Abstract
Advanced ovarian carcinoma is a lethal tumour, and its standard treatment is consists of aggressive primary cytoreductive surgery followed by a chemoadjuvance based on platinum agents. We searched the Cochrane Gynaecological Cancer Group Trials Register of 2010, Cochrane Central Register of Controlled Trials, MEDLINE and EMBASE of 2010. We also searched registers of clinical trials, abstracts of scientific meetings, and reference lists of included studies. One of the goals of its management is to achieve the longest overall survival possible, and the most important survival factor is the residual tumour after cytoreductive surgery, obtaining the best surveillance in the cases where no tumour is left in the abdomen. To improve the cytoreductive rates in the actual management strategy, a change is necessary, selecting the cases not suitable for primary debulking surgery and adding, if necessary, procedures different than the ovarian tumour resection, like bowel resections, peritonectomies (particularly diaphragmatic ones) and splenectomies. This review pretends to understand why advanced ovarian carcinoma should be treated with primary surgery whenever possible and to rationate the use of extrapelvic surgical procedures. The improvement of surgical rates with these manoeuvres can determine the best management of our patients, without clinical complications.
Similar content being viewed by others
Background
Ovarian carcinoma is the second most common gynaecological cancer in developed countries, but the most mortal of them. The American Cancer Society estimated 21,550 new cases in the USA in 2009, and 14,600 women (more than half) will die of this disease [1]. These figures can be explained by the fact that most of these patients will be diagnosed with advanced disease, this is, stages III–IV. These data have not changed, and although standard treatment has improved the average overall survival from 1 year in the 1970s to nearly 5 years in the last decade [2], even in the best circumstances, only a third part of the patients will have a long-term cure rate. The best option for our patients is to improve the interval-free disease with an optimal management. Standard treatment consists in debulking surgery and adjuvant chemotherapy (ADJ). This ADJ is standard, and it is based in six cycles of a combination of platinum agents and paclitaxel, with a significant improvement when platinum agents are administrated intraperitoneally [3]. So, the factor we can modify is surgery. A debulking procedure may not be enough: the goal is to achieve a complete cytoreduction. In this review, we will study the rationality of advanced ovarian cancer surgery and the abdominal procedures the oncologist gynaecologist should be familiarized to improve the complete cytoreduction rates.
Surgery in advanced ovarian carcinoma
The optimal concept of cytoreduction in ovarian carcinoma surgery was stated with Griffith’s report in the 1970s, when he observed that overall survival was inversely proportional to residual mass under 1.6 cm [4]. From then on, many authors have discussed the optimal size of residual disease in advanced ovarian cancer to be limiting in surveillance [2, 5–9].
Historically, this threshold of optimal cytoreduction was defined in a 2-cm residual burden disease, and any smaller dimensions of residual disease were considered to have a favourable 5-year survival [10]. This definition was subsequently revised by the GOG, and in Protocol 97, which opened in 1986, the definition was set as ≤ 1-cm residual tumour [11]. But even when a clinical benefit was observed with this definition in several GOG trials (52, 158, and 172), it could be associated to a more favourable prognosis if the tumour left was <1 cm, or even more, if a complete absence of macroscopic disease was achieved [2, 3].
This relationship between surveillance and tumour left in the abdomen was demonstrated in a meta-analysis by Bristow et al. who reported a consistent 5.5% increase in median survival associated with each 10% increase in “maximal” cytoreduction among series with various fractions (median, 41.9%; range, 0–100%) undergoing “maximal” cytoreduction [8]. To establish the optimal threshold of residual disease is mandatory, as the transcendent end point is to get a potential survival benefit with the surgery approach, and do not harm unnecessarily with futility surgeries that will not give any benefit to the patient and potentially, can decrease her quality of life.
Why is primary surgery so determinant in ovarian carcinoma surveillance? Thigpen hypothesized the next reasons [12]:
-
1.
Surgery is able to remove resistant clones of tumour cells and thus decreases the likelihood of the early onset of drug resistance.
-
2.
The removal of large masses likely to be associated with poorly vascularized areas of tumour purportedly improved the probability of delivering adequate drug doses to the remaining cancer cells.
-
3.
The higher growth fraction in better vascularized small masses enhanced the effect of chemotherapy.
-
4.
In principle, smaller masses require fewer cycles of chemotherapy and thus decrease the likelihood of drug resistance.
-
5.
Removal of bulky disease theoretically enhanced the immune system.
-
6.
The patients feel better after removal of ascites and large tumour masses, particularly from the omentum.
-
7.
Surgery alleviates the associated nausea and satiety these patients feel.
By reviewing the literature, some authors question the real role of surgery in advanced epithelial ovarian carcinoma [13]. Up to date, primary cytoreductive surgery has not been shown to be beneficial in any randomized controlled trial. Several retrospective studies have shown that the quantity of tumour remaining is a major determinant of prognosis, but some authors assume that this may have more to do with tumour biology than the cytoreductive surgery per se. More on, the criteria by which surgical success is marked is inaccurate, with tumour residual underestimated more likely than overestimated. The concept of residual maximum largest diameter does not always reflect the residual disease, as one lesion of 1.5 cm is supposed to have better prognose than multiple widespread 0.5-cm miliar lesions. In addition, the morbidity of the procedures employed to achieve a complete surgery can be unacceptably high, delaying the initiation of chemotherapy and diminishing quality of life. So, for women in whom residual disease is inevitable, primary chemotherapy could be an alternative.
Although the concept of biological aggressiveness of the tumour is not well defined in the literature, it tries to explain those ovarian carcinomas whose natural history present in an abdominal cavity with a technical impossibility of achieving a complete cytoreduction. It is long-time discussed whether it is the surgical procedure itself that is responsible for the superior outcome associated with smaller disease or whether the ability to achieve an optimal debulking simply identifies a biologically more favourable patient group. This relationship between the extent of disease and the aggressive tumour biology has been long-time studied, and many variables have been tried to be correlated: the CA 125 levels, the ascites volume, the largest size of metastasis observed in a scanner, the disease affection of retroperitoneum or abdominal organs, etc., but no one has showed a practical consistent relationship [6, 7, 14–16].
