Abstract
Background
It is well known that carbon dioxide (CO2) is absorbed faster in the body than air and also that it is rapidly excreted through respiration. This study aimed to investigate the safety of CO2 insufflation used for esophageal and gastric endoscopic submucosal dissection (ESD) in patients under deep sedation.
Methods
Patients with either early gastric or esophageal cancers that could be resected by ESD were enrolled in this study from March 2007 to July 2008 and randomly assigned to undergo ESD procedures with CO2 insufflation (CO2 group) or air insufflation (air group). A TOSCA measurement system and TOSCA 500 monitor were used to measure and monitor both transcutaneous partial pressure of CO2 (PtcCO2) and oxygen saturation (SpO2).
Results
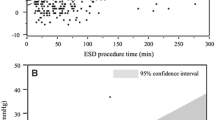
The study enrolled 89 patients and randomly assigned them to a CO2 group (45 patients) or an air group (44 patients). The mean CO2 group versus air group measurements were as follows: PtcCO2 (49.1 ± 5.0 vs. 50.1 ± 5.3 mmHg; nonsignificant difference [NS]), maximum PtcCO2 (55.1 ± 6.5 vs. 56.8 ± 7.0 mmHg; NS), PtcCO2 elevation (9.1 ± 5.4 vs. 11.4 ± 5.6 mmHg; p = 0.054), SpO2 (99.0 ± 0.7% vs. 99.0 ± 1.0%; NS), minimum SpO2 (96.5 ± 2.4% vs. 95.4 ± 3.3%; p = 0.085), and SpO2 depression (2.4 ± 2.3% vs. 3.3 ± 2.9%; NS). The PtcCO2 and SpO2 measurements were similar in the two groups, but the CO2 group was better than the air group in PtcCO2 elevation and minimum SpO2.
Conclusions
The findings demonstrated CO2 insufflation to be as safe as air insufflation for upper gastrointestinal tract ESDs performed for patients under deep sedation without evidencing any adverse effects.



Similar content being viewed by others
References
Hussein AM, Bartram CI, Williams CB (1984) Carbon dioxide insufflation for more comfortable colonoscopy. Gastrointest Endosc 30:68–70
Stevenson GW, Wilson JA, Wilkinson J, Norman G, Goodacre RL (1992) Pain following colonoscopy: elimination with carbon dioxide. Gastrointest Endosc 38:564–567
Church J, Delaney C (2003) Randomized, controlled trial of carbon dioxide insufflation during colonoscopy. Dis Colon Rectum 46:322–326
Bretthauer M, Thiis-Evensen E, Huppertz-Hauss G, Gisselsson L, Grotmol T, Skovlund E, Hoff G (2002) NORCCAP (Norwegian colorectal cancer prevention): a randomised trial to assess the safety and efficacy of carbon dioxide versus air insufflation in colonoscopy. Gut 50:604–607
Bretthauer M, Lynge AB, Thiis-Evensen E, Hoff G, Fausa O, Aabakken L (2005) Carbon dioxide insufflation in colonoscopy: safe and effective in sedated patients. Endoscopy 37:706–709
Bretthauer M, Seip B, Aasen S, Kordal M, Hoff G, Aabakken L (2007) Carbon dioxide insufflation for more comfortable endoscopic retrograde cholangiopancreatography: a randomized, controlled, double-blind trial. Endoscopy 39:58–64
Minami S, Gotoda T, Ono H, Oda I, Hamanaka H (2006) Complete endoscopic closure of gastric perforation induced by endoscopic resection of early gastric cancer using endoclips can prevent surgery (with video). Gastrointest Endosc 63:596–601
Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Muraki Y, Ono S, Kobayashi K, Hashimoto T, Yamamichi N, Tateishi A, Shimizu Y, Oka M, Ogura K, Kawabe T, Ichinose M, Omata M (2006) Successful nonsurgical management of perforation complicating endoscopic submucosal dissection of gastrointestinal epithelial neoplasms. Endoscopy 38:1001–1006
Oyama T, Tomori A, Hotta K, Morita S, Kominato K, Tanaka M, Miyata Y (2005) Endoscopic submucosal dissection of early esophageal cancer. Clin Gastroenterol Hepatol 3:67–70
Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Muraki Y, Ono S, Yamamichi N, Tateishi A, Shimizu Y, Oka M, Ogura K, Kawabe T, Ichinose M, Omata M (2006) Endoscopic submucosal dissection of esophageal squamous cell neoplasms. Clin Gastroenterol Hepatol 4:688–694
