Abstract
Introduction
While porcine-based biologic meshes are increasingly used for hernia repair, little data exist on tissue responses to such products. Host foreign body reaction, local inflammation, and wound healing are principally controlled by monocytes/macrophages (M/MØs). Exaggerated activation of M/MØs may deleteriously influence mesh integration and remodeling. We hypothesized that common porcine meshes induce the differential activation of M/MØs in vitro.
Materials and methods
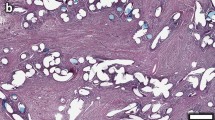
Samples of four acellular porcine-derived meshes, CollaMend™ (CM; C.R. Bard/Davol), Permacol™ (PC; TSL/Covidien), Strattice™ (ST; LifeCell), and Surgisis® (SS; Cook Biotech), were exposed to mononuclear cells derived from the peripheral blood of six healthy subjects. Following a 7-day incubation period, supernatants were assayed for interleukin-1beta (IL-1β), interleukin-6 (IL-6), interleukin-8 (IL-8), and vascular endothelial growth factor (VEGF) using a multiplex bead-based immunoassay system. The four groups were compared using analysis of variance (ANOVA) and Student’s t-test.
Results
Each mesh type induced differential mononuclear cell activation in vitro. The mean IL-1β expressions for CM (7,195 pg/ml) and PC (4,215 pg/ml) were significantly higher compared to ST and SS (123 and 998 pg/ml, respectively; P < 0.05). Similar trends were also seen for IL-6 (range 445–70,729 pg/ml), IL-8 (range 11,640–1,045,938 pg/ml), and VEGF (range 686–7,133 pg/ml).
Conclusion
For the first time, we demonstrated that porcine meshes induce M/MØ activation in vitro. CM and PC (chemically crosslinked dermis) induced significantly higher cytokine expression compared to ST (non-crosslinked dermis) and SS (small intestine submucosa). These differences are likely related to proprietary processing methods and/or the extent of collagen crosslinking. Further understanding of immunologic effects of porcine-derived biologic meshes will not only allow for a comparison between existing products, but it may also lead to mesh modifications and improvement of their clinical performance.

Similar content being viewed by others
References
Usher FC, Ochsner J, Tuttle LL Jr (1958) Use of marlex mesh in the repair of incisional hernias. Am Surg 24:969–974
Bachman S, Ramshaw B (2008) Prosthetic material in ventral hernia repair: how do I choose? Surg Clin North Am 88:101–112, ix
Udwadia TE (2006) Inguinal hernia repair: the total picture. J Min Access Surg 2:144–146
Jin J, Rosen MJ, Blatnik J, McGee MF, Williams CP, Marks J, Ponsky J (2007) Use of acellular dermal matrix for complicated ventral hernia repair: does technique affect outcomes? J Am Coll Surg 205:654–660
Milburn ML, Holton LH, Chung TL, Li EN, Bochicchio GV, Goldberg NH, Silverman RP (2008) Acellular dermal matrix compared with synthetic implant material for repair of ventral hernia in the setting of peri-operative Staphylococcus aureus implant contamination: a rabbit model. Surg Infect (Larchmt) 9:433–442
Saettele TM, Bachman SL, Costello CR, Grant SA, Cleveland DS, Loy TS, Kolder DG, Ramshaw BJ (2007) Use of porcine dermal collagen as a prosthetic mesh in a contaminated field for ventral hernia repair: a case report. Hernia 11:279–285
Bellows CF, Albo D, Berger DH, Awad SS (2007) Abdominal wall repair using human acellular dermis. Am J Surg 194:192–198
Hiles M, Record Ritchie RD, Altizer AM (2009) Are biologic grafts effective for hernia repair?: a systematic review of the literature. Surg Innov 16:26–37
