Abstract
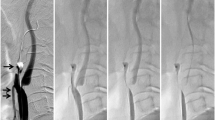
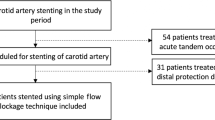
The treatment for patients with near occlusion of the cervical internal carotid artery (ICA) is controversial. The aim of this study was to examine the results of carotid artery stenting (CAS) as a surgical treatment for ICA near occlusion. Between April 2008 and September 2012, 14 patients (all men; mean age, 75.4 years) with ICA near occlusion were treated with CAS. This represents 5.2 % of a total of 267 patients treated with CAS during the study period. All patients were treated with CAS using an embolic protection device. The proximal balloon protection method was performed in five patients, and the dual protection method using a proximal balloon and distal filter protection was used in nine patients. We examined the change of stenotic lesion, hyperintensity spot in diffusion-weighted imaging (DWI), and perioperative complications after CAS. All near occlusions were successfully dilated. Among 2 of 14 patients, DWI showed 1 and 4 hyperintensity spots. Transient and persistent complications, including neurological deficits, did not occur in any patients. In this small number of cases, CAS using the proximal or dual embolic protection method seems to be a safe and beneficial treatment for ICA near occlusion.



Similar content being viewed by others
References
Brott TG, Hobson RW 2nd, Howard G, Roubin GS, Clark WM, Brooks W, Mackey A, Hill MD, Leimgruber PP, Sheffet AJ, Howard VJ, Moore WS, Voeks JH, Hopkins LN, Cutlip DE, Cohen DJ, Popma JJ, Ferguson RD, Cohen SN, Blackshear JL, Silver FL, Mohr JP, Lal BK, Meschia JF, Investigators CREST (2010) Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 363:11–23
European Carotid Surgery Trialists' Collaborative Group (1998) Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 351:1379–1387
Fox AJ (1993) How to measure carotid stenosis. Radiology 186:316–318
Fox AJ, Eliasziw M, Rothwell PM, Schmidt MH, Warlow CP, Barnett HJ (2005) Identification, prognosis, and management of patients with carotid artery near occlusion. AJNR Am J Neuroradiol 26:2086–2094
González A, Gil-Peralta A, Mayol A, Gonzalez-Marcos JR, Moniche F, Aguilar M, Gutierrez I (2011) Internal carotid artery stenting in patients with near occlusion: 30-day and long-term outcome. AJNR Am J Neuroradiol 32:252–258
Gurm HS, Yadav JS, Fayad P, Katzen BT, Mishkel GJ, Bajwa TK, Ansel G, Strickman NE, Wang H, Cohen SA, Massaro JM, Cutlip DE, Investigators SAPPHIRE (2008) Long-term results of carotid stenting versus endarterectomy in high-risk patients. N Engl J Med 358:1572–1579
Hirata Y, Sakata N, Inoue T, Yasumori K, Yasaka M, Okada Y (2011) Histopathological features with angiographic correlates of internal carotid artery pseudo-occlusion: impact of plaque compositions. Clinical article. J Neurosurg 115:350–358
Jeong YH, Hwang JY, Kim IS, Park Y, Hwang SJ, Lee SW, Kwak CH, Park SW (2010) Adding cilostazol to dual antiplatelet therapy achieves greater platelet inhibition than high maintenance dose clopidogrel in patients with acute myocardial infarction: Results of the adjunctive cilostazol versus high maintenance dose clopidogrel in patients with AMI (ACCEL-AMI) study. Circ Cardiovasc Interv 3:17–26
Lee SW, Park SW, Yun SC, Kim YH, Park DW, Kim WJ, Lee JY, Lee CW, Hong MK, Kim JJ, Park SJ (2010) Triple antiplatelet therapy reduces ischemic events after drug-eluting stent implantation: Drug-Eluting stenting followed by Cilostazol treatment REduces Adverse Serious cardiac Events (DECREASE registry). Am Heart J 159:284–291
Lippman HH, Sundt TM Jr, Holman CB (1970) The poststenotic carotid slim sign: supurious internal carotid hypolasia. Mayo Clin Proc 45:762–767
