Abstract
Purpose
In febrile neutropenia (FN), no reliable marker has been identified to discriminate between severe infection and other causes of fever early in the clinical course. Since lipopolysaccharide-binding protein (LBP) has proven to be an accurate biomarker of bacteremia/clinical sepsis in critically ill non-immunocompromised infants and children, we performed a prospective study to determine the diagnostic accuracy of LBP in children with FN.
Methods
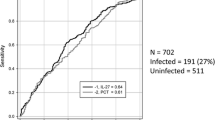
Concentrations of LBP, procalcitonin (PCT), interleukin-6 (IL-6), and C-reactive protein (CRP) were prospectively measured on two consecutive days in 90 FN episodes experienced by 47 children. Receiver operating characteristic curve analysis was performed for each biomarker to predict bacteremia/clinical sepsis and severe sepsis.
Results
Eighteen of the 90 episodes were classified as bacteremia/clinical sepsis. On both days 1 and 2, all biomarkers had a low to intermediate diagnostic accuracy for sepsis, and no significant differences were found between them (area under the curve (AUC) for LBP, 0.648 and 0.714; for PCT, 0.665 and 0.744; for IL-6, 0.775 and 0.775; and for CRP, 0.695 and 0.828). Comparison of their AUCs to the AUC of maximum body temperature on admission (AUC = 0.668) also failed to show any significant differences. In severe sepsis, however, the best diagnostic accuracies were found for IL-6 and PCT (AUC 0.892 and 0.752, respectively), and these were significantly higher than those for LBP (AUC 0.566) on admission.
Conclusions
On admission and 24 h later, the LBP concentration is less accurate for predicting bacteremia/clinical sepsis compared to IL-6, PCT, and CRP.


Similar content being viewed by others
References
Bodey GP, Buckley M, Sathe YS, Freireich EJ (1966) Quantitative relationships between circulating leukocytes and infection in patients with acute leukemia. Ann Intern Med 64:328–340
Levy MM, Fink MP, Marshall JC et al (2003) SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med 31:1250–1256
Goldstein B, Giroir B, Randolph A, the members of the International Consensus Conference on Pediatric Sepsis (2005) International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 6(Suppl 3):2–8
Hakim H, Flynn PM, Knapp KM, Srivastava DK, Gaur AH (2009) Etiology and clinical course of febrile neutropenia in children with cancer. J Pediatr Hematol Oncol 31:623–629
Phillips B, Wade R, Stewart LA, Sutton AJ (2010) Systematic review and meta-analysis of the discriminatory performance of risk prediction rules in febrile neutropenic episodes in children and young people. Eur J Cancer 46:2950–2964
Phillips B, Selwood K, Lane SM et al (2007) Variation in policies for the management of febrile neutropenia in United Kingdom Children's Cancer Study Group centres. Arch Dis Child 92:495–498
Boragina M, Patel H (2007) Management of febrile neutropenia in pediatric oncology patients: a Canadian survey. Pediatr Blood Cancer 48:521–526
Sakr Y, Sponholz C, Tuche F et al (2008) The role of procalcitonin in febrile neutropenic patients: review of literature. Infection 36:396–407
Phillips RS, Wade R, Lehrnbecher T et al (2012) Systematic review and meta-analysis of the value of initial biomarkers in predicting adverse outcome in febrile neutropenic episodes in children and young people with cancer. BMC Med 10:6. doi:10.1186/1741-7015-10-6
Pavcnik Arnol M, Hojker S, Derganc M (2004) Lipopolysaccharide-binding protein in critically ill neonates and children with suspected infection: comparison with procalcitonin, interleukin-6, and C-reactive protein. Intensive Care Med 30:1454–1460
Groselj-Grenc M, Ihan A, Pavcnik-Arnol M et al (2009) Neutrophil and monocyte CD64 indexes, lipopolysaccharide-binding protein, procalcitonin and C-reactive protein in sepsis of critically ill neonates and children. Intensive Care Med 35:1950–1958
