Abstract
Background
Surgery residents are required to achieve performance milestones to advance in their residency. Level-specific, technical performance norms that could be used as milestones, however, do not currently exist. Our aim was to develop level-specific, technical performance norms for general surgery residents on select simulated tasks across multiple institutions.
Study Design
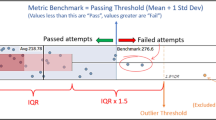
An IRB-approved, prospective, multi-institutional collaborative study with voluntary participation of residents was undertaken at the start of the 2011–2012 academic year. General surgery residents (PGY I–V) from seven institutions were tested on three laparoscopic and five open simulated surgical tasks, and their performance was assessed based on task time and errors. Means and standard deviations of performance for each resident level were calculated and compared. Residents with performance 1 standard deviation below the mean were considered outliers.
Results
A total of 147 residents were evaluated. Mean resident age was 28 ± 3 years; 42 % were female; and they had attended 74 different medical schools. Senior residents (PGY III–V) had more clinical and simulator experience than junior residents (PGY I–II) (p < 0.001). Resident performance scores progressively increased in all tasks reaching a plateau at a lower PGY level for open tasks. Depending on the task, 0–18 % of residents were outliers. When surveyed, 66 % of residents agreed that national performance norms for residents should exist.
Conclusions
Performance norms were established for select tasks in a representative sample of US surgery residents. Such performance norms allow a more informed assessment of resident skill through comparison to national data and enable the identification of outliers who may benefit from additional training.

Similar content being viewed by others
Abbreviations
- ACGME:
-
Accreditation Council for Graduate Medical Education
- ABS:
-
American Board of Surgery
- ANOVA:
-
Analysis of variance
- APDS:
-
Association of Program Directors in Surgery
- ASE:
-
Association for Surgical Education
- UTSW:
-
Fundamentals of Laparoscopic Surgery (FLS), University of Texas Southwestern’s
- IRB:
-
Institutional review board
- OR:
-
Operating room
- PGY:
-
Post-graduate year
References
Magill R (2004) Motor learning and control: concepts and applications, 7th edn. McGraw-Hill, New York
Nasca TJ, Philibert I, Brigham T, Flynn TC (2012) The next GME accreditation system—rationale and benefits. N Engl J Med 366:1051–1056
Chiang L, Chui CH, Low Y, Jacobsen AS (2011) Perforation: a rare complication of choledochal cysts in children. Pediatr Surg Int 27:823–827
Flin R, OCP, Crichton M (2009) Safety at the sharp end: a guide to non-technical skills. Ashgate Publishing Ltd, England
Fried GM, Feldman LS, Vassiliou MC, Fraser SA, Stanbridge D, Ghitulescu G, Andrew CG (2004) Proving the value of simulation in laparoscopic surgery. Ann Surg 240:518–525 discussion 525–518
Sachdeva AK, Buyske J, Dunnington GL, Sanfey HA, Mellinger JD, Scott DJ, Satava R, Fried GM, Jacobs LM, Burns KJ (2011) A new paradigm for surgical procedural training. Curr Probl Surg 48:854–968
Peters JH, Fried GM, Swanstrom LL, Soper NJ, Sillin LF, Schirmer B, Hoffman K (2004) Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery 135:21–27
Goova MT, Hollett LA, Tesfay ST, Gala RB, Puzziferri N, Kehdy FJ, Scott DJ (2008) Implementation, construct validity, and benefit of a proficiency-based knot-tying and suturing curriculum. J Surg Educ 65:309–315
Mashaud LB, Arain NA, Hogg DC, Scott DJ (2013) Development, validation, and implementation of a cost-effective intermediate-level proficiency-based knot-tying and suturing curriculum for surgery residents. J Surg Educ 70:193–199
Ritter EM, Scott DJ (2007) Design of a proficiency-based skills training curriculum for the fundamentals of laparoscopic surgery. Surg Innov 14:107–112
Ericsson KA (2004) Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med 79:S70–S81
Stefanidis D (2010) Optimal acquisition and assessment of proficiency on simulators in surgery. Surg Clin North Am 90:475–489
Acknowledgments
We thank Rich Milner for help with data collection and Amanda Walters for help with statistical analysis. This study was funded by the first collaborative grant of the Association for Surgical Education and Association for Program Directors in Surgery.
Disclosures
Drs. Edelman, Korndorffer, Sievers, Grewal, and Scott have no conflicts of interest or financial ties to disclose. Dr. Stefanidis is on the speakers’ bureau of Gore and Bard and has a completed grant from Ethicon. Dr. Paige is a co-editor for Simulation in Radiology (Oxford University Press), and Dr. Nepomnayshy is the recipient of a collaborative research grant from ASE/APD.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was funded by the first collaborative grant of the ASE/APDS and was presented from the podium at the 2012 ASE meeting in San Diego, CA.
Rights and permissions
About this article
Cite this article
Stefanidis, D., Grewal, H., Paige, J.T. et al. Establishing technical performance norms for general surgery residents. Surg Endosc 28, 3179–3185 (2014). https://doi.org/10.1007/s00464-014-3582-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3582-y