Abstract
This review describes the current state of knowledge about the ABCD family of peroxisomal half adenosine-triphosphate-binding cassette (ABC) transporters. ABCDs are predicted to be present in a variety of eukaryotic organisms, although at present, only ABCDs in the yeast Saccharomyces cerevisiae, the plant Arabidopsis thaliana, and different mammalian species have been identified and characterized to any significant extent. The functional role of none of these ABCDs has been established definitively and awaits successful reconstitution of ABCDs, either as homo- or heterodimers into liposomes, followed by transport studies. Data obtained in S. cerevisiae suggest that the two ABCDs, which have been identified in this organism, form a heterodimer, which actually transports acyl coenzyme A esters across the peroxisomal membrane. In mammals, four ABCDs have been identified, of which one [adrenoleukodystrophy protein (ALDP)] has been implicated in the transport of the coenzyme A esters of very-long-chain fatty acids. Mutations in the gene (ABCD1) encoding ALDP are the cause of a severe X-linked disease, called X-linked adrenoleukodystrophy. The availability of mutant mice in which Abcd1, Abcd2, or Abcd3 have been disrupted will help to resolve the true role of the peroxisomal half-ABC transporters.
Similar content being viewed by others
Introduction
Peroxisomes are ubiquitous subcellular organelles present in virtually all eukaryotic cells. They contain a variety of metabolic functions, some of which are specific for certain organisms, whereas others are common to all eukaryotes. In mammals, peroxisomes are essential for life, as exemplified by the devastating consequences of a defect in peroxisome biogenesis in human patients affected by Zellweger syndrome [93], whereas mice in which one of the genes involved in peroxisome biogenesis has been disrupted also show major abnormalities and a short life span [6, 11]. In contrast, peroxisomes in other species, including the yeast Saccharomyces cerevisiae, are only indispensable under selected growth conditions. Notably, peroxisome-deficient yeast cells are unable to grow on media with fatty acids (FAs) as sole carbon source but grow normally with glucose or glycerol.
One metabolic function of peroxisomes common to most, if not all, peroxisome-containing eukaryotic organisms, is the beta-oxidation of FAs. In higher eukaryotes, including humans, rats and mice, both mitochondria and peroxisomes are capable of FA beta-oxidation, whereas in lower eukaryotic organisms, including yeasts and plants, FA beta-oxidation is confined to peroxisomes. Available evidence indicates that at least some of the peroxisomal half adenosine-triphosphate (ATP)-binding cassette (ABC) transporters, as identified so far, play a role in FA beta-oxidation. For this reason we will first give some general information on peroxisomal FA beta-oxidation, with particular emphasis on human peroxisomes, which is then followed by a discussion of the characteristics of the various individual peroxisomal ABC transporters as identified in different eukaryotic organisms.
Fatty acid beta-oxidation in peroxisomes
Fatty acid beta-oxidation in peroxisomes proceeds in a similar way as FA beta-oxidation in mitochondria and involves a four-step mechanism in which acyl–coenzyme A (CoA) esters undergo dehydrogenation, hydration, another dehydrogenation, and thiolytic cleavage [44]. Although similar in mechanism, there are some major differences between the mitochondrial and peroxisomal beta-oxidation systems. For example, the two organelles catalyse the oxidation of different FA species, which has been most clearly established in peroxisomes of mouse and man. In particular, studies in patients afflicted by the genetic disease Zellweger syndrome, who lack peroxisomes, have been instrumental in this respect, and it is now clear that substrates, like (1) very-long-chain fatty acids (VLCFAs), (2) pristanic acid, (3) di- and trihydroxycholestanoic acid, and (4) tetracosahexaenoic acid (C24:6), are solely oxidized in peroxisomes and not in mitochondria, whereas long-chain and medium-chain FAs are predominantly oxidized in mitochondria, although peroxisomes may also contribute to long-chain FA beta-oxidation to some extent [94]. Furthermore, the enzymes involved in FA beta-oxidation in mitochondria and peroxisomes are different and the products of distinct genes, whereas the catalytic mechanisms of the different enzymes are actually very similar. A notable difference between the peroxisomal and mitochondrial systems concerns the first step, that is, the dehydrogenation of acyl–CoAs to trans-2-enoyl-CoAs, which is catalysed by different flavin adenine dinucleotide (FAD)-containing acyl–CoA dehydrogenases in mitochondria but by FAD-containing acyl–CoA oxidases in peroxisomes. In the case of the acyl–CoA oxidases, the FADH2 is reoxidized directly by molecular oxygen to produce hydrogen peroxide, whereas the FADH2 in acyl–CoA dehydrogenases is reoxidized via the mitochondrial electron transfer flavoprotein (ETF)–ETF dehydrogenase (ETFDH)–coenzyme Q system [15].
