Abstract
Background
We investigated the mode of progression of intraductal papillary-mucinous neoplasm of the pancreas (IPMN) in patients who underwent follow-up in order to elucidate the characteristics of malignancy and to establish an effective treatment strategy.
Methods
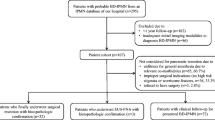
Fifty-one patients with IPMN (branch-duct type, 47; main-duct type, 4) who had undergone follow-up study by endoscopic ultrasonography (EUS) were included (mean follow-up duration, 41.0 ± 32.3 months; average number of EUS examinations performed during follow-up, 4.4). Chronological changes in EUS findings and histological findings of resected specimens were evaluated.
Results
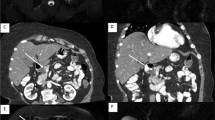
Of the patients with the branch-duct type, only 2% showed enlargement of the dilated branches. In the main-duct-type group, an increase in size of the main pancreatic duct (MPD) was observed in 75% of the patients. In 14 patients with papillary protrusions, an increase in size and lateral spread was observed in 71% and 43%, respectively. No patients developed invasive cancer. In 15 patients who had thick septum-like structures (TSS), the development of papillary protrusions and that of invasive cancer were observed in 53% and 13%, respectively. Twenty-nine patients who had thin septum-like structures showed no change. Two patients with dense multilocular large cysts and TSS developed invasive cancer without change in the cystic lesions. One patient developed carcinoma with multifocal stromal invasion.
Conclusions
Patients with branch-duct type IPMNs without papillary protrusions or TSS are not immediate candidates for surgery. Those who have small papillary protrusions have a benign course. It is recommended that patients with the large branch-duct type with TSS should undergo surgery. Attention should be paid to the entire pancreas when performing follow-up examinations in patients with branch-duct type IPMN, as invasive ductal adenocarcinoma can develop at a site in the pancreas different from that of the IPMN.
Similar content being viewed by others
References
K Ohhashi Y Murakami M Maruyama T Takekoshi H Ohta I Ohhashi et al. (1982) ArticleTitleFour cases of mucus-secreting pancreatic cancer (in Japanese) Prog Dig Endosc 20 348–51
DS Longnecker RH Hruben G Adler G Kloppel (2000) Intraductal papillary-mucinous neoplasms of the pancreas. World Health Organization classification of tumors International Agency for Research on Cancer Lyon 237–40
G Kobayashi N Fujita Y Noda K Kimura A Yago T Yamazaki et al. (1999) Histologic features and prognosis of mucinous cystic tumor of the pancreas A Wakui H Yamauchi K Ouchi (Eds) Carcinoma of the pancreas and biliary tract Tohoku University Press Sendai 213–8
G Kobayashi N Fujita Y Noda K Kimura A Yago T Yamazaki et al. (1999) Three morphological types of mucinous cystic tumor of the pancreas: correlation between morphological features and histological findings A Wakui H Yamauchi K Ouchi (Eds) Carcinoma of the pancreas and biliary tract Tohoku University Press Sendai 203–12
H Maguchi (1994) ArticleTitleClinicopathological and diagnostic study of mucin producing pancreatic tumors (in Japanese with English abstract) Jpn J Gastroenterol 91 1003–15
M Kobari S Egawa K Shibuya H Shimamura M Sunamura K Takeda et al. (1999) ArticleTitleIntraductal papillary mucinous tumors of the pancreas comprise two clinical subtypes Arch Surg 134 1131–6 Occurrence Handle10.1001/archsurg.134.10.1131 Occurrence Handle10522860
K Yamaguchi Y Ogawa K Chijiiwa Y Tanaka (1996) ArticleTitleMucin-hypersecreting tumors of the pancreas: assessing the grade of malignancy preoperatively Am J Surg 171 427–31 Occurrence Handle10.1016/S0002-9610(97)89624-9 Occurrence Handle8604836
W Kimura N Sasahira T Yoshikawa T Muto M Makuuchi (1996) ArticleTitleDuct-ectatic type of mucin producing tumor of the pancreas. New concept of pancreas neoplasia Hepatogastroenterology 43 692–709 Occurrence Handle8799417
M Sugiyama Y Atomi (1998) ArticleTitleIntraductal papillary mucinous tumors of the pancreas: imaging studies and treatment strategies Ann Surg 228 685–91 Occurrence Handle10.1097/00000658-199811000-00008 Occurrence Handle9833807
H Kubo Y Chijiiwa K Akahoshi S Hamada N Harada T Sumii et al. (2001) ArticleTitleIntraductal papillary-mucinous tumors of the pancreas: differential diagnosis between benign and malignant tumors by endoscopic ultrasonography Am J Gastroenterol 96 1429–34 Occurrence Handle10.1111/j.1572-0241.2001.03794.x Occurrence Handle11374678
