Abstract
Methicillin-resistant Staphylococcus aureus (MRSA) is an important cause of nosocomial pneumonia. Compared with glycopeptide antibiotics, linezolid achieves higher lung epithelial lining fluid concentrations, which may have an advantage in treating nosocomial pneumonia patients. The objective of this study was to evaluate the efficacy and safety of linezolid versus vancomycin or teicoplanin for the treatment of nosocomial pneumonia. Data were obtained from the Cochrane Central Register of Controlled Trials and the EMBASE and MEDLINE databases. Randomised controlled studies involving the use of linezolid versus vancomycin or teicoplanin in nosocomial pneumonia patients were included in the study. Twelve linezolid trials were included. There was no statistically significant difference between the two groups in the treatment of nosocomial pneumonia regarding the clinical cure rate [relative risk (RR) = 1.08, 95 % confidence interval (CI) = 1.00–1.17, p = 0.06]. Linezolid was associated with better microbiological eradication rate in nosocomial pneumonia patients compared with glycopeptide antibiotics (RR = 1.16, 95 % CI = 1.03–1.31, p = 0.01). There were no differences in the all-cause mortality (RR = 0.95, 95 % CI = 0.83–1.09, p = 0.46) between the two groups. However, the risks of rash (RR = 0.41, 95 % CI = 0.24–0.71, p = 0.001) and renal dysfunction (RR = 0.41, 95 % CI = 0.27–0.64, p < 0.0001) were higher with glycopeptide antibiotics. Although linezolid was more effective in eradicating microbiology than glycopeptide antibiotics for nosocomial pneumonia patients, it did not demonstrate superiority in clinical cure. The incidences of renal dysfunction and rash are higher in the glycopeptide antibiotics group.
Similar content being viewed by others
Introduction
Pneumonia is the second most common hospital-associated infection in the United States and is associated with substantial mortality, ranging from 24 to 57 % [1, 2]. Gram-positive cocci are responsible for many severe infections in hospital settings [3]. Staphylococcus aureus (S. aureus) is the most common cause of nosocomial pneumonia, accounting for 17 % of isolates in the national nosocomial infections surveillance study [4]. Up to 60 % of S. aureus isolates are reportedly resistant to methicillin [5]. The isolation of methicillin-resistant S. aureus (MRSA) has increased markedly in the past decade [6]. More than 60 % of nosocomial S. aureus isolates are MRSA in China [7]. MRSA represents the most common pathogen associated with nosocomial pneumonia [8]. Although given positive treatment, the mortality rate in patients with MRSA pneumonia ranged from 33 to 55 % [9, 10].
Even though glycopeptide antibiotics (vancomycin and teicoplanin) have long been the standard treatment of MRSA pneumonia, vancomycin-resistant isolates of S. aureus have emerged in the USA [11]. Moreover, serious adverse effects such as renal toxicity limits its use. Linezolid is the first available agent in a new class of antimicrobials called oxazolidinones and was approved in the USA in 2000 for the treatment of MRSA pneumonia. It works via the inhibition of bacterial protein synthesis by preventing the formation of the 70S initiation complex [12], resulting in good efficacy in treating Gram-positive bacterial infections. Linezolid has been shown to have epithelial lining fluid (ELF) concentrations several-fold higher than serum concentrations, and this has been perceived as a significant advantage over vancomycin [13]. On the basis of the better penetration of linezolid into respiratory secretions compared with vancomycin, linezolid has demonstrated a survival advantage in the subgroup of subjects with documented MRSA nosocomial pneumonia [14]. In recent guidelines, it has been suggested that linezolid may be preferred over glycopeptide antibiotics for MRSA pneumonia [15]. This recommendation remains controversial because of its methodologic flaws [16, 17]. Several randomised trials have already been performed to compare the efficacy between linezolid and glycopeptide antibiotics for the treatment of nosocomial pneumonia. A recent meta-analysis of nine randomised controlled trials (RCTs) did not demonstrate the clinical superiority of linezolid versus glycopeptide antibiotics for the treatment of nosocomial pneumonia [18]. Another meta-analysis of eight RCTs acquired similar results [19]. However, only RCTs published until 2011 were included in that meta-analysis. To better assess the value of linezolid versus glycopeptide antibiotics in the treatment of nosocomial pneumonia, we conducted a meta-analysis based on prospectively published RCTs in this area.