In S. cerevisiae, the four steps of beta-oxidation in peroxisomes are catalysed by one set of enzymes, including (1) an acyl–CoA oxidase (Fox1p), (2) a bifunctional protein with enoyl-CoA hydratase and D-3-hydroxyacyl-CoA dehydrogenase activity (Fox2p), and (3) a 3-oxoacyl-CoA thiolase (Fox3p) [44] (Fig. 1). In other yeasts, notably Yarrowia lipolytica [44], multiple enzymes are involved in each step of beta-oxidation. The same is true for plants, including Arabidopsis thaliana [29], and mammals. Remarkably, there are also differences between the beta-oxidation systems in humans vs rats and mice (see Ref. [95] for review). Indeed, in humans, there are only two acyl–CoA oxidases, two bifunctional enzymes, and two peroxisomal thiolases, whereas in rats and mice, there are three oxidases and at least three thiolases.
Schematic representation of the organisation of the peroxisomal beta-oxidation systems in the yeast S. cerevisiae and Homo sapiens showing the involvement of a single set of beta-oxidation enzymes in S. cerevisiae in contrast to H. sapiens. THC–CoA Trihydroxycholestanoyl–CoA; TMTD–CoA 4,8,12-trimethyl-tridecanoyl-CoA
The two human peroxisomal acyl–CoA oxidases have different substrate specificities: acyl–CoA oxidase 1 (ACOX1) is specific for the CoA esters of straight-chain FAs, whereas acyl–CoA oxidase 2 (ACOX2) is reactive with the CoA esters of both straight-chain and 2-methyl branched-chain FAs, including pristanoyl-CoA and di- and trihydroxycholestanoyl–CoA [90]. In human as well as in mouse and rat peroxisomes, the second and third steps of beta-oxidation are catalysed by two bifunctional proteins, both harbouring enoyl–CoA hydratase and 3–hydroxyacyl-CoA dehydrogenase activities. The two bifunctional proteins, however, do differ in their stereochemistry. Indeed, the L-bifunctional protein [alternative names: multifunctional protein 1 (MFP1), multifunctional enzyme I (MFEI), or L-peroxisomal bifunctional enzyme (L-PBE)] generates 3-ketoacyl-CoAs via an L-3-hydroxyacyl-CoA intermediate, whereas the D-bifunctional protein [alternative names: multifunctional protein 2 (MFP2), multifunctional enzyme II (MFEII), or D-peroxisomal bifunctional enzyme (D-PBE)] generates a D-3-hydroxyacyl-CoA intermediate. The two human peroxisomal thiolases comprise (1) peroxisomal 3-ketoacyl-CoA thiolase 2, better known as sterol carrier protein X (SCPX), which catalyses the thiolytic cleavage of the 3-ketoacyl-CoA esters of both straight-chain and branched-chain FAs, and (2) peroxisomal 3-ketoacyl-CoA thiolase 1 (pTH1), which resembles the clofibrate-inducible thiolase identified by Miyazawa and co-workers [56] and is only reactive with the 3-ketoacyl-CoA esters of straight-chain FAs [3]. The importance of the different enzymes in human peroxisomal FA beta-oxidation is emphasized by the existence of patients with a genetic deficiency at the level of acyl–CoA oxidase 1 [66], D-bifunctional protein [17], and SCPX [18]. In addition, studies with mice in which either the gene encoding acyl–CoA oxidase 1 [16], L-bifunctional protein [71], D-bifunctional protein [5], or SCPX [75] has been disrupted have also contributed greatly to the current knowledge about the involvement of the different enzymes in the beta-oxidation of the various substrates.