More on, no clinical/laboratory/image technique has shown to be a determinant variable in survival, being always the absence of macroscopic residual disease the only variable related to the survival improve [9]. All the trials that have been initiated to answer this question were prematurely closed because of the bias favouring surgery [17, 18].
Optimal debulking rate
Studying the literature, a large account of different rates in optimal debulking, and therefore, in survival outcome can be observed. That suggests that it is necessary to have adequate systems to quantify the extent of abdominal disease and, somehow, standardize the surgical procedures, to achieve a complete cytoreductive surgery. Median and estimated 5-year survivals exceeding 75 months and 50% have been reproduced within multiple phase III trials and large primary surgical series for patients with optimal debulked stage III disease, with the prognosis uninfluenced by inclusion of patients with stage IIIA/B disease (Table 1) [2, 7, 9, 20, 22, 25].
While a randomized trial to confirm the effect of cytoreductive surgery on long-term survival is near impossible because of ethical and practical considerations, description of surgical procedures should be studied and used to increase the possibility of this optimal debulking [26].
One of the institutions which has more deeply studied the relationship between overall survival and advanced ovarian cancer surgery is the Memorial Sloan-Kettering Cancer Center. In their study, analysed various residual disease sizes, they could observe that patients with no-gross residual disease had the longest survival (106 months), but when the residual disease was less of 0.5 mm the survival went down to 66 months and to 48 months when the tumour left was 0.6–1 cm. The worst prognosis was observed when the tumour left was greater than 1 cm: the patient’s survival was 33 months [22]. Similar long-term survival has been reported by other authors when no-gross disease is left in the abdomen [3, 27].
One of the most determinant situations in this surgery in order to achieve an optimal cytoreduction is the presence of upper abdominal metastasis. The Memorial Center has recently reported in a series of 474 EOC stage IIIC that only 24% had no upper abdominal disease; meanwhile, a 42% rate of patients had metastasis of >1 cm involving the upper abdomen above the greater omentum. In particular, these metastases were present in the diaphragm, especially in the right hemi-diaphragm, and up to 40% of them with bulky metastatic diaphragmatic disease [28].
Chi, from this institution [22], has reported the surgical abdominal procedures needed to achieve its rate of optimal cytoreductive surgery. Up to 46 out of 465 patients had extension to the diaphragm peritoneum and needed a resection of it to achieve an optimal debulking. Large bowel resection was even more usual to be done (78/645). Less frequent were the next procedures: splenectomy (6/465), distal pancreatectomy (2/465), cholecystectomy (9/465), and liver resection (6/465). If we thoroughly study the extra procedures, different than the ones performed during staging (bilateral salpingo-ophorectomy, hysterectomy, omentectomy, appendicectomy, and pelvic/aortic lymphadenectomy), bowel resection, and diaphragm stripping/resection account the 74% of them. So, most of the surgery in case of affection of the upper abdomen is removing peritoneal tissue. With this attitude, the median survival time for the entire cohort (optimal and suboptimal result) was 48 months. Probably, these figures have gone up in this institution, as this retrospective study included patients from the period 1998–2003, and they only performed upper abdominal procedures since 2000. So, as they improved the surgical skills in new surgical procedures in upper abdomen, they moved to different figures. In a series of 141 cases with bulky upper abdominal disease (2001–2006) presented at SGO meeting in 2009 [29], this institution gets a 90% of optimal debulking (<1 cm) with a major complication rate of 29% and a 1.4% mortality. For obtaining 57 months overall survival, they reached an 86% rate of procedures in the diaphragm area and 32% splenectomies. It can be concluded that the more surgery is done, the better survival you get: near 10 months changing surgical strategy. Their experience suggests that incorporation of extensive upper abdominal debulking procedures may increase the optimal cytoreduction rate of primary surgery by 50%. As they have reported, this implantation of new procedures can dramatically change favourably the rates of an institution. And so, employing new approaches in the upper abdomen and extrapelvic anatomic spaces during the last decade, their optimal (<1 cm residual disease) and complete cytoreductive rates have improved in 26% and 17%, respectively, and more interesting, without increasing the complications rate [30].
Eisenkop et al. conclude the same idea finding that cytoreduction has more significant influence on survival that the extent of metastatic disease observed before surgery [21]. Incorporating extensive upper abdominal debulking procedures with standard pelvic cytoreduction (rectosigmoid resection, peritoneal stripping, diaphragm stripping, extensive bowel resection, splenectomy, partial gastrectomy, resection of liver and kidney) not only improved significantly the disease-free survival rate of patients left with optimal residual disease (85%), but also lead to a significant improvement in overall survival, with a median and estimated 5-year survival for this cohort of 54 months and 48%, respectively.
When studying deeply the multivisceral cytoreductive surgery procedures employed by different authors, it can be observed a different rate of bowel resection, splenectomy and peritonectomy needed to achieve an optimal debulking. This can indicate the different surgical criteria and, maybe, the “different concept” of complete cytoreduction. Scholz reports a median survival of 47 months and a 33% survival rate in a 5-year follow-up in a cohort of 101 patients affected of stage IIIC ovarian carcinoma with a high rate of extra procedures [31]. With a high rate of bowel procedures (81% modified posterior exenteration and 19% ileocoecal resection), 56% splenectomies, 39% Glisson’s capsule resection and 22% cholecystectomies, and >80% rate of complete debulking, this institution gets 3 months of difference of mean time to disease recurrence (29 vs 26 months) between patients without gross residual disease and patients with post-operative residual disease. Studying these results, 10% of the patients died within the first 6 months after surgery in the no-gross residual disease group, and although it is a one-center experience, that sets out if so much surgery is needed. Near a half of the cohort received neoadjuvant therapy, with a significant worse survival and time to progression in this group. This implies, somehow, that primary surgery should be the first patient’s option. We should consider that ovarian carcinoma is a celomic disease, with no near infiltration of solid viscera, and with superficial affection of the bowel serosa; so, the superficial resection should always be the first attempt whenever possible.