Matsushige T, Kiura Y, Sakamoto S, Okazaki T, Shinagawa K, Ichinose N, Takasu M, Akiyama Y, Sugiyama K, Kurisu K (2013) Multiple antiplatelet therapy contributes to the reversible high signal spots on diffusion-weighted imaging in elective coiling of unruptured cerebral aneurysm. Neuroradiology 55:449–457
Mehigan JT, Olcott C 4th (1980) The carotid "string" sign. Differential diagnosis and management. Am J Surg 140:137–143
Morgenstern LB, Fox AJ, Sharpe BL, Eliasziw M, Barnett HJ, Grotta JC (1997) The risks and benefits of carotid endarterectomy in patients with near occlusion of the carotid artery. North American Symptomatic Carotid Endarterectomy Trial (NASCET) Group. Neurology 48:911–915
Nikas DN, Ghany MA, Stabile E, Sorropago G, Saccá S, Favero L, Zakaryan N, Reimers B, Rubino P (2010) Carotid artery stenting with proximal cerebral protection for patients with angiographic appearance of string sign. JACC Cardiovasc Interv 3:298–304
North American Symptomatic Carotid Endarterectomy Trial (1991) Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 325:445–453
Rothwell PM, Warlow CP (2000) Low risk of ischemic stroke in patients with reduced internal carotid artery lumen diameter distal to severe symptomatic carotid stenosis: cerebral protection due to low poststenotic flow? On behalf of the European Carotid Surgery Trialists' Collaborative Group. Stroke 31:622–630
Rothwell PM, Gutnikov SA, Warlow CP, European Carotid Surgery Trialist's Collaboration (2003) Reanalysis of the final results of the European Carotid Surgery Trial. Stroke 34:514–523
Sekhar LN, Heros RC, Lotz PR, Rosenbaum AE (1980) Atheromatous pseudo-occlusion of the internal carotid artery. J Neurosurg 52:782–789
Terada T, Tsuura M, Matsumoto H, Masuo O, Tsumoto T, Yamaga H, Itakura T (2006) Endovascular treatment for pseudo-occlusion of the internal carotid artery. Neurosurgery 59:301–309
Yadav JS, Wholey MH, Kuntz RE, Fayad P, Katzen BT, Mishkel GJ, Bajwa TK, Whitlow P, Strickman NE, Jaff MR, Popma JJ, Snead DB, Cutlip DE, Firth BG, Ouriel K, Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy Investigators (2004) Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med 351:1493–1501
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Gerasimos Baltsavias, Zurich, Switzerland
I think the present report about carotid stenting for near occlusion of the cervical carotid artery is interesting for a couple of reasons. Apart from the technical aspects of the described technique which is eloquently presented, it is very interesting to realize how broad is the spectrum of periprocedural management and techniques which are currently used in various departments from different endovascular groups to treat the same disease: From 9Fr guide catheter, double protection devices and triple antiplatelet agents, as in the current group, to 6Fr guide catheter, without protection devices and double antiplatelet agents practiced by other groups including ours. This variety of approaches reminds us once again how a good result can be achieved through different approaches. On the other hand, it highlights the need for larger studies and guidelines at least for some aspects of our practice as the antithrombotic regime. Personally and despite this interesting aspect of this report, I would be rather reluctant to apply or recommend the presented technique and rational. One significant reason, among others, is its contrariety to the highly appreciated “kisss” principle1 (keep it simple, short and safe). Interestingly enough and despite the double and triple protection, the known and clinically silent DWI lesions were still detected postoperatively in a small percentage of patients.