Other differences between the mitochondrial and peroxisomal systems follow logically from the fact that peroxisomes lack a respiratory chain and a citric acid cycle, which implies that the reducing equivalents, generated in the first (FADH2) and third [nicotinamide adenine dinucleotide (reduced form; NADH)] step of beta-oxidation, cannot be reoxidized by these systems. In case of the FADH2 generated in the first step, this is solved by the direct reoxidation of the acyl–CoA-oxidase-bound FADH2 to FAD by molecular oxygen, which generates hydrogen peroxide (H2O2). Peroxisomal catalase reconverts the H2O2 thus generated back into O2. The NADH produced at the third step of beta-oxidation is transferred to mitochondria via different redox shuttles, including a malate dehydrogenase-based NADH shuttle in yeast [88], whereas in higher eukaryotes, a lactate dehydrogenase-based NADH redox shuttle has been proposed [7]. With respect to the other end products of peroxisomal beta-oxidation, that is, acetyl–CoA and other chain-shortened acyl–CoAs, current evidence holds that transfer of these CoA esters to mitochondria may proceed via two different mechanisms. The first involves conversion of an acyl–CoA species into the corresponding acylcarnitine via one of the two peroxisomal carnitine acyltransferases, including carnitine acetyltransferase (CAT) and carnitine octanoyltransferase (COT), followed by export from the peroxisome to the cytosol via an unknown mechanism and uptake into mitochondria via the mitochondrial carnitine/acylcarnitine transporter (CACT). After retroconversion of the acylcarnitine species back into the corresponding acyl–CoA, degradation to CO2 and H2O occurs. In the other mechanism, acyl–CoA species are hydrolyzed by one of the different acyl–CoA thioesterases identified in peroxisomes, followed by export of the free FA to the cytosol and uptake into mitochondria. Inside mitochondria, activation to the corresponding CoA ester may occur, followed by beta-oxidation. FAs originating from peroxisomes may also leak out of the cell and into the plasma compartment and finally into the urine, as, for instance, is the case for certain dicarboxylic acids.
Peroxisomal ABC transporters
ABC transporters constitute one of the largest families of proteins, with 48 members identified so far in humans, and are integral membrane proteins catalysing the transport of a variety of substrates ranging from ions to proteins. Structurally, ABC transporters may occur either as full transporters or half transporters. Most eukaryotic ABC transporters are full transporters composed of two homologous halves, with each half made up of a hydrophobic transmembrane domain containing multiple alpha helices, and a hydrophilic nucleotide-binding fold (NBF) with Walker A and B consensus motifs. Half-ABC transporters only have single hydrophobic and hydrophilic domains and are only functional after dimerization either as homo- or heterodimers. All peroxisomal ABC transporters are half-transporters and belong to subclass D of the ABC protein family.
Yeast peroxisomal ABC transporters
Saccharomyces cerevisiae contains two peroxisomal half-ABC transporters named Pxa1p (peroxisomal ABC transporter1 protein) and Pxa2p. Alternative names used in literature are Pat2p [33] and Pal1 [85] for Pxa1p, and Pat1p [33] for Pxa2p. The PXA1 gene was first identified by Shani et al. [77] using RNA from oleate-induced S. cerevisiae as template and degenerate primers corresponding to the Walker A and B motifs of the ATP-binding domains of the mammalian peroxisomal half-ABC transporters known at that time, that is, adrenoleukodystrophy protein (ALDP) [59] and peroxisomal membrane protein (PMP)70 [39]. The Pxa1p protein was most similar to human ALDP, human PMP70, and the product of another yeast gene, YKL741, already identified earlier by the yeast genome sequencing project [9]. Disruption of PXA1 resulted in impaired growth on oleate-containing medium and a reduced ability to oxidize oleate. Disruption of YKL741 gave a growth phenotype identical to that of the PXA1 mutant. The double knockout also had the same phenotype. The non-additive effect of disruption of both PXA1 and YKL741 led Shani et al. [77] to suggest that their protein products (Pxa1p and Ykl401p) may be subunits of one and the same transporter. Subsequent studies by different groups [33, 76, 85] showed that Pxa1p and Pxa2p are integral PMPs, which heterodimerize to form a complete peroxisomal ABC transporter. The finding that oxidation of long-chain FAs, like oleate and palmitate, was deficient in whole cells but not in homogenates of the pxa1Δ and pxa2Δ cells suggested that the Pxa1p/Pxa2p couple is involved in transmembrane transport of FAs, most likely in their CoA ester form [33].