Two particular situations deserve some considerations: stage IV ovarian carcinoma and the primary peritoneal carcinoma. Stage IV disease presents an obstacle toward maximal surgical cytoreduction in primary ovarian cancer. Early reports suggested that even with stage IV disease, optimal cytoreduction may be associated with improved outcome [32]. However, many of these reports defined “optimal” cytoreduction as residual disease of less than 2 cm. Furthermore, these early reports identified pleural cavity disease by positive cytology alone. The optimal method to evaluate disease in the pleural cavity is with video-assisted thoracic surgery (VATS). Recent reports suggest the utilization of VATS to guide management of primary ovarian cancer [33]. Findings with VATS can quantify intrathoracic disease and allow intrathoracic cytoreduction achieving maximal cytoreduction.
Near 10% of supposed advanced ovarian carcinomatosis are really peritoneum papillary serous carcinomas [34]. Most of the patients (about 98%) present stages III or IV [35] and that explains its worse prognosis, with a median survival of near 2 years (21–26 months). Although the cornerstone of treatment is surgery, the suboptimal debulking rate is higher than in ovarian carcinoma, as it usually presents with extensive nodular infiltration of the mesenteric, visceral and peritoneal surfaces, and involvement of the porta hepatis, liver, stomach, and retroperitoneal nodes [36].
It would be a simple statement that optimal surgery by itself is the most important surveillance prognosis factor. Surgery and chemotherapy are hand with hand along the time life of the disease. So, when we are pointing that optimal debulking to no disease in the abdomen is the most important prognosis factor, we suggest that chemotherapy is in its best moment to adjuvant the therapy. And this can be observed in the significant improvement in long-term survival with the maximum benefit of intraperitoneal chemotherapy schedules when an optimal surgery has been achieved [3].
Interestingly, one of the “historically” criticisms to primary surgery has been that aggressive surgery often dilates in time the starting of the chemotherapy treatment. The common and intuitive belief that chemotherapy should start as soon as possible after surgery, and especially after suboptimal surgery, has never been demonstrated in the literature. On the contrary, the few published studies [37, 38] in the literature indicate that the time interval has little or no importance, and it may even be disadvantageous to start the chemotherapy too early after surgery.
In light of the above considerations, the cornerstone of management for patients with a diagnosis of ovarian cancer is surgical intervention. Surgery plays an essential role in any stage because establishes a diagnosis and determine the extent of disease and, of course, tries to achieve a complete debulking of abdominal metastasis. This surgery should be done by an experienced gynaecologist oncologist team as it has been shown to improve the patients’ outcome and result in a more favourable cost-effective analysis [39]. Probably this is one of the more real prognosis factors in these patients, and there should not be any excuse to refer an advanced ovarian cancer patient to an expertise surgical team. Recently, a study of the National Cancer Data Base established in ≥ 21 cases/year the ovarian cancer surgical volume in hospital to be associated with a higher likelihood of patients with advanced disease to be treated correctly with standard treatment, being a prognostic factor for overall survival. But in this study, only 61% of all the patients studied had a recommended treatment (surgery plus adjuvant treatment), identifying the above mentioned problem: how many patients are not correctly managed by non expertise specialist [40].
Strategies to improve surgical management
The first intention when attempting a cytoreductive surgery should be to achieve a complete debulking surgery. Different procedures than the staging ones should be considered. Upper abdominal surgery procedures and bowel surgery, the most employed, should be included in the knowledge of the gynaecological oncologist surgeon. But prior to surgery, correct selection and diagnosis of the real extension of disease should be properly done, being the laparoscopic exploration probably the best tool. It is important to describe the most important considerations of these procedures to know the real impact on the disease and to be aware of the potential complications.
Laparoscopic exploration
Laparotomy constitutes the most accurate way to evaluate tumour burden and establish whether or not a patient is suitable of optimal surgery, but it is an aggressive approach if used only to explore the abdomen and to consider tumor resectability. In the last decade, some institutions have matched the laparoscopic exploration in order to assess resectability in advanced disease [24, 41–43]. Advantages of laparoscopy include magnification of pelvic and abdominal anatomy and enhanced visualization of the peritoneum surface of the upper abdomen, particularly diaphragm. It also allows exploring de “traditional” places of surgical contraindications: hepatic hilio, bowel serosa, and small bowel mesenterium. Its short operative time permit an out day patient surgery and a correct strategy of a future surgery or, otherwise, a neoadjuvant surgery. With this more comprehensive approach, we avoid a hypothetic incomplete debulking during an initial laparotomy, improving the proportion of patients achieving an optimal residual disease. And so, with the use of a diagnostic open laparoscopy, Anglioli et al. have reported a 96% rate of complete cytoreduction [42].
A disadvantage with the use of open laparoscopy is the magnification of the disease, increasing the number of patients treated with neoADJ. The laparoscopic exploration can lead the surgeon to believe there is more extensive disease than there really is, creating doubts on a successful cytoreduction. When studying deeply Anglioli’s results, about 10–15% of patients submitted to neoADJ after open laparoscopy could probably be optimally cytoreducted.
Bowel resection
Near 25% of women with advanced ovarian carcinoma needs a bowel resection as part of their primary cytoreductive operation [44–46].
The data regarding colon resection for the purpose of surgical cytoreduction of ovarian cancer and the potential benefit that can be achieved are all retrospective, but all the information published supports a benefit in terms of survival when cytoreduction is clearly optimal, confirming the benefit of complete debulking of the disease.