Materials and methods
Literature search
Only studies published as an abstract or journal article in English were eligible for this analysis. The literature search was performed on the Cochrane Central Register of Controlled Trials and the MEDLINE and EMBASE databases. The following subject headings were employed: “linezolid”, “vancomycin or teicoplanin”, “pneumonia”. Only RCTs involving nosocomial pneumonia patients were included. Studies published by November 2012 were eligible.
Study selection
The following inclusion criteria were used: (1) RCTs, (2) study population consisting of nosocomial pneumonia patients and (3) intervention therapies consisting of linezolid versus vancomycin or teicoplanin. Studies were excluded if: (1) they were not written in English, (2) the study population did not consist of nosocomial pneumonia patients, (3) the control group did not use glycopeptide antibiotics, (4) the study data were not available from articles and (5) they did not assess clinical treatment success as an end point.
Data extraction and quality assessment
Publication trials included in the final meta-analysis were assessed for validity by two independent reviewers. Data were abstracted by the two reviewers and consensus was reached if there was any disagreement. They examined and recorded the trial characteristics and outcomes, using Jadad scoring to examine the reliability of RCTs [20]. Clinical cure and microbiological eradication were defined at the test of cure evaluation for the clinically evaluable population and the microbiological eradication population, respectively. If the test of cure data were not available, the results from the last follow-up outcome assessment were analysed for these studies. Clinical treatment success in these studies was defined as the resolution of clinical signs and symptoms of pneumonia compared with baseline and microbiologic success was defined as sputum pathogen eradication. Mortality was defined as all-cause deaths. Gastrointestinal events included nausea, vomiting and diarrhoea. Renal failure, rash, anaemia and thrombocytopaenia were defined as reported by the authors of each article.
Statistical analysis
Two reviewers independently extracted the data and used the program Review Manager for the analysis (RevMan Version 5.0 for Windows). The differences observed between the two groups were expressed as the relative risk (RR) along with the 95 % confidence interval (CI). The presence of heterogeneity between trials was assessed by the Chi-square and I2 statistics. Chi-square statistics with a p-value < 0.1 was considered to be significant across trials. Treatment effects across trials were combined using a random effects model (I2 > 0) and a fixed effects model (I2 = 0). The publication bias was assessed using Begg’s and Egger’s tests.
Results
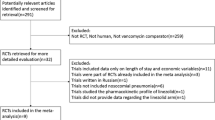
The electronic database search yielded 274 potentially relevant publications, and the process for relevant trials was assessed as shown in Fig. 1. Finally, 12 RCTs fulfilled the inclusion criteria and were subjected to the meta-analysis [21–32]. The study quality was assessed by using the Jadad scores; the quality score ranged from 2 to 4, in which a higher score is associated with better quality. Table 1 lists the key features of the studies included in this meta-analysis.
Clinical cure
The clinical cure (n = 1,327, clinically evaluable population) rates between linezolid and glycopeptide antibiotics for the treatment of nosocomial pneumonia were not statistically significantly different (RR = 1.08, 95 % CI 1.00–1.17, p = 0.06) (Fig. 2). When a low-quality study [23] was removed, the clinical cure rates between the two groups was not statistically significantly different (RR = 1.08, 95 % CI = 1.00–1.17, p = 0.05). If linezolid is compared with vancomycin only (n = 1,171, clinically evaluable population), linezolid was not superior to vancomycin in regards to clinical treatment success (RR = 1.09, 95 % CI = 0.99–1.19, p = 0.07) (Fig. 3). When a low-quality study [23] was removed, the clinical cure rates between the two groups were not statistically significantly different (RR = 1.09, 95 % CI = 1.00–1.19, p = 0.06).
