Abstract
Background
The initial focus of simulation in surgical education was to provide instruction in procedural tasks and technical skills. Recently, the importance of instruction in nontechnical areas, such as communication and teamwork, was realized. On rotation, the surgical resident requires proficiency in both technical and non-technical skills through the entire patient care pathway, i.e., pre-, intra- and postoperatively.
Methods
The focus was upon implementation of a biliary disease-based surgical simulation curriculum. The cornerstones of this module were clinical care pathway simulation sessions, at the commencement and conclusion of the 3 days. Each resident completed a simulated outpatient encounter with a standardized patient (SP) presenting with biliary colic, performed a laparoscopic cholecystectomy on a porcine model in a simulated operating room and completed an uncomplicated follow-up visit with the same SP. Assessments of resident performance were collected for every pathway scenario using standardized assessment forms approved by the American Board of Surgery. Additional formative sessions included hands-on, didactic and SP encounter sessions.
Results
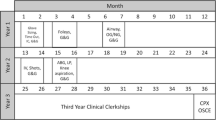
The biliary surgical simulation pathway curriculum was successful implemented over the course of a 3-day, immersive module. The curriculum was delivered within the Penn Medicine Clinical Simulation Center and accommodated six junior surgical resident learners. The curriculum was divided into 4-h sessions, each led by a department faculty member. The cost of the implementation approximated $17,500 (USD).
Conclusion
It is imperative that surgical residents undergo simulation training directly linked to their hospital responsibilities so as to provide immediate performance improvement and reduce errors in the clinical environment. This pathway curriculum has successfully shown the feasibility to implement this novel approach to surgical simulation for junior resident training at an academic medical center. Such a patient-focused approach to surgical simulation should lead to higher-quality training for residents and supports the use of this pathway curriculum in the future.


Similar content being viewed by others
References
Aggarwal R, Mytton OT, Derbrew M, Hananel D, Heydenburg M, Issenberg B, MacAulay C, Mancini ME, Morimoto T, Soper N, Ziv A, Reznick R (2010) Training and simulation for patient safety. Qual Saf Health Care 19(Suppl 2):i34–i43. doi:10.1136/qshc.2009.038562
Scott DJ, Dunnington GL (2008) The new ACS/APDS Skills Curriculum: moving the learning curve out of the operating room. J Gastrointest Surg 12(2):213–221. doi:10.1007/s11605-007-0357-y
ACGME Program Requirements for Graduate Medical Education in General Surgery. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/440_general_surgery_01012008_07012012.pdf
Peters JH, Fried GM, Swanstrom LL, Soper NJ, Sillin LF, Schirmer B, Hoffman K, Committee SF (2004) Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery 135:21–27. doi:10.1016/S0039-6060(03)00156-9
General Surgery Resident Performance Assessments. http://www.absurgery.org/default.jsp?certgsqe_resassess
Aggarwal R, Darzi A (2006) Technical-skills training in the 21st century. N Engl J Med 355(25):2695–2696. doi:10.1056/NEJMe068179
Nasca TJ, Philibert I, Brigham T, Flynn TC (2012) The next GME accreditation system–rationale and benefits. N Engl J Med 366(11):1051–1056. doi:10.1056/NEJMsr1200117
SCORE|General Surgery Resident Curriculum Portal
Aggarwal R, Undre S, Moorthy K, Vincent C, Darzi A (2004) The simulated operating theatre: comprehensive training for surgical teams. Qual Saf Health Care 13(Suppl 1):i27–i32. doi:10.1136/qhc.13.suppl_1.i27
Pucher PH, Aggarwal R, Srisatkunam T, Darzi A (2014) Validation of the simulated ward environment for assessment of ward-based surgical care. Ann Surg 259(2):215–221. doi:10.1097/SLA.0b013e318288e1d4
Aggarwal R, Ward J, Balasundaram I, Sains P, Athanasiou T, Darzi A (2007) Proving the effectiveness of virtual reality simulation for training in laparoscopic surgery. Ann Surg 246(5):771–779. doi:10.1097/SLA.0b013e3180f61b09
Aggarwal R, Grantcharov TP, Eriksen JR, Blirup D, Kristiansen VB, Funch-Jensen P, Darzi A (2006) An evidence-based virtual reality training program for novice laparoscopic surgeons. Ann Surg 244(2):310–314. doi:10.1097/01.sla.0000218094.92650.44
Aggarwal R, Crochet P, Dias A, Misra A, Ziprin P, Darzi A (2009) Development of a virtual reality training curriculum for laparoscopic cholecystectomy. Br J Surg 96(9):1086–1093. doi:10.1002/bjs.6679
Larson JL, Williams RG, Ketchum J, Boehler ML, Dunnington GL (2005) Feasibility, reliability and validity of an operative performance rating system for evaluating surgery residents. Surgery 138(4):640–647; discussion 647–649. doi:10.1016/j.surg.2005.07.017
Norcini JJ, Blank LL, Duffy FD, Fortna GS (2003) The mini-CEX: a method for assessing clinical skills. Ann Intern Med 138(6):476–481
Williams NN, Mittal MK, Dumon KR, Matika G, Pray LA, Resnick AS, Morris JB (2011) Penn medicine clinical simulation center. J Surg Educ 68(1):83–86. doi:10.1016/j.jsurg.2010.05.028
Vassiliou MC, Dunkin BJ, Fried GM, Mellinger JD, Trus T, Kaneva P, Lyons C, Korndorffer JR Jr, Ujiki M, Velanovich V, Kochman ML, Tsuda S, Martinez J, Scott DJ, Korus G, Park A, Marks JM (2014) Fundamentals of endoscopic surgery: creation and validation of the hands-on test. Surg Endosc 28(3):704–711. doi:10.1007/s00464-013-3298-4
Mery CM, Greenberg JA, Patel A, Jaik NP (2008) Teaching and assessing the ACGME competencies in surgical residency. Bull Am Coll Surg 93(7):39–47
Curriculum Outline for Resident Education—A SAGES Guideline. http://www.sages.org/publications/guidelines/curriculum-outline-for-resident-education/
Surgical Skills Curriculum|American College of Surgeons. http://www.facs.org/education/surgicalskills.html
Sachdeva AK (2010) Establishment of American College of Surgeons-accredited Education Institutes: the dawn of a new era in surgical education and training. J Surg Educ 67(4):249–250. doi:10.1016/j.jsurg.2010.07.014
Gawande AA, Thomas EJ, Zinner MJ, Brennan TA (1999) The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery 126(1):66–75. doi:10.1067/msy.1999.98664
Newton RC, Mytton OT, Aggarwal R, Runciman WB, Free M, Fahlgren B, Akiyama M, Farlow B, Yaron S, Locke G, Whittaker S (2010) Making existing technology safer in healthcare. Qual Saf Health Care 19(Suppl 2):i15–i24. doi:10.1136/qshc.2009.038539
Disclosures
Joseph Buchholz, Charles Vollmer, Kiyoyuki Miyasaka, Denise LaMarra and Rajesh Aggarwal have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented at the SAGES 2014 Annual Meeting, April 2–5, 2014, Salt Lake City, Utah.
Rights and permissions
About this article
Cite this article
Buchholz, J., Vollmer, C.M., Miyasaka, K.W. et al. Design, development and implementation of a surgical simulation pathway curriculum for biliary disease. Surg Endosc 29, 68–76 (2015). https://doi.org/10.1007/s00464-014-3661-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3661-0