The most frequent bowel segment involved in surgery is the rectum-sigmoid. Bulky disease involving the cul-de-sac can require an en-bloc resection with low-anterior resection in order to achieve a complete gross resection of the pelvic disease [45, 47–49]. Most women undergo a primary colorectal anastomosis without a protective colostomy. The most important complication is the fail of a low-anterior rectal anastomosis, but usually it is presented with a low rate, less than 5% [44, 48, 50].
The second most frequent bowel resection in cytoreductive surgery is the terminal ileum and the ceccum, because their proximity to the pelvis and usual affection of the appendix [51]. Other important part of the bowel than can be considered to be removed is the transverse colon, because the high incidence of bulky omental metastasis than can infiltrate the bowel wall/mesentery. So many times this resection can be avoided because superficial affection, with an easy finding of a surgical plane for dissection between the fatty tissue and the colon serosa. When this situation is not possible, omentectomy en bloc with transverse colectomy has to be considered.
Whenever possible, it is important to avoid large bowel resections and multiple anastomoses. And also, it has a great impact on quality of life to avoid estomas, as they have not shown to protect a leaking in the anastomosis [46, 52].
The impact on quality of life of large bowel resections is not as important as it can be thought, with a median frequency of two bowel movements per day 6 months after surgery, although the patients should be aware of dehydrations problems, mostly the first weeks after surgery and during chemotherapy treatment [50]. Antimotility medications have to be considered, and also resincolestiramine agents whenever the ileocecum valve is removed.
Diaphragm surgery
The Morrison pouch is, because of gravity, one of the most frequent places of disease affection in advanced ovarian cancer, and, negatively, one of the most usual related places of residual disease in cases of cytoreductive surgery [53]. Diaphragmatic disease can be optimally debulked with several procedures described in the literature, as ablation techniques, peritonectomy and diaphragm resection [54, 55]. The procedures in this part of the upper abdomen should be included in the surgical oncology training programs, as they are determinant in achieving an optimal cytoreduction. As in other procedures, it is necessary a deep knowledge of the liver and diaphragmatic anatomy, basically to avoid any injury of major vessels (retro-hepatic cava vein, hepatic hilio, supra-hepatic veins, and diaphragmatic vessels). Technically, it is determinant to do a complete liver mobilization at the beginning of the surgical procedure in order to avoid difficulties in the diaphragm suturing in case that a closure of a defect is needed. Even if part of the muscle is removed, there are not usually problems in making a closure without tension. Although rarely needed, a permanent mesh can be used.
The most important complication is pleural effusion, presented in near a half of the patients, and correlates with liver mobilization, size of diaphragmatic resection and the diaphragmatic perforation that can be present in near 50% of the cases [56]. Intra- and post-operative management of this complication varies between authors, but the low rate of thoracocentesis or pleural drainage really needed does not support the routinely use of prophylactic chest tube placement, saving it for patients with a complete liver mobilization and large diaphragmatic peritoneal/muscle resection, situation that can be presented in 7–30% of the cases [56–60]. It is important to teach the patient pre-operatively breathing exercises and to have a strict early post-operative pulmonary follow-up. Less frequent complications are pulmonary embolism, hemothorax and pneumothorax.
Ablation systems can be employed to facilitate a complete cytoreduction of the diaphragm peritoneum. And so, the argon beam coagulation can achieve homogeneous and consistent tissue destruction [61]. Using a combination of the argon beam coagulation and the cavitron ultrasonic surgical aspirator with radical surgical techniques, Eisenkop et al. [7] reported removal of all visible tumour in 85.3% of 163 consecutive patients with advanced ovarian cancer presented for primary cytoreductive surgery. This study demonstrated that complete surgical elimination of all macroscopic disease was feasible and associated with prolonged survival.
Splenectomy
To perform optimal cytoreductive surgery in patients with advanced ovarian cancer, it is often necessary to perform a splenectomy, many times because of the extension of the omentum invasion. The surgical technique is well described in the literature [62, 63]. When splenic lesions are macroscopically suspected during cytoreductive surgery for an ovarian cancer, up to 80% of the cases the disease is confirmed by histology, justifying the splenectomy [64].
Up to 13% of the splenectomy indications can be due to intra-operative trauma, frequently observed during omentum debulking, omentum manoeuvres and large bowel dissection [65].
After a splenectomy, a number of considerations should be taken into account. Changes typically occur in the blood composition, and frequently leukocytosis, trombocytosis and Howell–Jolly bodies in blood analysis can be observed temporally. More serious are pulmonary complications, (lower lobe atelectasis that can derivate to pneumonia and pleural effusions) and subphrenic abscess, many times aggravated with a pancreatic leakage, that can be diagnosed because a pseudocyst [66].
Because the immunological impact promotes a decrease of serum immunoglobulin M, the administration of pneumococcus vaccine, meningococcus vaccine, and a vaccine against haemophilus influenzae are mandatory. And because of the increase rate of sepsis, antibiotic prophylaxis is recommended [62].
Lymph nodes debulking
Retroperitoneal lymph node dissection is well described in the literature [67]. Whether systematic removal of retroperitoneal lymph nodes should be part of maximal cytoreductive surgery or not is still unclear. Retroperitoneal lymph node involvement occurs in approximately 50–80% of women with advanced ovarian cancer, but not always in a bulky fashion [68]. An association between lymph node involvement and clinical outcome has been long established, with a worse prognosis when they are involved. In a randomized trial considering systematic pelvic and aortic lymphadenectomy versus only selected bulky nodes dissection, it could be observed a 25% improvement in progression-free survival in the systematic lymphadenectomy arm, although this did not translate into an improvement in overall survival [69].