Oude Nijhuis CSM, Vellenga E, Daenen SMGJ et al (2003) Lipopolysaccharide-binding protein: a possible diagnostic marker for Gram-negative bacteremia in neutropenic cancer patients. Intensive Care Med 29:2157–2161
Zweigner J, Schumann RR, Wener JR (2006) The role of lipopolysaccharide binding protein in modulating the innate immune response. Microbes Infect 8:946–952
Triantafilou M, Triantafilou K (2002) Lipopolysaccharide recognition: CD14, TLRs and the LPS-activation cluster. Trends Immunol 23:301–304
Arditi M, Zhou J, Dorio R et al (1993) Endotoxin-mediated endothelial cell injury and activation: role of soluble CD14. Infect Immun 61:3149–3156
Faure E, Equils O, Sieling PA (2000) Bacterial lipopolysaccharide activates NF-kappaB trough toll-like receptor 4 (TLR-4) in cultured human dermal endothelial cells. Differential expression of TLR-4 and TLR-2 in endothelial cells. J Biol Chem 275:11058–11063
Blairon L, Wittebole X, Laerre PF (2003) Lipopolysaccharide-binding protein serum levels in patients with severe sepsis due to Gram-positive and fungal infections. J Infect Dis 187:287–291
Ubenauf KM, Krueger M, Henneke P, Benrer R (2007) Lipopolysaccharide binding protein is a potential marker for invasive bacterial infections in children. Pediatr Infect Dis J 26:159–162
Pavare J, Grope I, Kalnins I, Gardovska D (2010) High-mobility group box-1 protein, lipopolysaccharide-binding protein, interleukin-6 and C-reactive protein in children with community acquired infections and bacteremia: a prospective study. BMC Infect Dis 10:1–9
Garner JS, Jarvis WR, Emori TG et al (1988) CDC definitions for nosocomial infections. Am J Hospital Infect 16:128–140
Buchheidt D, Böhme A, Cornely OA et al (2001) Dokumentierte Infektionen bei Neutropenie-Empfehlungen zu Diagnostik und Therapie. Dtsch Med Wochenschr 126:1085–1090
Buchheidt D, Böhme A, Cornely OA et al (2003) Diagnosis and treatment of documented infections in neutropenic patients—recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol 82(Suppl 2):S127–S132
De Pauw B, Walsh TJ, Donnelly JP et al (2008) Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 46:1813–1821
Penel N, Fournier C, Clisant S, N'Guyen M (2004) Causes of fever and value of C-reactive protein and procalcitonin in differentiating infections from paraneoplastic fever. Support Care Cancer 12:593–598
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 148:839–843
Anisimova NLU, Gromova EG, Kuznetsova LS, Kiselevski MV (2011) Prognostic value of lipopolysaccharide and lipopolysaccharide-binding protein serum levels in cancer patients with sepsis. Zh Mikrobiol Epidemiol Immunobiol 2:82–84
Carcillo JA (2006) Searching for the etiology of systemic inflammatory response syndrome: is SIRS occult endotoxemia? Intensive Care Med 32:181–184
Pavcnik Arnol M, Hojker S, Derganc M (2007) Lipopolysaccharide-binding protein, lipopolysaccharide, and soluble CD14 in sepsis of critically ill neonates and children. Intensive Care Med 33:1025–1032
Meynaar IA, Droog W, Batstra M et al (2011) In critically ill patients, serum procalcitonin is more useful in differentiating between sepsis and SIRS than CRP, IL-6, or LBP. Crit Care Res Pract 2011:594645. doi:10.1155/2011/594645
Kitanovski L, Jazbec J, Hojker S et al (2006) Diagnostic accuracy of procalcitonin and interleukin-6 values for predicting bacteremia and clinical sepsis in febrile neutropenic children with cancer. Eur J Clin Microbiol Infect Dis 25:413–415
Lin SG, Hou TY, Huang DH et al (2012) Role of procalcitonin in the diagnosis of severe infection in pediatric patients with fever and neutropenia—a systemic review and meta-analysis. Pediatr Infect Dis J 31(10):e182–e188. doi:10.1097/INF.0b013e31825da45d