Microbiological eradication
The microbiologically evaluable population of nine randomised trials (n = 800, microbiologically evaluable population) demonstrated the following results of microbiological eradication. Linezolid was associated with a better microbiological eradication rate in nosocomial pneumonia patients compared with glycopeptide antibiotics (RR = 1.16, 95 % CI 1.03–1.31, p = 0.01) (Fig. 4). When a low-quality study [23] was removed, the microbiological eradication rates between the two groups were statistically significantly different (RR = 1.17, 95 % CI = 1.03–1.32, p = 0.01). If linezolid is compared with vancomycin only (n = 766, microbiologically evaluable population), linezolid was more effective than vancomycin in nosocomial pneumonia patients in regards to the microbiological eradication rate (RR = 1.16, 95 % CI 1.02–1.31, p = 0.02) (Fig. 5). When a low-quality study [23] was removed, the microbiological eradication rates between the two groups were statistically significant different (RR = 1.16, 95 % CI = 1.03–1.32, p = 0.02). The microbiologically evaluable population of six randomised trials (n = 539, MRSA evaluable population) demonstrated the results of MRSA eradication (RR = 1.18, 95 % CI 1.01–1.38, p = 0.04).
Adverse effects
Data on the total number of adverse effects (AEs) were reported for nine trials [21–29]. There was no difference in the total number of AEs between the two antibiotics classes [intention to treat (ITT) 2,933 patients, RR = 1.03, 95 % CI 0.74–1.43 p = 0.86). The proportions of AEs such as anaemia (ITT 3,716 patients, RR = 1.14, 95 % CI 0.73–1.79, p = 0.55) and thrombocytopaenia (ITT 3,286 patients, RR = 1.58, 95 % CI 0.75–3.33, p = 0.23) that developed were not statistically significantly different between the two groups. When a low-quality study [23] was removed, the incidences of anaemia and thrombocytopaenia between the two groups were not significantly different. Gastrointestinal events was recorded more commonly in patients receiving linezolid (ITT 3,323 patients, RR = 1.66, 95 % CI 1.03–2.67, p = 0.04). When a low-quality study [23] was removed, the occurrence of gastrointestinal events between the two groups was not statistically significantly different (RR = 1.52, 95 % CI = 0.97–2.39, p = 0.07). However, the risks of rash (ITT 3,570 patients, RR = 0.41, 95 % CI 0.24–0.71, p = 0.001) and renal dysfunction (ITT 3,371 patients, RR = 0.41, 95 % CI 0.27–0.64, p < 0.0001) were higher with glycopeptide antibiotics. When a low-quality study [23] was removed, the risks of rash and renal dysfunction between the two groups remained statistically significantly different.
Mortality
The all-cause mortality during the study period was available in all 12 trials. There was no significant difference in the mortality between linezolid and glycopeptide antibiotics (4,719 patients, RR = 0.95, 95 % CI 0.83–1.09, p = 0.46). When a low-quality study [23] was removed, the mortality between the two groups was not statistically significantly different.
Publication bias
Begg’s funnel plot and Egger’s test were performed to assess the publication bias of the 12 studies. The evaluation of publication bias for clinical cure using the Begg’s test (p = 0.891) and the Egger’s test (p = 0.965) were not significant.
Discussion
This meta-analysis of RCTs comparing linezolid to glycopeptide antibiotics for nosocomial pneumonia does, indeed, support the view that linezolid is more effective in microbiological eradication and MRSA eradication. When compared with vancomycin only, linezolid also has an advantage in microbiological eradication and MRSA eradication. One study reported that linezolid was shown to have ELF concentrations several-fold higher than serum concentrations [13]. However, this study was conducted in healthy volunteers, so these results may not be extrapolated to critically ill patients with ventilation-associated pneumonia (VAP). In this particular patient population, linezolid exhibited 100 % alveolar diffusion, with ELF concentrations equivalent to serum concentrations using both intermittent or continuous infusion [33, 34]. Another study initiated in vivo experiments using a mouse MRSA pneumonia model. This study described the immunomodulatory effects of linezolid on bacteria. The mechanism of immunomodulation was suppressing the virulence factor expression of MRSA and regulating host inflammatory responses [35]. If the microbiological eradication rate was related to the clinical cure rate with pneumonia, then we would expect to observe a statistical advantage for linezolid in our study. However, no statistically significant clinical cure benefits were demonstrated in our results. These results are consistent with other meta-analyses [18, 36].