Interestingly, the single mutants (pxa1Δ and pxa2Δ) and the double mutant (pxa1Δ, pxa2Δ) exhibited normal growth on laurate (C12:0)- and myristate (C14:0)-containing medium and oxidized these substrates at near-normal rates (Fig. 2). These data provided suggestive evidence in favour of a model in which FAs can reach the peroxisomal matrix via two independent pathways, one taken by LCFAs and the other by medium-chain fatty acids (MCFAs).
Fatty acid oxidation in wild-type S. cerevisiae and different mutants, including pxa1Δ, pxa2Δ, pxa1Δ/pxa2Δ, faa2Δ, pxa2Δ/faa2Δ, and pxa1Δ/faa2Δ. Cells were grown on oleate-containing medium, incubated with different [1-14C] fatty acids, and beta-oxidation-measured as described in Hettema et al. [33]. Data taken from Hettema et al. [33]
It has been firmly established that LCFAs (but not MCFAs) are activated outside peroxisomes by one of the acyl–CoA synthetases [37] and are then transported into the peroxisomal matrix by the Pxa1p/Pxa2p heterodimer. On the other hand, MCFAs appear to traverse the peroxisomal membrane in their free acid form, either mediated by Pex11p [89] or not [48], after which activation occurs by the medium-chain acyl–CoA synthetase Faa2p, localized within peroxisomes, followed by beta-oxidation. Strong evidence in favour of this model (see Fig. 3a) came from experiments by Hettema et al. [33], who reasoned that the site of activation actually determines which of the two routes is taken. This conclusion was confirmed in experiments using a mutant in which Faa2p was mislocalized to the cytosol. This mutant was able to oxidize all FAs. Importantly, double mutants with Faa2p mislocalized to the cytosol, and either PXA1 and/or PXA2 deleted, failed to grow on both MCFAs and LCFAs. This implies that when MCFAs undergo activation in the cytosol as in the mutant with Faa2p mislocalized to the cytosol, oxidation of MCFAs is dependent on the Pxa1p/Pxa2p heterodimer. These data fully support the model depicted in Fig. 3a.
Models depicting a the oxidation of MCFA and LCFA in peroxisomes in S. cerevisiae and the role of Faa2p and Pxa1p/Pxa2p therein and b the oxidation of VLCFAs in peroxisomes in human cells and the role of ALDP therein either as homodimer or heterodimer with ALDR, PMP70, and PMP69 as potential partners
Mutagenesis studies focused on the excitatory amino acid (EAA) motif, a conserved motif of approximately 30 residues between transmembrane domains 4 and 5 (TM4 and TM5), and the loop 1 motif, localized between TM1 and TM2, have shown that substitution of the conserved amino acid glutamine at position 294 (E294D) and glutamate at position 301 (G301A) is associated with a full loss of activity [78].
Mammalian peroxisomal ABC transporters
So far, four ABC transporters have been detected in mammalian peroxisomes. The first peroxisomal ABC transporter was identified by Kamijo et al. [38]. The protein involved, named PMP70, encoded by the ABCD3 gene, is one of the major integral membrane proteins of peroxisomes, known to be markedly induced by the administration of hypolipidaemic agents, including di(2-ethyl)hexylphthalate (DEHP), at least in rodents. The PMP70 cDNA was isolated by expression cloning using cDNA prepared from the liver of a rat treated with DEHP. The cDNA coded for a protein of 659 amino acids of which the carboxy-terminal region showed strong sequence similarity to the group of ABC transporters withWalker A (AA473-486) and Walker B (AA583-596) motifs. Hydropathy analysis revealed that the amino-terminal half of PMP70 is hydrophobic with six predicted transmembrane segments. Protease treatment of peroxisomes indicated that the ATP-binding domain of PMP70 is exposed to the cytosol. The human PMP70 was soon identified by the same group [39] and, independently, by Gärtner and Valle [26], and has 99.1 and 95.0% sequence similarity and identity, respectively, with the rat PMP70.