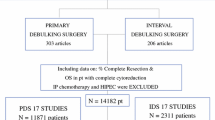
Neoadjuvant chemotherapy in advanced ovarian carcinoma
NeoADJ is an “attractive” strategy for patients considered to be suboptimal debulked. Table 2 shows different overall survivals published in the literature when a neoADJ approach is employed. Reasons for suboptimal debulking in ovarian carcinoma surgery may be due to several causes. Probably, surgery related ones are important: surgeon skills, the surgeon “believing” in cytoreductive surgery, the institution and its facilities. But more important are the disease dependent factors, like abdominal and retroperitoneal extension, with affection of the upper abdomen, the small bowel mesenterium, the hepatic hileo, etc., and the comorbidity of the patient (age, other medical disease, and medical status). Indicate a neoadjuvant therapy should be done with caution, cause taking directly this option is potentially worsening the patient vital prognosis. Disease factors associated with suboptimal debulking have a big amount of false positives, and they should not be taken into account only when making up the clinical decision. As it has been discussed above, many reports in the literature have showed the limitations of this clinical criteria (CA 125, computed tomography), with a false-positive rate as high as 62–86% predicting an optimal cytoreduction [75, 76].
The “optimal” rate of patients that should be managed with neoADJ may be “patients whom a primary surgery would result in an incomplete cytoreduction”. Identify these patients is difficult, as it depends on so many factors above related. Probably, the rate should keep in a wide range around 20%, as the best figures of optimal cytoreductive surgery are actually around 80%. The problem probably is not the rate of neoadjuvant therapy but the proper identification of patients not suitable for surgery. Nowadays, we have to play with all the tools we can offer the patient in our institutions: the clinical data, including CA 125, the radiographic findings and the laparoscopic exploration.
Recently it has been published an EORTC-GCG/NCIC-CTG randomized trial lead by Vergote [24], comparing primary debulking surgery with neoADJ. They demonstrated similar PFS and overall survival when compared with patients undergoing primary cytoreductive surgery. The median overall survival was 29 months in the primary surgery group and 30 months in the neoADJ group, with a median progression-free survival in both groups of 12 months. It has to be stand out the low optimal debulking rate in the primary debulking surgery arm they published (41.6%), being the most frequent sites of residual disease the diaphragm, the abdominal peritoneum and pelvis (pouch of Douglas, uterus, bladder, rectum, and sigma), anatomical places that have been long discussed above that are technically and safely removable. Again, the strongest independent predictor of prolonged survival was the absence of residual tumour after surgery, situation that confronts with their low optimal debulking rate. The median overall survival for women with no residual tumour (optimal result), those with residual tumours that measured 1–10 mm in diameter (suboptimal result), and those with residual tumours larger than 10 mm (other result) was 45, 32, and 26 months, respectively, in the group that underwent primary debulking surgery and 38, 27, and 25 months, respectively, in the group that underwent neoADJ. Additionally, they did not observe significant advantages between these approaches in adverse effects, quality of life or post-operative morbidity or mortality.
One fact when performing surgery after neoADJ is that gross disease is sometimes difficult to identify, with the original tumour extension frequently not visible. We can hypothesize that the microscopic tumour burden left is bigger, with more possible tumour resistance clones and so, more facilities for tumour recurrence. Also, after chemotherapy and after a failed attempt of primary surgery, the abdominal procedures (peritoneal stripping and cytoreductive procedures) are more difficult, as tissue characteristics change to fibrosis and neovascularization [31].
Impact on quality of life and morbimortality
Quality of life of patients with advanced ovarian carcinoma should be, with the cure rate and progression-free survival, end points of treatment. Which negative impacts have standard treatment in quality of life patients? We have to consider separately surgery and chemotherapy impact. Surgical menopause, infertility, sexual dysfunction and bowel obstruction are the most frequent observed because of surgery [77]. Population-based reports on post-operative mortality after primary cytoreductive surgery for advanced stage EOC vary with rates from 2.5% to 4.8%, with a mean of 3.7% [78]. This low-operative risk corroborates the current treatment strategy of primary cytoreductive surgery followed by platinum-based chemotherapy in patients with advanced stage EOC. But this figures move to 5.4% till 11.7% in patients older than 80 years, and we should consider to change the management to a neoADJ schedule in this group of patients [79].
But optimal debulking with a more aggressive surgery not necessarily implies more comorbidity or mortality. And so, Soegaard [80] and Marx [81] have reported similar post-operative mortality (4.8% and 4.4%, respectively) with very different surgical outcomes (79% vs 39% optimal cytoreduction rates, respectively).
Conclusions
Actual surgical management goal of advanced ovarian cancer is to achieve a complete cytoreduction of the tumour. This is constantly reported in the literature as the most important factor in patient’s surveillance. It is our responsibility to employ different procedures than the tumoral ovarian and uterus removal, mainly outside the pelvis. These new procedures should be trained in any institution specialized in the surgical management of this tumour.