1. Adopted from: A neurosurgeon’s notebook. One man’s way of trying to avoid trouble. CBT Adams. Oxford Blackwell Science. 1998
William W. Ashley Jr. and Christopher M. Loftus, Maywood, USA.
In “Carotid artery stenting using the proximal or dual protection method for near occlusion of the cervical internal carotid artery”, the authors present a retrospective analysis of data from 10 symptomatic and 4 asymptomatic patients with carotid near occlusion treated at a single institution over an approximately 4.5-year period. All 14 patients were male and the mean age was about 75 years of age. They were treated with carotid artery stenting using proximal protection alone (n = 5) or proximal protection combined with distal protection (n = 9). Four patients received triple antiplatelet regimens and 10 received dual antiplatelet regimens. Symptomatic patients were treated within an average of 29 days from onset of symptoms. MRS data is not presented but the mean follow-up was about 17 months (range 5–29). All near occlusions were successfully dilated and there were no transient or permanent complications. There were only 2 patients who showed new small T2 hyperintensities on follow-up MRI.
We would like to thank the authors for presenting this stimulating paper. As they point out, carotid near occlusion is a controversial topic. Thus we appreciate the effort to add further improve the treatment of these complex patients. As the authors themselves point out, this is a small non-randomized retrospective chart review. It is not clear whether the patients were treated by the same practitioner but there is a great deal of variability (antiplatelet regimen, type of stent, type of protection, symptomatic status in the methods used to treat these patients). As a result, no meaningful comparisons can be made between the very small sub-groups. We want to congratulate the authors on excellent results in this small group of difficult patients. We agree that by using careful technique and patient selection, carotid near occlusion can be safely and effectively treated using CAS in some patients.
This paper brings up some very important issues. First, it is not clear as to the true natural history of this phenomenon. How does near occlusion fall in the continuum between a normal patent vessel and a completely occluded one? Are we seeing a point in the temporal progression toward occlusion or is near occlusion a different pathophysiologic phenomenon? Our understanding of the answers to these questions will inform our understanding of the risk of stroke associated with near occlusion. Some analysis of data from the NASCET and ECST trials suggests that carotid near occlusion is low risk while other suggests that treating near occlusion may be of benefit. Unfortunately, due to the relatively rarity of the problem and heterogeneity of the patient population, we do not have adequate evidence from which to draw conclusions. Thus it is still not clear whether we should aggressive treat carotid near occlusion. We must make decisions based on individual patient data. Patient symptoms, the chronicity of the lesion, the type of prior medical therapy, the type and stability of the collateral network and other factors must be considered. Certainly an acute near occlusion in a symptomatic patient seems like a reasonable candidate for therapy. But what of the asymptomatic patient with a chronic narrowing?
Next even if we should treat, what methodology should we use? Again we do not have any randomized controlled trials comparing revascularization to medical therapy for carotid near occlusion. Similarly we do not have good studies comparing CEA to CAS for this subset of patients. This paper highlights the fact that it can be done but we must organize larger well designed studies or, at least, effective registries with standardized treatment regimens to further understand the issue. In this paper the patient population was relatively old with a mean age of 75 and a range from 60 to 84 years of age. If we are to generalize and believe the CREST data, there are at least some of these patients (35 % of patients in the study were over 80 years old) that would be better treated with CEA. It would be interesting to know more about how the authors chose which patients with near occlusion to treat using CAS versus CEA. And were there any near occlusions that they chose not to treat at all and why? Again, we need more studies.