There were no differences in the total AEs, anaemia, thrombocytopaenia and all-cause mortality between the two groups in our study. The results of this analysis is similar to previous data [37]. However, Kalil et al. reported that, compared with glycopeptide antibiotics, the risk of thrombocytopaenia was approximately doubled in linezolid. The risk of gastrointestinal effects between the two groups was significantly different in our study, and the results are similar to Kalil et al.’s report. One study has shown that linezolid can cause time-dependent myelosuppression [38]. The mean duration of linezolid treatment in our study may have been too short to affect the probability of thrombocytopaenia. Some studies have reported an increased risk of nephrotoxicity during vancomycin treatment [18, 37]. A mouse pneumonia model study has shown that the possibility of increased vancomycin-induced nephrotoxicity cannot be ruled out [39]. In our meta-analysis, an increased risk of nephrotoxicity was also seen in the vancomycin group. In addition, the incidence of rash occurred more frequently during vancomycin treatment.
There are several limitations that should be considered in our meta-analysis. First, some studies were not double-blinded and the lack of blinding could affect the outcomes assessment. Second, several studies did not routinely measure the vancomycin serum concentration, which may have contributed to the lower microbiological eradication rate. Third, only English studies were included in this analysis, which may cause language bias. Finally, the most important limitation was publication bias. In this analysis, although the assessment of publication bias for clinical cure was not significant, the possibility of publication bias may exist in any research, because the negative studies and studies with small sample sizes may be less likely to be published.
In summary, although linezolid was associated with a better microbiological eradication rate in nosocomial pneumonia patients compared with glycopeptide antibiotics, it did not demonstrate superiority in clinical treatment success. Glycopeptide antibiotics are associated with a greater risk of renal dysfunction and rash than linezolid, whereas they showed a lower risk for gastrointestinal events.
References
Emori TG, Gaynes RP (1993) An overview of nosocomial infections, including the role of the microbiology laboratory. Clin Microbiol Rev 6:428–442
Chastre J, Fagon JY (2002) Ventilator-associated pneumonia. Am J Respir Crit Care Med 165:867–903
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB (2004) Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 39:309–317
Richards MJ, Edwards JR, Culver DH, Gaynes R (2000) Nosocomial infections in combined medical–surgical intensive care units in the United States. Infect Control Hosp Epidemiol 21:510–515
Fridkin SK, Hill HA, Volkova NV, Edwards JR, Lawton RM, Gaynes RP, McGowan JE Jr; Intensive Care Antimicrobial Resistance Epidemiology Project Hospitals (2002) Temporal changes in prevalence of antimicrobial resistance in 23 US hospitals. Emerg Infect Dis 8:697–701
Moran GJ, Krishnadasan A, Gorwitz RJ, Fosheim GE, McDougal LK, Carey RB, Talan DA; EMERGEncy ID Net Study Group (2006) Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med 355:666–674
Wang F, Zhu DM, Hu FP, Zhang YY (2001) Surveillance of bacterial resistance among isolates in Shanghai in 1999. J Infect Chemother 7:117–120
Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS (2005) Epidemiology and outcomes of health-care-associated pneumonia: results from a large US database of culture-positive pneumonia. Chest 128:3854–3862
DeRyke CA, Lodise TP Jr, Rybak MJ, McKinnon PS (2005) Epidemiology, treatment, and outcomes of nosocomial bacteremic Staphylococcus aureus pneumonia. Chest 128:1414–1422