Ono H, Kondo H, Gotoda T, Shirao K, Yamaguchi H, Saito D, Hosokawa K, Shimoda T, Yoshida S (2001) Endoscopic mucosal resection for treatment of early gastric cancer. Gut 48:225–229
Yamamoto H, Kawata H, Sunada K, Sasaki A, Nakazawa K, Miyata T, Sekine Y, Yano T, Satoh K, Ido K, Sugano K (2003) Successful en bloc resection of large superficial tumors in the stomach and colon using sodium hyaluronate and small-caliber-tip transparent hood. Endoscopy 35:690–694
Yahagi N, Fujishiro M, Kakushima N, Kobayashi K, Hashimoto T, Oka M (2004) Endoscopic submucosal dissection for early gastric cancer using the tip of an electrosurgical snare (thin type). Dig Endosc 16:34–38
Oda I, Gotoda T, Hamanaka H (2005) Endoscopic submucosal dissection for early gastric cancer: technical feasibility, operation time, and complications from a large consecutive series. Dig Endosc 17:54–58
Saito Y, Uraoka T, Matsuda T, Emura F, Ikehara H, Mashimo Y, Kikuchi T, Fu KI, Sano Y, Saito D (2007) Endoscopic treatment of large superficial colorectal tumors: a case series of 200 endoscopic submucosal dissections (with video). Gastrointest Endosc 66:966–973
Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Muraki Y, Ono S, Yamamichi N, Tateishi A, Oka M, Ogura K, Kawabe T, Ichinose M, Omata M (2007) Outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms in 200 consecutive cases. Clin Gastroenterol Hepatol 5:678–683
Gotoda T (2007) Endoscopic resection of early gastric cancer. Gastric Cancer 10:1–11
Takizawa K, Oda I, Gotoda T, Yokoi C, Matsuda T, Saito Y, Saito D, Ono H (2008) Routine coagulation of visible vessels may prevent delayed bleeding after endoscopic submucosal dissection: an analysis of risk factors. Endoscopy 40:179–183
Kimball EJ, Rollins MD, Mone MC, Hansen HJ, Baraghoshi GK, Johnston C, Day ES, Jackson PR, Payne M, Barton RG (2006) Survey of intensive care physicians on the recognition and management of intraabdominal hypertension and abdominal compartment syndrome. Crit Care Med 34:2340–2348
Williams C (1986) Who’s for CO2? Gastrointest Endosc 32:365–367
Hayakawa M, Gando S, Kameue T, Morimoto Y, Kemmotsu O (2002) Abdominal compartment syndrome and intrahepatic portal venous gas: a possible complication of endoscopy. Intensive Care Med 28:1680–1681
Peppriell JE, Bacon DR (2000) Acute abdominal compartment syndrome with pulseless electrical activity during colonoscopy with conscious sedation. J Clin Anesth 12:216–219
Rizzo AG, Sample GA (2003) Thoracic compartment syndrome secondary to a thoracic procedure: a case report. Chest 124:1164–1168
van Mook WN, Huslewe-Evers RP, Ramsay G (2002) Abdominal compartment syndrome. Lancet 360:1502
Saito Y, Uraoka T, Matsuda T, Emura F, Ikehara H, Mashimo Y, Kikuchi T, Kozu T, Saito D (2007) A pilot study to assess the safety and efficacy of carbon dioxide insufflation during colorectal endoscopic submucosal dissection with the patient under conscious sedation. Gastrointest Endosc 65:537–542
Gotoda T, Kondo H, Ono H, Saito Y, Yamaguchi H, Saito D, Yokota T (1999) A new endoscopic mucosal resection procedure using an insulation-tipped electrosurgical knife for rectal flat lesions: report of two cases. Gastrointest Endosc 50:560–563
Ono H, Hasuike N, Inui T, Takizawa K, Ikehara H, Yamaguchi Y, Otake Y, Matsubayashi H (2008) Usefulness of a novel electrosurgical knife, the insulation-tipped diathermic knife-2, for endoscopic submucosal dissection of early gastric cancer. Gastric Cancer 11:47–52
Saito Y, Takisawa H, Suzuki H, Takizawa K, Yokoi C, Nonaka S, Matsuda T, Nakanishi Y, Kato K (2008) Endoscopic submucosal dissection of recurrent or residual superficial esophageal cancer after chemoradiotherapy. Gastrointest Endosc 67:355–359
Yamamoto H, Yahagi N, Oyama T, Gotoda T, Doi T, Hirasaki S, Shimoda T, Sugano K, Tajiri H, Takekoshi T, Saito D (2008) Usefulness and safety of 0.4% sodium hyaluronate solution as a submucosal fluid “cushion” in endoscopic resection for gastric neoplasms: a prospective multicenter trial. Gastrointest Endosc 67:830–839