References
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ (2008) Cancer statistics 2009. CA Cancer J Clin 59:225–249
Ozols RF, Bundy BN, Greer BE et al (2003) Phase III trial of carboplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecological Oncology Group study. J Clin Oncol 21(17):3194–3200
Armstrong DK, Bundy B, Wenzel L, Huang HQ, Baergen R, Lele S et al (2006) Intraperitoneal cisplatin and paclitaxel ovarian cancer. N Engl J Med 354:34–43
Griffiths CT (1978) Surgical resection of tumor bulk in the primary treatment of ovarian cancer. Natl Cancer Inst Monogr 42:131–136
Hoskins WJ, McGuire WP, Brandy MF, Homsley HD, Creasman WT, Berman M et al (1994) The effect of diameter oflartgest residual disease on survival after primary cytoreductive surgery in patients with suboptimal residual epithelial ovarian carcinoma. Am J Obstet Gynecol 170(4):974–979
Makar AP, Baekelandt M, Trope' CG, Kristensen GB (1995) The Prognostic significance of residual disease, FIGO substage, tumor histology, and grade in patients with FIGO stage III ovarian cancer. Gynecol Oncol 56:175–180
Eisenkop SM, Friedman RL, Wang H (1998) Complete cytoreductive surgery is feasible and maximizes survival in patients with advanced epithelial ovarian cancer: a prospective study. Gynecol Oncol 69:103–106
Bristow RE, Tomacruz RS, Armstrong DK, Trimble ELS, Montz FJ (2002) Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J Clin Oncol 20:1248–1259
Aletti G, Dowdy SC, Gostout BS, Jones MB, Stanhope RC, Wilson TO et al (2006) Aggressive surgical effort and improved survival in advanced-stage ovarian cancer. Obstet Gynecol 107:77–85
Hacker NF, Berek JS, Lagasse LD, Nieberg RK, Elashoff RM (1983) Primary cytoreductive surgery for ovarian cancer. Obstet Gynecol 61:413–420
Omura GA, Blessing J, Ehrlich C et al (1991) Long follow-up and prognostic factor analysis in advanced ovarian carcinoma: the gynecologic oncology group experience. J Clin Oncol 9:1138–1150
Thigpen T (2004) The if and when of surgical debulking for ovarian carcinoma. N Engl J Med 351(24):2544–2546
Carter J (2004) Primary surgery for ovarian cancer. In: Gershenson DM, McGuire WP, Gore M, Quinn MA, Thomas G (eds) Gynecologic cancer: controversies in management. Elsevier, pp 399–409
Gemer O, Lurian M, Gdalevich M, Kapustian V, Piura E, Schneider D et al (2005) A multicenter study of CA-125 level as a predictor of non-optimal cytoreduction of advanced epithelial ovarian cancer. Eur J Surg Oncol 31:1006–1010
von Georgi R, Franke FE, Munstedt K (2003) Influence of surgery and postoperative therapy and tumor characteristics on patient prognosis in advanced ovarian carcinomas. Eur J Obstet Gynecol Reprod Biol 111:189–196
Naik R, Nordin A, Cross PA, Hemming D, Lopes AB, Monaghan JM (2000) Complete cytoreduction: is epithelial ovarian cancer confined to the pelvis biologically different from bulky abdominal disease? Gynecol Oncol 78:176–180
Covens AL (2000) A critique of surgical cytoreduction in advanced ovarian cancer. Gynecol Oncol 78(3):269–274
Markman M (2007) Conceptr of optimal cytoreduction in advanced ovarian cancer: a brief critique and a call for action. J Clin Oncol 25(27):4168–4170
Alberts DS, Liu PY, Hannigan EV, O'Tolle R, Williams SD, Young JA et al (1996) Intraperitoneal cisplatin plus intravenous cyclophosphamide versus intravenous cisplatin plus intravenous cyclophosphamide for stage III ovarian cancer. N Engl J Med 335:1950–1955
Le T, Krepart GV, Lotocki RJ, Heywood MS (1997) Does debulking surgery improve survival in biologically aggressive ovarian cancer. Gynecol Oncol 67:208–214
Chi DS, Eisenhauer EL, Lang J, Huh J, Haddad L, Abu-Rustum NR, Sonoda Y, Levine DA, Hensley M, Barakat RR (2006) What is the optimal goal of primary cytoreductive surgery for bulky stage IIIC epithelial ovarian carcinoma (EOC)? Gynecol Oncol 103:559–564
Eisenkop S, Spirtos NM, Lin WM (2006) “Optimal” cytoreduction for advanced epithelial ovarian cancer: a commentary. Gynecol Oncol 103:329–335
Benedetti Panici P, Maggioni A, Hacker N, Landoni F, Ackermann S, Campagnutta E et al (2005) Systematic aortic and pelvic lymphadenectomy versus resection of bulky nodes only in optimally debulked advanced ovarian cancer: a randomized clinical trial. J Natl Cancer Inst 97:560–566
Zivanovic O, Eisenhauer EL, Zhou Q, Iasonos A, Sabbatini P, Sonoda Y et al (2008) The impact of bulky upper abdominal disease cephalad to the greater omentum on surgical outcome for stage IIIC epithelial ovarian, fallopian tube, and primary peritoneal cancer. Gynecol Oncol 108:287–292
Zivanovic O et al (2009) Upper abdominal disease chephalad to the greater omentum and the impact on progression-free survival in patients with stage IIIC ovarian cancer. SGO 112(Suppl) abstract 1
Chi DS, Franlkin CC, Levine D, Akselrod F, Sabbatini P, Jarnigan WR et al (2004) Improved optimal cytoreduction rates for stages IIIC and IV epithelial ovarian, fallopian tube, and primary peritoneal cancer: a change in surgical approach. Gynecol Oncol 94:650–654
Eisenkop SM, Spirtos NM, Friedman RL, Lin WC, Pisani AL, Perticucci S (2003) Relative influences of tumor volume before surgery and the cytoreductive outcome on survival for patients with advanced ovarian cancer: a prospective study. Gynecol Oncol 90:390–394
Scholz HS, Tasdemir H, Hunlich T, Turnwald W, Both A, Egger H (2007) Multivisceral cytoreductive surgery in FIGO stages IIIC and IV epithelialovarian cancer: results and 5-year follow-up. Gynecol Oncol 106:591–595