Schuster R, Singh J, Safadi BY, Wren SM (2006) The use of acellular dermal matrix for contaminated abdominal wall defects: wound status predicts success. Am J Surg 192:594–597
Shaikh FM, Giri SK, Durrani S, Waldron D, Grace PA (2007) Experience with porcine acellular dermal collagen implant in one-stage tension-free reconstruction of acute and chronic abdominal wall defects. World J Surg 31:1966–1972; discussion 1973–1974, 1975
Badylak SF (2004) Xenogeneic extracellular matrix as a scaffold for tissue reconstruction. Transpl Immunol 12:367–377
Badylak SF, Valentin JE, Ravindra AK, McCabe GP, Stewart-Akers AM (2008) Macrophage phenotype as a determinant of biologic scaffold remodeling. Tissue Eng Part A 14:1835–1842
Gordon S, Taylor PR (2005) Monocyte and macrophage heterogeneity. Nat Rev Immunol 5:953–964
Schachtrupp A, Klinge U, Junge K, Rosch R, Bhardwaj RS, Schumpelick V (2003) Individual inflammatory response of human blood monocytes to mesh biomaterials. Br J Surg 90:114–120
Schutte RJ, Parisi-Amon A, Reichert WM (2009) Cytokine profiling using monocytes/macrophages cultured on common biomaterials with a range of surface chemistries. J Biomed Mater Res A 88:128–139
Anderson JM, Rodriguez A, Chang DT (2008) Foreign body reaction to biomaterials. Semin Immunol 20:86–100
Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M (2008) Growth factors and cytokines in wound healing. Wound Repair Regen 16:585–601
Schutte RJ, Xie L, Klitzman B, Reichert WM (2009) In vivo cytokine-associated responses to biomaterials. Biomaterials 30:160–168
Orenstein S, Qiao Y, Kaur M, Klueh U, Kreutzer D, Novitsky Y (2010) In vitro activation of human peripheral blood mononuclear cells induced by human biologic meshes. J Surg Res 158:10–14
Orenstein SB, Qiao Y, Kaur M, Klueh U, Kreutzer DL, Novitsky YW (2009) Human monocyte activation by biologic and biodegradable meshes in vitro. Surg Endosc (in press)
Usher FC (1959) Further observations on the use of marlex mesh: a new technique for the repair of inguinal hernias. Am Surg 25:792–795
Usher FC, Hill JR, Ochsner JL (1959) Hernia repair with Marlex mesh. A comparison of techniques. Surgery 46:718–724
Johnson J, Roth JS, Hazey JW, Pofahl WE (2004) The history of open inguinal hernia repair. Curr Surg 61:49–52
Jansen PL, Mertens Pr P, Klinge U, Schumpelick V (2004) The biology of hernia formation. Surgery 136:1–4
Kaback LA, Smith TJ (1999) Expression of hyaluronan synthase messenger ribonucleic acids and their induction by interleukin-1beta in human orbital fibroblasts: potential insight into the molecular pathogenesis of thyroid-associated ophthalmopathy. J Clin Endocrinol Metab 84:4079–4084
Sandor M, Xu H, Connor J, Lombardi J, Harper JR, Silverman RP, McQuillan DJ (2008) Host response to implanted porcine-derived biologic materials in a primate model of abdominal wall repair. Tissue Eng Part A 14:2021–2031
Xu H, Wan H, Sandor M, Qi S, Ervin F, Harper JR, Silverman RP, McQuillan DJ (2008) Host response to human acellular dermal matrix transplantation in a primate model of abdominal wall repair. Tissue Eng Part A 14:2009–2019
Chaplin JM, Costantino PD, Wolpoe ME, Bederson JB, Griffey ES, Zhang WX (1999) Use of an acellular dermal allograft for dural replacement: an experimental study. Neurosurgery 45:320–327
Tarhan E, Cakmak O, Ozdemir BH, Akdogan V, Suren D (2008) Comparison of AlloDerm, fat, fascia, cartilage, and dermal grafts in rabbits. Arch Facial Plast Surg 10:187–193
Khor E (1997) Methods for the treatment of collagenous tissues for bioprostheses. Biomaterials 18:95–105