González C, Rubio M, Romero-Vivas J, González M, Picazo JJ (1999) Bacteremic pneumonia due to Staphylococcus aureus: a comparison of disease caused by methicillin-resistant and methicillin-susceptible organisms. Clin Infect Dis 29:1171–1177
Wong SS, Ng TK, Yam WC, Tsang DN, Woo PC, Fung SK, Yuen KY (2000) Bacteremia due to Staphylococcus aureus with reduced susceptibility to vancomycin. Diagn Microbiol Infect Dis 36:261–268
Stevens DL, Dotter B, Madaras-Kelly K (2004) A review of linezolid: the first oxazolidinone antibiotic. Expert Rev Anti Infect Ther 2:51–59
Conte JE Jr, Golden JA, Kipps J, Zurlinden E (2002) Intrapulmonary pharmacokinetics of linezolid. Antimicrob Agents Chemother 46:1475–1480
Wunderink RG, Rello J, Cammarata SK, Croos-Dabrera RV, Kollef MH (2003) Linezolid vs vancomycin: analysis of two double-blind studies of patients with methicillin-resistant Staphylococcus aureus nosocomial pneumonia. Chest 124:1789–1797
American Thoracic Society; Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171:388–416
Powers JH, Ross DB, Lin D, Soreth J (2004) Linezolid and vancomycin for methicillin-resistant Staphylococcus aureus nosocomial pneumonia: the subtleties of subgroup analyses. Chest 126:314–316
Kalil AC, Puumala SE, Stoner J (2004) Unresolved questions with the use of linezolid vs vancomycin for nosocomial pneumonia. Chest 125:2370–2371
Kalil AC, Murthy MH, Hermsen ED, Neto FK, Sun JF, Rupp ME (2010) Linezolid versus vancomycin or teicoplanin for nosocomial pneumonia: a systematic review and meta-analysis. Crit Care Med 38:1802–1808
Walkey AJ, O’Donnell MR, Wiener RS (2011) Linezolid vs glycopeptide antibiotics for the treatment of suspected methicillin-resistant Staphylococcus aureus nosocomial pneumonia: a meta-analysis of randomized controlled trials. Chest 139:1148–1155
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12
Wilcox M, Nathwani D, Dryden M (2004) Linezolid compared with teicoplanin for the treatment of suspected or proven Gram-positive infections. J Antimicrob Chemother 53:335–344
Wunderink RG, Mendelson MH, Somero MS, Fabian TC, May AK, Bhattacharyya H, Leeper KV Jr, Solomkin JS (2008) Early microbiological response to linezolid vs vancomycin in ventilator-associated pneumonia due to methicillin-resistant Staphylococcus aureus. Chest 134:1200–1207
Kohno S, Yamaguchi K, Aikawa N, Sumiyama Y, Odagiri S, Aoki N, Niki Y, Watanabe S, Furue M, Ito T, Croos-Dabrera R, Tack KJ (2007) Linezolid versus vancomycin for the treatment of infections caused by methicillin-resistant Staphylococcus aureus in Japan. J Antimicrob Chemother 60:1361–1369
Lin DF, Zhang YY, Wu JF, Wang F, Zheng JC, Miao JZ, Zheng LY, Sheng RY, Zhou X, Shen HH, Ijzerman MM, Croos-Dabrera RV, Sheng W (2008) Linezolid for the treatment of infections caused by Gram-positive pathogens in China. Int J Antimicrob Agents 32:241–249
Stevens DL, Herr D, Lampiris H, Hunt JL, Batts DH, Hafkin B (2002) Linezolid versus vancomycin for the treatment of methicillin-resistant Staphylococcus aureus infections. Clin Infect Dis 34:1481–1490
Wunderink RG, Cammarata SK, Oliphant TH, Kollef MH; Linezolid Nosocomial Pneumonia Study Group (2003) Continuation of a randomized, double-blind, multicenter study of linezolid versus vancomycin in the treatment of patients with nosocomial pneumonia. Clin Ther 25:980–992
Jaksic B, Martinelli G, Perez-Oteyza J, Hartman CS, Leonard LB, Tack KJ (2006) Efficacy and safety of linezolid compared with vancomycin in a randomized, double-blind study of febrile neutropenic patients with cancer. Clin Infect Dis 42:597–607