Curtin JP, Malik R, Venkatraman ES, Barakat RR, Hoskins WJ (1997) Stage IV ovarian cancer: impact of surgical debulking. Gynecol Oncol 64:9–12
Diaz JP, Abu-Rustum NR, Sonoda Y, Downey RJ, Park BJ, Flores RM et al (2010) Video-assisted thoracic surgery (VATS) evaluation of pleural effusions in patients with newly diagnosed advanced ovarian carcinoma can influence the primary management choice for these patients. Gynecol Oncol 116:483–488
Fromme GL, Gershenson DM, Silva E (1990) Papillary serous carcinoma of the peritoneum. Obstet Gynecol 75:89–95
Ben-Baruch G, Sivan E, Moran O, Rizel S, Menczer J, Seidman D (1996) Primary peritoneal serous papillary carcinoma: a study of 25 cases and comparison with Stage III–IV ovarian papillary serous carcinoma. Gynecol Oncol 60:393–396
Killackey MA, Davis AR (1993) Papillary serous carcinoma of the peritoneal surface: matched-comparison with papillary serous ovarian carcinoma. Gynecol Oncol 51:171–174
Flynn PM, Paul J, Cruickshank DJ (2002) Does the interval from primary surgery to chemotherapy influence progression-free survival in ovarian cancer? Gynecol Oncol 86:354–357
Sorbe B (2004) Prognostic importance of the time interval from surgery to chemotherapy in treatment of ovarian carcinoma. Int J Gynecol Cancer 14:788–793
Bristow RE, SAntillan A, Diaz-Montes TP et al (2007) Centralization of care for patients with advanced-stage ovarian cancer: a cost-effectiveness analysis. Cancer 109(8):1513–1522
Bristow R, Palis BE, Chi DS, Cliby WA (2010) The National Cancer Database report on advanced-stage epithelial ovarian cancer: impact of hospital surgical case volume on overall survival and surgical treatment paradigm. Gynecol Oncol 118(3):262–267
Vergote I, Tropé CG, Amant F et al (2010) NeoADJ or primary surgery in stage IIIC or IV ovarian cancer. NEJM 363:943–953
Fagotti A, Fanfani F, Ludovisi M, Lo Voi R, Bifulco G, Testa A et al (2005) Role of laparoscopy to assess the chance of optimal cytoreductive surgery in advanced ovarian cancer: a pilot study. Gynecol Oncol 96:729–735
Angioli R, Palaia I, Zullo MA, Muzii L, Manci N, Calcagno M, Panici PB (2006) Diagnostic Panici open laparoscopy in the anagement of advanced ovarian cancer. Gynecol Oncol 100(3):455–461
Fagotti A, Fanfani F, Vizzielli G, Gallotta V, Ercoli A, Paglia A, Costantini B, Vigliotta M, Scambia G, Ferrandina G (2010) Should laparoscopy be included in the work-up of advanced ovarian cancer patients attempting interval debulking surgery? Gynecol Oncol 116:72–77
Scarabelli C, Gallo A, Franceschi S, Campagnutta E, De Piero G, Giorda G (2000) Primary cytoreductive surgery with rectosigmoid colon resection for patients with advanced epithelial ovarian carcinoma. Cancer 88:389–397
Aletti GD, Podratz KC, Jones MB, Cliby WA (2006) Role of rectosigmoidectomy and stripping of pelvic peritoneum in outcomes of patients with advanced ovarian cancer. J Am Coll Surg 203:521–526
Hoffman MS, Griffin D, Tebes S, Cardosi RJ, Martino MA, Fiorica JV et al (2005) Sites of bowel resected to achieve optimal ovarian cancer cytoreduction: implications regarding surgical management. Am J Obstet Gynecol 193:582–586
Gillette-Cloven N, Burger RA, Monk BJ, McMeekin DS, Vasilev S, DiSaia PJ et al (2001) Bowel resection at the time of primary cytoreduction for epithelial ovarian cancer. J Am Coll Surg 193:626–632
Mourton SM, Temple LK, Abu-Rustum NR, Gemignani ML, Sonoda Y, Bochner BH et al (2005) Morbidity of rectosigmoid resection and primary anastomosis in patients undergoing primary cytoreductive surgery for advanced epithelial ovarian cancer. Gynecol Oncol 99:608–614
Estes JM, Leath CA 3rd, Straughn JM Jr, Rocconi RP, Kirby TO, Huh WK et al (2006) Bowel resection at the time of primary debulking for epithelial ovarian carcinoma: outcomes in patients treated with platinum and taxane-based chemotherapy. J Am Coll Surg 203:527–532
Silver DF, Zgheib NB (2009) Extended left colon resections as part of complete cytoreduction for ovarian cancer: tips and considerations. Gynecol Oncol 114:427–430
Hoffman MS, Zervose E (2008) Colon resection for ovarian cancer: intraoperative decisions. Gynecol Oncol 111:S56–S65
Konishi T, Watanabe T, Kishimoto J, Nagawa H (2006) Risk factors of anastomotic leakage after surgery for colorectal cancer: results of prospective surveillance. J Am Coll Surg 202:439–444
Tangjitgamol S, Manusirivithaya S, Laopaiboon M, Lumbiganon P (2009) Interval debulking surgery for advanced epithelial ovarian cancer: a Cochrane systematic review. Gynecol Oncol 112:257–264
Cliby W, Dowdy S, Feitoza SS, Gostout BS, Podratz KC (2004) Diaphragm resection for ovarian cancer: technique and short-term complications. Gynecol Oncol 94:655–660
Kehoe SM, Eisenhauer EL, Chi DS (2008) Upper abdominal surgical procedures: liver mobilization and diaphragm peritonectomy/resection, splenectomy, and distal pancreatectomy. Gynecol Oncol 111:S51–S55
Fanfani F, Fagotti A, Gallotta V, Ercoli A, Pacelli F, Costantini B, Vizzielli G, Margariti PA, Garganese G, Scambia G (2010) Upper abdominal surgery in advanced and recurrent ovarian cancer: role of diaphragmatic surgery. Gynecol Oncol 116:497–501
Dowdy SC, Loewen RT, Aletti G et al (2008) Assessment of outcomes and morbidity following diaphragmatic peritonectomy for women with ovarian carcinoma. Gynecol Oncol 109:303–307