J Compagno JE Oertel (1978) ArticleTitleMucinous cystic neoplasms of the pancreas with overt and latent malignancy (cystadenocarcinoma and cystadenoma) Am Soc Clin Pathol 69 573–80
G Klöppel (1984) Pancreatic non-endocrine tumors G Kloppel PH Heitz (Eds) Pancreatic pathology Churchill Livingstone Edinburgh 79–113
EV Loftus BA Olivares-Pakzad KP Batts MC Adkins DH Stephens MG Sarr et al. (1996) ArticleTitleIntraductal papillary-mucinous tumors of the pancreas: clinicopathological features, outcome, and nomenclature Gastroenterology 110 1909–18 Occurrence Handle10.1053/gast.1996.v110.pm8964418 Occurrence Handle8964418
C Cellier E Cuillerier L Palazzo F Rickaert JF Flejou B Napoleon et al. (1998) ArticleTitleIntraductal papillary and mucinous tumors of the pancreas: accuracy of preoperative computed tomography, endoscopic retrograde pancreatography and endoscopic ultrasonography, and long-term outcome in a large surgical series Gastrointest Endosc 47 42–9 Occurrence Handle9468422
G Kobayashi N Fujita S Lee K Kimura T Ikeda T Toyohara et al. (1990) ArticleTitleCorrelation between ultrasonographic findings and pathological diagnosis of the mucin producing tumor of the pancreas (in Japanese with English abstract) Jpn J Gastroenterol 87 235–42
K Koito T Namieno T Nagakawa T Shyonai N Hirokawa K Morita (1997) ArticleTitleSolitary cystic tumor of the pancreas: EUS-pathologic correlation Gastrointest Endosc 45 268–76 Occurrence Handle9087833
K Inui S Nakazawa J Yoshino H Yamachika N Kanemaki T Wakabayashi et al. (1998) ArticleTitleMucin-producing tumor of the pancreas—intraluminal ultrasonography Hepatogastroenterology 45 1996–2000 Occurrence Handle9951853
M Sugiyama Y Atomi M Saito (1998) ArticleTitleIntraductal papillary tumors of the pancreas: evaluation with endoscopic ultrasonography Gastrointest Endosc 48 164–71 Occurrence Handle9717782
K Yamao K Ohashi T Nakamura T Suzuki Y Watanabe Y Shimizu et al. (2001) ArticleTitleEvaluation of various imaging methods in the differential diagnosis of intraductal papillary-mucinous tumor (IPMT) of the pancreas Hepatogastroenterology 48 962–6 Occurrence Handle11490849
T Hara T Yamaguchi T Ishihara T Tsuyuguchi F Kondo K Kato et al. (2002) ArticleTitleDiagnosis and patient management of intraductal papillary mucinous tumor of the pancreas by using peroral pancreatoscopy and intraductal ultrasonography Gastroenterology 122 34–43 Occurrence Handle10.1053/gast.2002.30337 Occurrence Handle11781278
T Obara H Maguchi Y Saitoh A Itoh S Arisato T Ashida et al. (1993) ArticleTitleMucin-producing tumor of the pancreas: natural history and serial pancreatogram changes Am J Gastroenterol 88 564–8 Occurrence Handle8385881
Y Suzuki Y Atomi M Sugiyama S Isaji K Inui W Kimura et al. (2004) ArticleTitleCystic neoplasm of the pancreas: a Japanese multiinstitutional study of intraductal papillary mucinous tumor and mucinous cystic tumor Pancreas 28 241–6 Occurrence Handle10.1097/00006676-200404000-00005 Occurrence Handle15084964
VP Collins RK Loeffler H Tivey (1956) ArticleTitleObservations on growth rates of human tumors AJR Am J Roentgenol 76 988–1000
A Yanagisawa Y Kato K Ohtake T Kitagawa K Ohhashi M Hori et al. (1991) ArticleTitleKi-ras point mutation in ductectatic-type mucinous cystic neoplasms of the pancreas Jpn J Cancer Res 82 1057–60 Occurrence Handle1955373
T Izawa T Obara S Tanno Y Mizukami N Yanagawa Y Kohgo (2001) ArticleTitleClonality and field cancerization in intraductal papillary-mucinous tumors of the pancreas Cancer 92 1807–17 Occurrence Handle10.1002/1097-0142(20011001)92:7<1807::AID-CNCR1697>3.0.CO;2-0 Occurrence Handle11745253
K Yamaguchi J Ohuchida T Ohtsuka K Nakano M Tanaka (2002) ArticleTitleIntraductal papillary-mucinous tumor of the pancreas concomitant with ductal carcinoma of the pancreas Pancreatology 2 484–90 Occurrence Handle10.1159/000064716 Occurrence Handle12378117
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kobayashi, G., Fujita, N., Noda, Y. et al. Mode of progression of intraductal papillary-mucinous tumor of the pancreas: analysis of patients with follow-up by EUS. J Gastroenterol 40, 744–751 (2005). https://doi.org/10.1007/s00535-005-1619-7
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s00535-005-1619-7