If we are going to treat using CAS, who do we treat and how do we do it? The CREST study suggested that CAS is not inferior to CEA. In reality CAS is probably better for some and CEA better for others. Improvements in technology may result in further expansion of the group who is best treated using CAS. The authors took advantage of multiple strategies to improve the safety and effectiveness of CAS including multiple protection strategies, dual and triple antiplatelet agents and intravascular ultrasound to check the quality of stent placement. They used these techniques in a heterogeneous fashion and achieved excellent results. We need to know more about when to choose each one of these strategies to optimize results. In terms of protection, there is mounting evidence that proximal protection may provide benefit over distal protection because one can avoid crossing the lesion unprotected. But it may be harmful in patients with poor collaterals or the isolated hemisphere. However, the benefit of a dual strategy of proximal and distal protection has not been proven. The authors used a dual strategy when they thought balloon deployment would be less than optimal. But in these cases would it be better to just use a distal protection device? We need to know more about the collateral networks in this group of patients to help us decide which device to use. In those with robust collaterals, proximal protection with or without a DPD may be all that is necessary. The choice to use an additional antiplatelet agent is also controversial. In coronary stenting and peripheral vascular studies, an additional agent has been shown to improve rates of restenosis and need for re-treatment. But it is postulated that is likely relate to providing a failsafe for those that are resistant to ASA or clopidogrel. Indeed, it may be that a more effective pre-treatment analysis of ASA or clopidogrel sensitivity may be more useful and safer than adding a third agent to all patients. The authors chose to use three agents in 4 patients but do not mention why they made this choice. IVUS has been shown to be effective in quality assurance after carotid stenting. It helps discover cases of poor stent apposition, or positioning or intravascular clot extruded through the stent. In small studies, it has not been shown to yield major improvements in outcomes from carotid stenting but has lead to decreased need for retreatment due to restenosis.
In addition to the three studies mentioned in this paper, there are at least three other papers that deal with this topic and show high procedural success rates with good outcomes. Most recently Ruiz-Salmerón et al. (2013) analyzed 54 patient with carotid near occlusion treated with CAS. They used proximal protection in over 50 % of the patients and, like the current study presented herein, they showed a 96 % success rate. However, they also showed that stenting in cases of near-occlusion caused increased detachment of plaque, as shown by higher percentages of macroscopic plaque captured by protection devices (18.5 % vs. 7 %, P = .01) and of perioperative ischemic brain lesions (47 % vs. 31 %, P = .07). They showed that in 30 days of follow-up, the tendency toward adverse neurological events (death, major and minor stroke) was higher in the near-occlusion group (9.2 % vs. 3.2 %, P = .08). These data are different from the experience of the current authors. These differences emphasize the need for further and better controlled studies.
It is an exciting time. We now have many more tools available. This study and others highlight the breadth and variation of techniques that can be employed to treat carotid near occlusion and and also the need also the need for further stringent investigative to help us optimize our treatment choices.
References
Choi BS, Park JW, Shin JE, Lü PH, Kim JK, Kim SJ, Lee DH, Kim JS, Kim HJ, Suh DC. Outcome evaluation of carotid stenting in high-risk patients with symptomatic carotid near occlusion. Interv Neuroradiol. 2010 Sep;16(3):309–16. Epub 2010 Oct 25.
Ruiz-Salmerón RJ, Gamero MA, Carrascosa C, Pérez S, de Araujo D, Marcos F, Rodríguez de Leiras S, Vizcaíno M, Caparrós C, Izquierdo G. Neurologia. Carotid artery stenting: clinical and procedural implications for near-occlusion stenosis. 2013Mar 1. doi: pii: S0213-4853(13)00002-9. 10.1016
Miyamoto N, Naito I, Takatama S, Shimizu T, Iwai T, Shimaguchi H. Urgent stenting for patients with acute stroke due to atherosclerotic occlusive lesions of the cervical internal carotid artery. Neurol Med Chir (Tokyo). 2008 Feb;48(2):49–55; discussion 55–6.
Rights and permissions
About this article
Cite this article
Sakamoto, S., Kiura, Y., Kajihara, Y. et al. Carotid artery stenting using the proximal or dual protection method for near occlusion of the cervical internal carotid artery. Neurosurg Rev 36, 551–558 (2013). https://doi.org/10.1007/s10143-013-0481-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-013-0481-y