Schmidt CE, Baier JM (2000) Acellular vascular tissues: natural biomaterials for tissue repair and tissue engineering. Biomaterials 21:2215–2231
Gouk SS, Lim TM, Teoh SH, Sun WQ (2008) Alterations of human acellular tissue matrix by gamma irradiation: histology, biomechanical property, stability, in vitro cell repopulation, and remodeling. J Biomed Mater Res B Appl Biomater 84:205–217
Mosser DM (2003) The many faces of macrophage activation. J Leukoc Biol 73:209–212
Mosser DM, Edwards JP (2008) Exploring the full spectrum of macrophage activation. Nat Rev Immunol 8:958–969
Mosser DM, Zhang X (2008) Activation of murine macrophages. Curr Protoc Immunol Chapter 14: Unit 14.2
Zhang X, Goncalves R, Mosser DM (2008) The isolation and characterization of murine macrophages. Curr Protoc Immunol Chapter 14: Unit 14.1
Badylak SF, Gilbert TW (2008) Immune response to biologic scaffold materials. Semin Immunol 20:109–116
Gilbert TW, Sellaro TL, Badylak SF (2006) Decellularization of tissues and organs. Biomaterials 27:3675–3683
Ansaloni L, Cambrini P, Catena F, Di Saverio S, Gagliardi S, Gazzotti F, Hodde JP, Metzger DW, D’Alessandro L, Pinna AD (2007) Immune response to small intestinal submucosa (surgisis) implant in humans: preliminary observations. J Invest Surg 20:237–241
Ansaloni L, Catena F, Coccolini F, Gazzotti F, D’Alessandro L, Pinna AD (2009) Inguinal hernia repair with porcine small intestine submucosa: 3-year follow-up results of a randomized controlled trial of Lichtenstein’s repair with polypropylene mesh versus surgisis inguinal hernia matrix. Am J Surg 198:303–312
Franklin ME Jr, Treviño JM, Portillo G, Vela I, Glass JL, González JJ (2008) The use of porcine small intestinal submucosa as a prosthetic material for laparoscopic hernia repair in infected and potentially contaminated fields: long-term follow-up. Surg Endosc 22:1941–1946
Pu LL (2005) Small intestinal submucosa (Surgisis) as a bioactive prosthetic material for repair of abdominal wall fascial defect. Plast Reconstr Surg 115:2127–2131
Ayubi FS, Armstrong PJ, Mattia MS, Parker DM (2008) Abdominal wall hernia repair: a comparison of Permacol and Surgisis grafts in a rat hernia model. Hernia 12:373–378
Trabuco EC, Zobitz ME, Klingele CJ, Gebhart JB (2007) Effect of host response (incorporation, encapsulation, mixed incorporation and encapsulation, or resorption) on the tensile strength of graft-reinforced repair in the rat ventral hernia model. Am J Obstet Gynecol 197:638.e1–638.e6
Xu H, Wan H, Zuo W, Sun W, Owens RT, Harper JR, Ayares DL, McQuillan DJ (2009) A porcine-derived acellular dermal scaffold that supports soft tissue regeneration: removal of terminal galactose-alpha-(1,3)-galactose and retention of matrix structure. Tissue Eng Part A 15:1807–1819
Connor J, McQuillan D, Sandor M, Wan H, Lombardi J, Bachrach N, Harper J, Xu H (2009) Retention of structural and biochemical integrity in a biological mesh supports tissue remodeling in a primate abdominal wall model. Regen Med 4:185–195
Acknowledgment
This study was funded by institutional support from the University of Connecticut Health Center.
Conflict of interest statement
Y.W.N. has received consulting and/or speaking fees from LifeCell Corp., C.R. Bard Inc., and Covidien. The other co-authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Orenstein, S.B., Qiao, Y., Klueh, U. et al. Activation of human mononuclear cells by porcine biologic meshes in vitro. Hernia 14, 401–407 (2010). https://doi.org/10.1007/s10029-010-0634-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-010-0634-7