Devolder K, Amant F, Neven P et al (2008) Role of diaphragmatic surgery in 69 patients with ovarian carcinoma. Int J Gynecol Cancer 18:363–368
Gouy S, Chereau E, Custodio AS, Uzan C, Pautier P, Haie-Meder C, Duvillard P, Morice P (2010) Surgical procedures and morbidities of diaphragmatic surgery in patients undergoing initial or interval debulking surgery for advanced-stage ovarian cancer. J Am Coll Surg 210(4):509–514
Einenkel J, Ott R, Handzel R et al (2009) Characteristics and management of diaphragm involvement in patients with primary advanced-stage ovarian, fallopian tube, or peritoneal cancer. Int J Gynecol Cancer 19:1288–1297
Bristow RE, Smith Sehdev AE, Kaufman HS et al (2001) Ablation of metastatic ovarian carcinoma with the argon beam coagulator: pathologic analysis of tumor destruction. Gynecol Oncol 83(1):49–55
Poulin EC, Schlachta CM, Mamazza J (2005) Splenectomy. Gastrointestinal tract and abdomen. In: Souba WW, Fink MJ, Jurkovich GJ et al (eds) ACS surgery. WebMd, New York
Ramirez PT, Dos Reis R (2007) Splenectomy in patients with advanced or recurrent ovarian cancer: open and laparoscopic surgical techniques and clinical outcomes. Gynecol Oncol 104:S29–S32
Uzan C, Bontoux LM, Gouy S, Duvillard P, Pautier P, Lhommé C, Morice P (2010) Correlation between macroscopic and microscopic diseases on splenectomies performed in the surgical management of ovarian cancer. Int J Gynecol Cancer 20(6):965–970
Magtibay PM, Adams PB, Silverman MB, Cha SS, Podratz KC (2006) Splenectomy as part of cytoreductive surgery in ovarian cancer. Gynecol Oncol 102:369–374
Eisenkop SM, Spirtos NM, Lin WM (2006) Splenectomy in the context of primary cytoreductive operations for advanced epithelial ovarian cancer. Gynecol Oncol 100:344–348
Chi DS, Roberts CA, Abu-Rustum NR (2007) Retroperitoneal lymph node dissection. Gynecol Oncol 104:S37–S39
Burghardt E, Girardi F, Lahousen M, Tamussino K, Stettner H (1991) Patterns of pelvic and paraaortic lymph node involvement in ovarian cancer. Gynecol Oncol 40:103–106
Panici PB, Maggioni A, Hacker N et al (2005) Systematic aortic and pelvic lymphadenectomy versus resection of bulky nodes only in optimally debulked advanced ovarian cancer: a randomized clinical trial. J Natl Cancer Inst 8:560–566
Salani R, Axtell A, Gerardi M, Holschneider C, Bristow RE (2008) Limited utility of conventional criteria for predicting unresectable disease in patients with advanced stage epithelial ovarian cancer. Gynecol Oncol 108:271–275
Axtell AE, Lee MH, Bristow RE et al (2007) Multi-institutional reciprocal validation study of computed tomography predictors of suboptimal primary cytoreduction in patients with advanced ovarian cancer. J Clin Oncol 25(4):384–389
Sun CC, Ramirez P, Bodurka DC (2007) Quality of life for patients with epithelial ovarian cancer. Nat Clin Pract Oncol 4(1):18–29
Gerestein CG, Damhuis RAM, Burger CW, Kooi GS (2009) Postoperative mortality after primary cytoreductive surgery for advanced stage epithelial ovarian cancer: a systematic review. Gynecol Oncol 114:523–527
Alphs HH, Zahurak ML, Bristow RE, Diaz-Montes TP (2006) Predictors of surgical outcome and survival among elderly women diagnosed with ovarian and primary peritoneal cancer. Gynecol Oncol 103(3):1048–1053
Soegaard Andersen E, Knudsen A, Svarrer T, Lund B, Nielsen K, Grove A et al (2005) The results of treatment of epithelial ovarian cancer after centralisation of primary surgery. Results from North Jutland, Denmark. Gynecol Oncol 99(3):552–556
Marx C, Bendixen A, Hogdall C, Ottosen C, Kehlet H, Ottesen B (2007) Organisation and quality of primary surgical intervention for ovarian cancer in Denmark. Acta Obstet Gynecol Scand 86(12):1496–1502
Eisenkop SM, Spirtos NM, Montag TW, Nalick RH, Wang H (1992) The impact of subspecialty training on the management of advanced ovarian cancer. Gynecol Oncol 47:203–209
du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J (2009) Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzinom (AGO-OVAR) and the Groupe d'Investigateurs Nationaux Pour les Etudes des Cancers de l'Ovaire (GINECO). Cancer 115:1234–1244
Vergote I, DeWever I, Tjalma W, Van Gramberen M, Decloedt J, van Dam P (1998) Neoadjuvant chemotherapy or primary debulking surgery in advanced ovarian carcinoma: a retrospective analysis of 285 patients. Gynecol Oncol 71:431–436
Schwartz PE, Rutherford TJ, Chambers JT, Kohorn EI, Thiel PR (1999) Neoadjuvant chemotherapy for advanced ovarian cancer: long-term survival. Gynecol Oncol 72:93–99
Ushijima K, Ota S, Komai K, Matsuo G, Motoshima S, Honda S et al (2002) Clinical assessment of neoadjuvant chemotherapy and interval cytoreductive surgery for unresectable advanced ovarian cancer. Int Surg 87:185–190
Fanfani F, Ferrandina G, Corrado G, Fagotti A, Zakut HV, Mancuso S et al (2003) Impact of interval debulking surgery on clinical outcome in primary unresectable FIGO Stage IIIc ovarian cancer patients. Oncology 65:316–322
Le T, Faught W, Hopkins L, Fung MFK (2005) Primary chemotherapy and adjuvant tumor debulking in the management of advanced-stage epithelial ovarian cancer. Int J Gynecol Cancer 15:770–775
Conflicts of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Domingo, S., Gurrea, M. & Pellicer, A. How to improve the optimal cytoreductive surgery in advanced ovarian carcinoma. Gynecol Surg 8, 289–298 (2011). https://doi.org/10.1007/s10397-011-0659-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10397-011-0659-7