Abstract
Purpose
To describe the early effectiveness of microvascular decompression (MVD) for the treatment of spasmodic torticollis (ST).
Methods
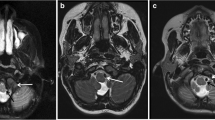
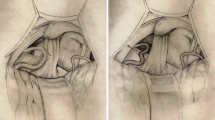
Twelve patients with spasmodic torticollis were treated by microvascular decompression of the accessory nerves using a microscopic neurosurgical technique via the retrosigmoid approach. The most common compressing blood vessels were the ipsilateral posterior inferior cerebral artery (PICA) and/or the vertebral artery. The intraoperative monitor was introduced to detect the accessory nerve and to avoid unnecessary damage to the nerve.
Results
Ten patients were cured (83%), and the other two (17%) improved with moderate spasms. In most cases, the improvement was noticed 1 week after the operation. No operation-related complications were observed during the follow-up period, which ranged from 2 months to 3 years.
Conclusions
The early effect of MVD for some patients with spasmodic torticollis was satisfactory, but the long-term results need to be assessed further.







Similar content being viewed by others
References
Adams CB (1989) Microvascular compression: an alternative view and hypothesis. J Neurosurg 70:1–12
Bertrand C, Molina-Negro P, Martinez SN (1978) Combined stereotactic and peripheral surgical approach for spasmodic torticollis. Appl Neurophysiol 41:122–133
Choppy-Jacolin M, Ferrey G, Demaria C (1977) A psychometric stury of 34 patients afflicted with spasmodic torticollis. Acta Neurol Scand 55:483–492
Colbassani HJ Jr, Wood JH (1986) Management of spasmodic torticollis. Surg Neurol 25:153–158
Duane DD (1988) Spasmodic torticollis. Adv Neurol 49:135–150
Freckmann N, Hagenah R, Herrmann HD, Muller D (1981) Treatment of neurogenic torticollis by microvascular lysis of the accessory nerve roots—indication, technique, and first results. Acta Neurochir (Wien) 59:167–175
Freckmann N, Hagenah R, Herrmann HD, Muller D (1986) Bilateral microsurgical lysis of the spinal accessory nerve roots for treatment of spasmodic torticollis. Follow-up of 33 cases. Acta Neurochir (Wien) 83:47–53
Herz E, Glaser GH (1949) Spasmodic torticollis; clinical evaluation. Arch Neurol Psychiatry 61:227–239
Jannetta PJ, Segal R, Wolfson SK Jr (1985) Neurogenic hypertension: etiology and surgical treatment. I. Observations in 53 patients. Ann Surg 201:391–398
Jho HD, Jannetta PJ (1995) Microvascular decompression for spasmodic torticollis. Acta Neurochir (Wien) 134:21–26
Magyar-Lehmann S, Antonini A, Roelcke U, Maguire RP, Missimer J, Meyer M, Leenders KL (1997) Cerebral glucose metabolism in patients with spasmodic torticollis. Mov Disord 12:704–708
Motomochi M, Makita Y, Nabeshima S, Itagaki T, Tei T, Imataka K (1983) Surgical treatment and long-term result of spasmodic torticollis. Neurol Med Chir (Tokyo) 23:741–746
Mundinger F, Riechert T, Disselhoff J (1972) Long-term results of stereotactic treatment of spasmodic torticollis. Confin Neurol 34:41–50
Nagata K, Matsui T, Joshita H, Shigeno T, Asano T (1989) Surgical treatment of spasmodic torticollis: effectiveness of microvascular decompression. No To Shinkei 41:97–102
Nakashima K, Thompson PD, Rothwell JC, Day BL, Stell R, Marsden CD (1989) An exteroceptive reflex in the sternocleidomastoid muscle produced by electrical stimulation of the supraorbital nerve in normal subjects and patients with spasmodic torticollis. Neurology 39:1354–1358
Pagni CA, Naddeo M, Faccani G (1985) Spasmodic torticollis due to neurovascular compression of the 11th nerve. Case report. J Neurosurg 63:789–791
Shima F, Fukui M, Kitamura K, Kuromatsu C, Okamura T (1988) Diagnosis and surgical treatment of spasmodic torticollis of 11th nerve origin. Neurosurgery 22:358–363
Acknowledgments
Thanks to the patients who were generous enough to share their photos in this report.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
In spite of the popularity of the microvascular decompression (MVD) procedure for treating "cranial nerve hyperactive syndromes," there are very few reports in the literature on its application to the accessory nerve for treating spasmodic torticollis. Therefore, the present article is interesting, although the follow-up is short for a number of cases in the series. A useful effect is reported in the majority of the patients. What is puzzling is the better effectiveness for the sternocleidomastoidian muscle than for the trapezius muscle. For a stronger demonstration it would have been important to have a comparison between the postoperative EMG recordings and the preoperative ones. The authors have promised to provide with these data in a future article. For most teams using neurovascular decompression, as well as most of the teams dealing with movement disorders, spasmodic torticollis fits more within the frame of dystonia-dyskinesia pathologies than within the so-called hyperactive cranial nerve syndromes.
The relatively good results obtained by the Shangai neurosurgical team are likely related to the rigorous selection of the patients, namely those having spasmodic muscles confined to the neck. However, even in such patients the spasmodic disorders generally also affect a large number of muscles innervated by the cervical motor roots, and this bilaterally. But it might be that the neurovascular conflict on the accessory rootlets triggers more general dysfunction. Understanding this pathology needs a lot of further work, both electrophysiological and neurosurgical. The authors have to be acknowledged for their reported experience.
Doctor Marc Sindou, M.D., D. Dc.
University of Lyon
Rights and permissions
About this article
Cite this article
Sun, K., Lu, Y., Hu, G. et al. Microvascular decompression of the accessory nerve for treatment of spasmodic torticollis: early results in 12 cases. Acta Neurochir 151, 1251–1257 (2009). https://doi.org/10.1007/s00701-009-0455-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-009-0455-6