory research. Am J Health Behav. 2007;31(2):146–58.
Rhodes SD, Hergenrather KC, Griffith D, Yee LJ, Zometa CS, Montaño J, et al. Sexual and alcohol use behaviours of Latino men in the south-eastern USA. Cult Health Sex. 2009;11(1):17–34.
North Carolina Institute of Medicine. NC Latino health 2003. Durham, NC: North Carolina Institute of Medicine; 2003.
Southern State Directors Work Group. Southern states manifesto: update 2008. HIV/AIDS and sexually transmitted diseases in the south. Birmingham, AL: Southern AIDS Coalition; 2008.
Hayes-Bautista D. La Nueva California: Latinos in the golden state. Berkeley, CA: University of California; 2004.
Huedo-Medina TB, Boynton MH, Warren MR, Lacroix JM, Carey MP, Johnson BT. Efficacy of HIV prevention interventions in Latin American and Caribbean nations, 1995–2008: a meta-analysis. AIDS Behav. 2010;14(6):1237–51.
Centers for Disease Control and Prevention. HIV/AIDS surveillance report. Atlanta; 2009.
Centers for Disease Control and Prevention. Sexually transmitted disease surveillance, 2008. Atlanta, GA: U.S. Department of Health and Human Services; 2009.
Viadro CI, Earp JA. The sexual behavior of married Mexican immigrant men in North Carolina. Soc Sci Med. 2000;50(5):723–35.
Rhodes SD, Hergenrather KC, Wilkin A, Alegria-Ortega J, Montaño J. Preventing HIV infection among young immigrant Latino men: results from focus groups using community-based participatory research. J Natl Med Assoc. 2006;98(4):564–73.
Organista KC, Organista PB, Bola JR, Garcia de Alba JE, Castillo Moran MA. Predictors of condom use in Mexican migrant laborers: exploring AIDS-related knowledge, attitudes, and behaviors of female Mexican migrant workers. Am J Community Psychol. 2000;28(2):245–65.
Rhodes SD, Hergenrather KC, Zometa C, Lindstrom K, Montaño J. Characteristics of immigrant Latino men who utilize formal healthcare services in rural North Carolina: baseline findings from the HoMBReS study. J Natl Med Assoc. 2008;100(10):1177–85.
Albarracin J, Albarracin D, Durantini M. Effects of HIV-prevention interventions for samples with higher and lower percents of Latinos and Latin Americans: a meta-analysis of change in condom use and knowledge. AIDS Behav. 2008;12(4):521–43.
Marin BV, Gomez CA, Tschann JM, Gregorich SE. Condom use in unmarried Latino men: a test of cultural constructs. Health Psychol. 1997;16(5):458–67.
McQuiston C, Flaskerud JH. “If they don’t ask about condoms, I just tell them”: a descriptive case study of Latino lay health advisers’ helping activities. Health Educ Behav. 2003;30(1):79–96.
Zambrana RE, Cornelius LJ, Boykin SS, Lopez DS. Latinas and HIV/AIDS risk factors: implications for harm reduction strategies. Am J Public Health. 2004;94(7):1152–8.
Flaskerud JH, Uman G, Lara R, Romero L, Taka K. Sexual practices, attitudes, and knowledge related to HIV transmission in low income Los Angeles Hispanic women. J Sex Res. 1996;33(4):343–53.
Organista KC, Carrillo H, Ayala G. HIV prevention With Mexican migrants: review, critique, and recommendations. J AIDS. 2004;37(Supplement 4):S227–39.
Amaro H, Vega RR, Valencia D. Gender, context, and HIV prevention among Latinos. In: Aguirre-Molina M, Molina CW, Zambrana RE, editors. Health issues in the Latino community. San Francisco, CA: Jossey-Bass; 2001. p. 301–24.
Marin BV. HIV prevention in the Hispanic community: sex, culture, and empowerment. J Transcult Nurs. 2003;14(3):186–92.
Cashman R, Eng E, Siman F, Rhodes SD. Exploring the sexual health priorities and needs of immigrant Latinas in the southeastern US: a community-based research approach. AIDS Educ Prev. In press.
Rothenberg BA. Understanding and working with parents and children from rural Mexico: What professionals need to know about child-rearing practices, the school experience, and health concerns. Menlo Park, CA: The CHC Center for Child and Family Development Press; 1995.