Svaldi M, Hirber J, Lanthaler AI et al (2001) Procalcitonin-reduced sensitivity and specificity in heavily leucopenic and immunosupressed patients. Br J Hematol 115:53–57
Povoa P, Souza-Danta VC, Soares M, Salluh JIF (2011) C-reactive protein in critically ill cancer patients with sepsis: influence of neutropenia. Crit Care 15(3):R129. doi:10.1186/cc10242
Secmeer G, Devrim I, Kara A et al (2007) Role of procalcitonin and CRP in differentiating a stable from a deteriorating clinical course in pediatric febrile neutropenia. J Pediatr Hematol Oncol 29:107–111
Santolaya ME, Alvarez AM, Aviles CL et al (2008) Predictors of severe sepsis not clinically apparent during the first twenty-four hours of hospitalization in children with cancer, neutropenia, and fever: a prospective, multicenter trial. Pediatr Infect Dis J 27:538–543
Santolaya ME, Cofre J, Beresi V (1994) C reactive protein: a valuable aid for the management of febrile children with cancer and neutropenia. Clin Infect Dis 18:589–595
Heney D, Lewis IJ, Evans SW et al (1992) Interleukin-6 and its relationship to C-reactive protein and fever in children with febrile neutropenia. J Infect Dis 165:886–890
Meckler G, Lindemulder S (2009) Fever and neutropenia in pediatric patients with cancer. Emerg Med Clin North Am 27:525–544
Santolaya ME, Alvarez AM, Becker A et al (2001) Prospective, multicenter evaluation of risk factors associated with invasive bacterial infection in children with cancer, neutropenia and fever. J Clin Oncol 19:3415–3421
Hatzistilanou M, Rekliti A, Athanassiadou F, Catriu D (2010) Procalcitonin as an early marker of bacterial infection in neutropenic febrile children with acute lymphoblastic leukemia. Inflamm Res 59:339–347
Nuutila J, Hohenthal U, Laitinen I et al (2007) Simultaneous quantitative analysis of FcgammaRI (CD64) expression on neutrophils and monocytes: a new, improved way to detect infections. J Immunol Methods 328:189–200
Groselj-Grenc M, Ihan A, Derganc M (2008) Neutrophil and monocyte CD64 and CD163 expression in critically ill neonates and children with sepsis: comparison of fluorescence intensities and calculated indexes. Mediat Inflamm 2008:202646. doi:10.1155/2008/202646
Gericke GH, Ericson SG, Pan L, Mills LE, Guyre PM, Ely P (1995) Mature polymorphonuclear leukocytes express high-affinity receptors for IgG (Fc gama RI) after stimulation with granulocyte colony-stimulating factor (G-CSF). J Leukoc Biol 57:455–461
Kwofie L, Rapoport BL, Fickl H et al (2012) Evaluation of circulating soluble triggering receptor expressed on myeloid cells-1 (sTREM-1) to predict risk profile, response to antimicrobial therapy, and development of complications in patients with chemotherapy-associated febrile neutropenia: a pilot study. Ann Hematol 91:605–611
Miedema KG, de Bont ES, Elferink RF et al (2011) The diagnostic value of CRP, IL-8, PCT, and sTREM-1 in the detection of bacterial infections in pediatric oncology patients with febrile neutropenia. Support Care Cancer 19:1593–1600
Acknowledgments
This study was supported by the Slovenian Research Agency, grants no. J3-2184 and J3-4220. The authors thank Dr. Dianne Jones for language review.
Conflict of interest
All authors declare no conflict of interest. Authors have full control of all primary data and agree to allow the journal to review their data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kitanovski, L., Jazbec, J., Hojker, S. et al. Diagnostic accuracy of lipopolysaccharide-binding protein for predicting bacteremia/clinical sepsis in children with febrile neutropenia: comparison with interleukin-6, procalcitonin, and C-reactive protein. Support Care Cancer 22, 269–277 (2014). https://doi.org/10.1007/s00520-013-1978-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1978-1