Abstract
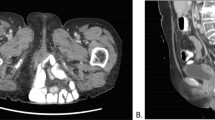
Parasacral hernias are defects through the pelvic floor which occur as the result of sacral resection. These defects are often large, and are frequently the result of treatment for sacral malignancies. This report documents the case of a 71-year-old woman who underwent radical coccygectomy and partial sacrectomy for a chordoma and subsequently presented 1 year later with a large parasacral hernia. The defect was repaired using an acellular human dermis graft with a gluteus maximus muscle-advancement flap overlay. This article summarizes the current literature of this challenging clinical problem, and examines the use of acellular human dermis in the repair of complex hernias.





Similar content being viewed by others
References
Junge K, Krones CJ, Rosch R, Fackeldey V, Schumpelick V (2003) Mesh reconstruction preventing sacral herniation. Hernia 7:224–226
Miles WK, Chang DW, Kroll SS, Miller MJ, Langstein HN, Reece GP, Evans GRD, Robb GL (2000) Reconstruction of large sacral defects following total sacrectomy. Plastic Reconstr Surg 105:2387–2394
Kaplan LJ, Santora TA (1996) Technique of sacral hernia repair. Am Surg 62:762–765
Galandiuk S, Jorden J, Mahid S, McCaferty MH, Tobin G 2005 The use of tissue flaps as an adjunct to pelvic surgery. Am J Surg 190:186–190
Bakx R, van Lanschot JJ, Zoetmulder FA (2004) Sacral resection in cancer surgery: Surgical technique and experience in 26 procedures. J Am Coll Surg 198:846–851
Buinewicz B, Rosen B (2004) Acellular cadaveric dermis (AlloDerm): a new alternative for abdominal hernia repair. Ann Plastic Surg 52:188–194
Silverman RP, Li EN, Holton III LH, Sawan KT, Goldberg NH (2004) Ventral hernia repair using allogenic acellular dermal matric in a swine model. Hernia 8:336–342
Butler CE, Prieto VG (2004) Reduction of adhesions with composite AlloDerm/polyproplylene mesh implants for abdominal wall reconstruction. Plastic Reconstr Surg 114:464–743
Butler CE, Langstein HN, Kronowitz SJ (2005) Pelvic, abdominal, and chest wall reconstruction with AlloDerm in patients at increased risk for mesh-related complications. Plastic Reconstr Surg 116:1263–1275
Vecchia LD, Engum S, Kogon B, Jensen E, Davis M, Grosfeld J (1999) Evaluation of small intestine submucosa and acellular dermis as diaphragmatic prostheses. J Pediatr Surg 34:167–171
Clemons JL, Myers DL, Aguilar VC, Arya LA 2003 Vaginal paravaginal repair with an AlloDerm graft. Am J Obstet Gynecol 189:1612–1619
Hirsch EF (2004) Repair of an abdominal wall defect after a salvage laparotomy for sepsis. J Am Coll Surg 198:324–328
Choe JM, Kothandapani R, James L, Bowling D (2001) Autologous, cadaveric and synthetic materials used in sling surgery: comparative biomechanical analysis. Urology 58:482–486
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brizendine, J.B., LeFaivre, J.F., Yost, M.J. et al. Reconstruction of parasacral hernia with acellular human dermis graft . Hernia 10, 360–363 (2006). https://doi.org/10.1007/s10029-006-0092-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-006-0092-4