Ramirez RL, Garcia-Toro VI, Velez-Galvan ML, Cunningham I. Masculine identities and sexuality: A study of Puerto Rican blue-collar workers. In: Ramirez RL, Garcia-Toro VI, Cunningham I, editors. Caribbean masculinities: working papers. San Juan, PR: HIV/AIDS Research and Education Center (CIEVS); 2002. p. 83–103.
Organista KC. Solving Latino psychosocial and health problems: theory, practice, and populations. Hoboken, NJ: John Wiley and Sons; 2007.
Sabogal F, Catania JA. HIV risk factors, condom use, and HIV antibody testing among heterosexual Hispanics: the National AIDS Behavioral Surveys (NABS). Hisp J Behav Sci. 1996;18(3):367–91.
Takahashi LM. Stigmatization, HIV/AIDS, and communities of color: exploring response to human service facilities. Health Place. 1997;3(3):187–99.
Talashek ML, Peragallo N, Norr K, Dancy BL. The context of risky behaviors for Latino youth. J Transcult Nurs. 2004;15(2):131–8.
Pulerwitz J, Amaro H, De Jong W, Gortmaker SL, Rudd R. Relationship power, condom use and HIV risk among women in the USA. AIDS Care. 2002;14(6):789–800.
Salabarria-Pena Y, Lee JW, Montgomery SB, Hopp HW, Muralles AA. Determinants of female and male condom use among immigrant women of Central American descent. AIDS Behav. 2003;7(2):163–74.
Aranda-Naranjo B, Gaskins S. HIV/AIDS in migrant and seasonal farm workers. J Assoc Nurses AIDS Care. 1998;9(5):80–3.
Williams DR. The health of men: structured inequalities and opportunities. Am J Public Health. 2003;93(5):724–31.
Buescher PA. A review of available data on the health of the Latino population in North Carolina. N C Med J. 2003;64(3):97–105.
Kim-Godwin YS, Bechtel GA. Stress among migrant and seasonal farmworkers in rural southeast North Carolina. J Rural Health. 2004;20(3):271–8.
Shedlin MG, Decena CU, Oliver-Velez D. Initial acculturation and HIV risk among new Hispanic immigrants. J Natl Med Assoc. 2005;97(7 Suppl):32S–7S.
Parrado EA, Flippen C. Community attachment, neighborhood context, and sex worker use among Hispanic migrants in Durham, North Carolina, USA. Soc Sci Med. 2010;70(7):1059–69.
Rhodes SD, Bischoff WE, Burnell JM, Whalley LE, Walkup MP, Vallejos QM, et al. HIV and sexually transmitted disease risk among male Hispanic/Latino migrant farmworkers in the Southeast: Findings from a pilot CBPR study. Am J Ind Med. 2010;53(10):976–83.
Montoya ID, Richard AJ, Bell DC, Atkinson JS. An analysis of unmet need for HIV services: The Houston Study. J Health Care Poor Underserved. 1997;8(4):446–60.
Sorensen W, Lopez L, Anderson P. Latino AIDS immigrants in the Western Gulf states: a different population and the need for innovative prevention strategies. J Health Soc Policy. 2001;13(1):1–19.
Sheppard VB, Zambrana RE, O’Malley AS, Zambrana RE, Cornelius LJ, Boykin SS, et al. Providing health care to low-income women: a matter of trust. Fam Pract. 2004;21(5):484–91.
Santos G, Puga AM, Medina C. HAART, adherence, and cultural issues in the US Latino community. AIDS Read. 2004;14(10 Suppl):S26–9.
Cuadros P. A home on the field: how one championship team inspires hope for the revival of small town America. New York, NY: Harpercollins; 2006.
Vissman AT, Bloom FR, Leichliter JS, Bachmann LH, Montaño J, Topmiller M, et al. Exploring the use of non-medical sources of prescription drugs among immigrant Latinos in the rural southeastern USA. J Rural Health. In press.
O’Donnell CR, O’Donnell L, San Doval A, Duran R, Labes K. Reductions in STD infections subsequent to an STD clinic visit. Using video-based patient education to supplement provider interactions. Sex Transm Dis. 1998;25(3):161–8.
Robles RR, Reyes JC, Colon HM, Sahai H, Marrero CA, Matos TD, et al. Effects of combined counseling and case management to reduce HIV risk behaviors among Hispanic drug injectors in Puerto Rico: a randomized controlled study. J Subst Abuse Treat. 2004;27(2):145–52.