Deville JG, Adler S, Azimi PH, Jantausch BA, Morfin MR, Beltran S, Edge-Padbury B, Naberhuis-Stehouwer S, Bruss JB (2003) Linezolid versus vancomycin in the treatment of known or suspected resistant Gram-positive infections in neonates. Pediatr Infect Dis J 22:S158–S163
Kaplan SL, Deville JG, Yogev R, Morfin MR, Wu E, Adler S, Edge-Padbury B, Naberhuis-Stehouwer S, Bruss JB; Linezolid Pediatric Study Group (2003) Linezolid versus vancomycin for treatment of resistant Gram-positive infections in children. Pediatr Infect Dis J 22:677–686
Rubinstein E, Cammarata S, Oliphant T, Wunderink R; Linezolid Nosocomial Pneumonia Study Group (2001) Linezolid (PNU-100766) versus vancomycin in the treatment of hospitalized patients with nosocomial pneumonia: a randomized, double-blind, multicenter study. Clin Infect Dis 32:402–412
Cepeda JA, Whitehouse T, Cooper B, Hails J, Jones K, Kwaku F, Taylor L, Hayman S, Shaw S, Kibbler C, Shulman R, Singer M, Wilson AP (2004) Linezolid versus teicoplanin in the treatment of Gram-positive infections in the critically ill: a randomized, double-blind, multicentre study. J Antimicrob Chemother 53:345–355
Wunderink RG, Niederman MS, Kollef MH, Shorr AF, Kunkel MJ, Baruch A, McGee WT, Reisman A, Chastre J (2012) Linezolid in methicillin-resistant Staphylococcus aureus nosocomial pneumonia: a randomized, controlled study. Clin Infect Dis 54:621–629
Boselli E, Breilh D, Rimmelé T, Djabarouti S, Toutain J, Chassard D, Saux MC, Allaouchiche B (2005) Pharmacokinetics and intrapulmonary concentrations of linezolid administered to critically ill patients with ventilator-associated pneumonia. Crit Care Med 33:1529–1533
Boselli E, Breilh D, Caillault-Sergent A, Djabarouti S, Guillaume C, Xuereb F, Bouvet L, Rimmelé T, Saux MC, Allaouchiche B (2012) Alveolar diffusion and pharmacokinetics of linezolid administered in continuous infusion to critically ill patients with ventilator-associated pneumonia. J Antimicrob Chemother 67:1207–1210
Yoshizawa S, Tateda K, Saga T, Ishii Y, Yamaguchi K (2012) Virulence-suppressing effects of linezolid on methicillin-resistant Staphylococcus aureus: possible contribution to early defervescence. Antimicrob Agents Chemother 56:1744–1748
Falagas ME, Siempos II, Vardakas KZ (2008) Linezolid versus glycopeptide or beta-lactam for treatment of Gram-positive bacterial infections: meta-analysis of randomised controlled trials. Lancet Infect Dis 8:53–66
Beibei L, Yun C, Mengli C, Nan B, Xuhong Y, Rui W (2010) Linezolid versus vancomycin for the treatment of gram-positive bacterial infections: meta-analysis of randomised controlled trials. Int J Antimicrob Agents 35:3–12
Kuter DJ, Tillotson GS (2001) Hematologic effects of antimicrobials: focus on the oxazolidinone linezolid. Pharmacotherapy 21:1010–1013
Docobo-Pérez F, López-Rojas R, Domínguez-Herrera J, Jiménez-Mejias ME, Pichardo C, Ibáñez-Martínez J, Pachón J (2012) Efficacy of linezolid versus a pharmacodynamically optimized vancomycin therapy in an experimental pneumonia model caused by methicillin-resistant Staphylococcus aureus. J Antimicrob Chemother 67:1961–1967
Acknowledgements
This work was supported by grants from the Natural Science Foundation of Jiangsu Province (no. BK 2011603) and the Foundation of Southeast University (no. seucx 201107).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
H. Jiang and R.-N. Tang contribute equally to this article and should be considered as co-first authors.
Rights and permissions
About this article
Cite this article
Jiang, H., Tang, RN. & Wang, J. Linezolid versus vancomycin or teicoplanin for nosocomial pneumonia: meta-analysis of randomised controlled trials. Eur J Clin Microbiol Infect Dis 32, 1121–1128 (2013). https://doi.org/10.1007/s10096-013-1867-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-013-1867-z