Fujishiro M, Yahagi N, Kashimura K, Mizushima Y, Oka M, Enomoto S, Kakushima N, Kobayashi K, Hashimoto T, Iguchi M, Shimizu Y, Ichinose M, Omata M (2004) Comparison of various submucosal injection solutions for maintaining mucosal elevation during endoscopic mucosal resection. Endoscopy 36:579–583
Fujishiro M, Yahagi N, Kashimura K, Mizushima Y, Oka M, Matsuura T, Enomoto S, Kakushima N, Imagawa A, Kobayashi K, Hashimoto T, Iguchi M, Shimizu Y, Ichinose M, Omata M (2004) Different mixtures of sodium hyaluronate and their ability to create submucosal fluid cushions for endoscopic mucosal resection. Endoscopy 36:584–589
Parker SM, Gibson GJ (2007) Evaluation of a transcutaneous carbon dioxide monitor (“TOSCA”) in adult patients in routine respiratory practice. Respir Med 101:261–264
Maniscalco M, Zedda A, Faraone S, Carratu P, Sofia M (2008) Evaluation of a transcutaneous carbon dioxide monitor in severe obesity. Intensive Care Med 34:1340–1344
Carter BG, Wiwczaruk D, Hochmann M, Osborne A, Henning R (2001) Performance of transcutaneous PCO2 and pulse oximetry monitors in newborns and infants after cardiac surgery. Anaesth Intensive Care 29:260–265
Eberhard P, Gisiger PA, Gardaz JP, Spahn DR (2002) Combining transcutaneous blood gas measurement and pulse oximetry. Anesth Analg 94:76–80
Rohling R, Biro P (1999) Clinical investigation of a new combined pulse oximetry and carbon dioxide tension sensor in adult anaesthesia. J Clin Monit Comput 15:23–27
Sumanac K, Zealley I, Fox BM, Rawlinson J, Salena B, Marshall JK, Stevenson GW, Hunt RH (2002) Minimizing postcolonoscopy abdominal pain by using CO2 insufflation: a prospective, randomized, double blind, controlled trial evaluating a new commercially available CO2 delivery system. Gastrointest Endosc 56:190–194
Inoue H, Endo M, Takeshita K, Yoshino K, Muraoka Y, Yoneshima H (1992) A new simplified technique of endoscopic esophageal mucosal resection using a cap-fitted panendoscope (EMRC). Surg Endosc 6:264–265
Nelson DB, Freeman ML, Silvis SE, Cass OW, Yakshe PN, Vennes J, Stahnke LL, Herman M, Hodges J (2000) A randomized, controlled trial of transcutaneous carbon dioxide monitoring during ERCP. Gastrointest Endosc 51:288–295
Bell GD (2000) Premedication, preparation, and surveillance. Endoscopy 32:92–100
Bolliger D, Steiner LA, Kasper J, Aziz OA, Filipovic M, Seeberger MD (2007) The accuracy of noninvasive carbon dioxide monitoring: a clinical evaluation of two transcutaneous systems. Anaesthesia 62:394–399
Oda I, Gotoda T, Sasako M, Sano T, Katai H, Fukagawa T, Shimoda T, Emura F, Saito D (2008) Treatment strategy after noncurative endoscopic resection of early gastric cancer. Br J Surg 95:1495–1500
Imagawa A, Fujiki S, Kawahara Y, Matsushita H, Ota S, Tomoda T, Morito Y, Sakakihara I, Fujimoto T, Taira A, Tsugeno H, Kawano S, Yagi S, Takenaka R (2008) Satisfaction with bispectral index monitoring of propofol-mediated sedation during endoscopic submucosal dissection: a prospective, randomized study. Endoscopy 40:905–909
Lazzaroni M, Porro Bianchi (2005) Preparation, premedication, and surveillance. Endoscopy 37:101–109
Acknowledgments
We thank Mr. Christopher Dix for editing the manuscript. This study was partly supported by the Japanese Foundation for Research and Promotion of Endoscopy. Although the CO2 regulator prototype was provided by the Olympus Optical Co., Ltd., Tokyo, Japan, this was not a collaborative study.
Disclosures
Satoru Nonaka, Yutaka Saito, Hajime Takisawa, Yongmin Kim, Tsuyoshi Kikuchi, and Ichiro Oda have no conflict of interests or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nonaka, S., Saito, Y., Takisawa, H. et al. Safety of carbon dioxide insufflation for upper gastrointestinal tract endoscopic treatment of patients under deep sedation. Surg Endosc 24, 1638–1645 (2010). https://doi.org/10.1007/s00464-009-0824-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-009-0824-5