North Carolina Department of Health and Human Services. Epidemiologic profile for HIV/STD prevention & care planning. Raleigh, NC: NC Department of Health and Human Services; 2009.
Israel BA, Eng E, Schulz AJ, Parker EA. Introduction to methods in community-based participatory research for health. In: Israel BA, Eng E, Schulz AJ, Parker EA, editors. Methods in community-based participatory research. San Francisco, CA: Jossey-Bass; 2005.
Rhodes SD, Malow RM, Jolly C. Community-based participatory research: a new and not-so-new approach to HIV/AIDS prevention, care, and treatment. AIDS Educ Prev. 2010;22(3):173–83.
Rhodes SD, DiClemente RJ, Yee LJ, Hergenrather KC. Factors associated with testing for hepatitis C in an internet-recruited sample of men who have sex with men. Sex Transm Dis. 2001;28(9):515–20.
Rhodes SD, Hergenrather KC, Vissman AT, Stowers J, Davis AB, Hannah A, et al. Boys must be men, and men must have sex with women: a qualitative CBPR study to explore sexual risk among African American, Latino, and white gay men and MSM. Am J Men’s Health. In press.
Rhodes SD, Hergenrather KC, Bloom FR, Leichliter JS, Montaño J. Outcomes from a community-based, participatory lay health advisor HIV/STD prevention intervention for recently arrived immigrant Latino men in rural North Carolina, USA. AIDS Ed Prev. 2009;21(Supplement 1):104–9.
Rhodes SD, Hergenrather KC. Recently arrived immigrant Latino men identify community approaches to promote HIV prevention. Am J Public Health. 2007;97(6):984–5.
Rhodes SD, Hergenrather KC, Montano J, Remnitz IM, Arceo R, Bloom FR, et al. Using community-based participatory research to develop an intervention to reduce HIV and STD infections among Latino men. AIDS Educ Prev. 2006;18(5):375–89.
Knipper E, Rhodes SD, Lindstrom K, Bloom FR, Leichliter JS, Montano J. Condom use among heterosexual immigrant latino men in the southeastern United States. AIDS Educ Prev. 2007;19(5):436–47.
Vissman AT, Eng E, Aronson RE, Bloom FR, Leichliter JS, Montaño J, et al. What do men who serve as lay health advisors really do?: Immigrant Latino men share their experiences as Navegantes to prevent HIV. AIDS Educ Prev. 2009;21(3):220–32.
Rhodes SD, Hergenrather KC, Aronson RE, Bloom FR, Felizzola J, Wolfson M, et al. Latino men who have sex with men and HIV in the rural south-eastern USA: findings from ethnographic in-depth interviews. Cult Health Sex. 2010;12(7):797–812.
Marsiglia FF, Kulis S. Diversity, oppression, and change. Chicago, IL: Lyceum; 2009.
Rhodes SD, Yee LJ, Hergenrather KC. A community-based rapid assessment of HIV behavioural risk disparities within a large sample of gay men in southeastern USA: a comparison of African American, Latino and white men. AIDS Care. 2006;18(8):1018–24.
Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 1987;9(2):183–205.
Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19(1):2–21.
Pleck JH, Sonenstein FL, Ku LC. Attitudes toward male roles among adolescent males: a discriminant validity analysis. Sex Roles. 1994;30(7/8):481–501.
Marin BV, Tschann JM, Gomez CA, Gregorich S. Self-efficacy to use condoms in unmarried Latino adults. Am J Community Psychol. 1998;26(1):53–71.
DiIorio C, Maibach E, O’Leary A, Sanderson CA, Celentano D. Measurement of condom use self-efficacy and outcome expectancies in a geographically diverse group of STD patients. AIDS Educ Prev. 1997;9(1):1–13.
Kalichman SC, Simbayi LC, Jooste S, Toefy Y, Cain D, Cherry C, et al. Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS Behav. 2005;9(2):135–43.
Rhodes SD, McCoy TP, Hergenrather KC, Vissman AT, Wolfson M, Alonzo J, et al. Prevalence estimates of health risk behaviors of immigrant Latino men who have sex with men. J Rural Health. In press.
Behling O, Law KS. Translating questionnaires and other research instruments: problems and solutions. London: Sage; 2000.
de la Puente M, Pan Y, Rose D. An overview of a proposed census bureau guideline for the translation of data collection instruments and supporting materials. Washington, DC: US Census Bureau; 2003.
Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs: Prentice-Hall; 1986.
Freire P. Education for critical consciousness. New York, NY: Seabury Press; 1973.
Rhodes SD. Tuberculosis, sexually transmitted diseases, HIV, and other infections among farmworkers in the eastern United States. In: Arcury TA, Quandt SA, editors. Latino farmworkers in the eastern united states: health, safety and justice. New York, NY: Springer; 2009. p. 131–52.
Eng E, Rhodes SD, Parker EA. Natural helper models to enhance a community’s health and competence. In: DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging theories in health promotion practice and research. San Francisco, CA: Jossey-Bass; 2009. p. 303–30.
Friedman LM, Furberg CD, DeMets DL. Fundamentals of clinical trials. 3rd ed. New York, NY: Springer-Verlag; 1998.
Muller KE, Fetterman BA. Regression and ANOVA: an integrated approach using SAS software. Cary, NC: SAS Institute & Wiley Inter-Science; 2003.
Little RJA, Rubin DB. Statistical analysis with missing data. 2nd ed. New York, NY: Wiley; 2002.
Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: Wiley; 1987.
van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med. 1999;18:681–94.
Royston P. Multiple imputation of missing values. The Stata J. 2004;4(3):227–41.
Vergidis PI, Falagas ME. Meta-analyses on behavioral interventions to reduce the risk of transmission of HIV. Infect Dis Clin North Am. 2009;23(2):309–14.
Herbst JH, Kay LS, Passin WF, Lyles CM, Crepaz N, Marin BV. A systematic review and meta-analysis of behavioral interventions to reduce HIV risk behaviors of Hispanics in the United States and Puerto Rico. AIDS Behav. 2007;11(1):25–47.
Janz NK, Zimmerman MA, Wren PA, Israel BA, Freudenberg N, Carter RJ. Evaluation of 37 AIDS prevention projects: successful approaches and barriers to program effectiveness. Health Educ Q. 1996;23(1):80–97.
Lyles CM, Crepaz N, Herbst JH, Kay LS. Evidence-based HIV behavioral prevention from the perspective of the CDC’s HIV/AIDS Prevention Research Synthesis Team. AIDS Educ Prev. 2006;18(4 Suppl A):21–31.
Lyles CM, Kay LS, Crepaz N, Herbst JH, Passin WF, Kim AS, et al. Best-evidence interventions: findings from a systematic review of HIV behavioral interventions for US populations at high risk, 2000–2004. Am J Public Health. 2007;97(1):133–43.
Darbes LA, Kennedy GE, Peersman GV, Zohrabyan L, Rutherford GW. Systematic review of HIV behavioral prevention research in Latinos. USA: Office of the Surgeon General, Department of Health and Human Services; 2001.
Johnson WD, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, et al. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database Syst Rev. 2008(3):CD001230.
Williams JK, Ramamurthi HC, Manago C, Harawa NT. Learning from successful interventions: A culturally congruent HIV risk-reduction intervention for African American men who have sex with men and women. Am J Public Health. 2009;99(6):1008–12.
Toro-Alfonso J, Varas-Diaz N, Andujar-Bello I. Evaluation of an HIV/AIDS prevention intervention targeting Latino gay men and men who have sex with men in Puerto Rico. AIDS Educ Prev. 2002;14(6):445–56.
Pequegnat W, Fishbein M, Celentano D, Ehrhardt A, Garnett G, Holtgrave D, et al. NIMH/APPC workgroup on behavioral and biological outcomes in HIV/STD prevention studies: a position statement. Sex Transm Dis. 2000;27(3):127–32.
Fishbein M, Pequegnat W. Evaluating AIDS prevention interventions using behavioral and biological outcome measures. Sex Transm Dis. 2000;27(2):101–10.
Acknowledgments
This study was funded by a grant from the National Institute of Mental Health (R21MH079827). We thank Jaime Montaño, the peer leaders, and the participants in this intervention trial.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rhodes, S.D., McCoy, T.P., Vissman, A.T. et al. A Randomized Controlled Trial of a Culturally Congruent Intervention to Increase Condom Use and HIV Testing Among Heterosexually Active Immigrant Latino Men. AIDS Behav 15, 1764–1775 (2011). https://doi.org/10.1007/s10461-011-9903-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-011-9903-4