The second mammalian ABC transporter, named ALDP, encoded by ABCD1 was identified in 1993 by Mosser et al. [59] using a positional cloning strategy. As discussed in more detail below, mutations in ABCD1 cause X-linked adrenoleukodystrophy (X-ALD). Topology studies have shown that the hydrophilic carboxy-terminal half containing the ATP-binding domains is on the cytoplasmic face of the peroxisomal membrane [14]. Shortly thereafter, Lombard-Platet and coworkers [50] identified the third peroxisomal half ABC transporter named ALDR (adrenoleukodystrophy-related protein) encoded by ABCD3 because of its marked homology with ALDP (63% amino acid identity). Corresponding homologies in the rat [2] and mouse [74] have also been identified.
Finally, a fourth peroxisomal half ABC transporter named PMP69 or, alternatively, PMP70R, encoded by ABCD4, was identified by two groups at the same time [34, 79]. Human PMP69 has weak sequence homology with the other peroxisomal half ABC transporters, with amino acid identities of 28.4 and 25.2% with PMP70 and ALDP, respectively.
Homo- or heteromerization of the peroxisomal half ABC transporters
It is still unclear whether the different half ABC transporters actually form homo- or hetero(di)mers. A first study by Liu and co-workers [49] suggested that both homo- and heterodimerization may occur. It should be noted, however, that this conclusion is based on two-hybrid experiments in which for experimental reasons, only the carboxy-terminal hydrophilic halves of ALDP, ALDR, and PMP70 were used. In addition, Liu and co-workers [49] also performed co-immunoprecipitation studies, which indicated homodimerization of ALDP, heterodimerization of ALDP with PMP70 or ALDRP, and heterodimerization of ALDRP with PMP70. A similar conclusion was reached by Smith and co-workers [84], who used a combined strategy of co-immunoprecipitation and in vitro synthesis to identify protein interactions between ALDP, PMP70, and ALDR. In a third study by Tanaka and co-workers [86], in which use was made of purified rat liver peroxisomes, co-immunoprecipitation of ALDP with PMP70 was found. Using a different approach, based on the use of the mild detergent digitonin, Guimaraes and co-workers [30] arrived at the completely opposite conclusion, suggesting that both ALDP and PMP70 are present in the peroxisomal membrane predominantly as homomers, probably dimers. Kashiwayama and co-workers [40] have also provided evidence in favour of PMP70 primarily being present as a homodimer. Furthermore, these authors concluded that PMP70 undergoes conformational changes upon binding and hydrolysis of ATP. Both PMP70 and ALDP are also subject to tyrosine phosphorylation [86].
Expression of the four mammalian ABC transporters
In Table 1, the relative mRNA expression levels of the four ABCDs in different mouse and human tissues as taken from the work of Berger et al. [8] and Langmann et al. [46], respectively, are depicted. The data show that, in general, the expression profiles of the four ABCDs and their levels are similar between mouse and man. ABCD1 mRNA was most abundant in the heart, testis, lung, and intestine, whereas ABCD2 (ALDR) mRNA was enriched in the brain and skeletal muscle. ABCD3 (PMP70) mRNA was highest in the liver and kidney, whereas ABCD4 (PMP69) mRNA was highest in the lung and testis, followed by the kidney, at least in human tissues.
Studies by Troffer-Charlier et al. [87] showed that the expression levels of the peroxisomal ABCDs may vary widely between different cell types within the same organ, at least in the case of ABCD1 (ALDP) and ABCD2 (ALDR), and that there is not always a strict correlation between mRNA and protein levels. In mouse brain, ABCD2 (ALDR) mRNA expression was highest in the cerebral cortex and in the pyramidal and granular cell layers of the dentate gyrus of the hippocampus. In the cerebellum, ABCD2 (ALDR) mRNA expression was detected in Purkinje cells and cells of the inner granular layer. In contrast, the expression of ABCD1 (ALDP) mRNA was more homogeneously distributed between the cerebral cortex and the white matter. In the cerebellum, expression of ABCD1 (ALDP) mRNA was found in the white matter but not in Purkinje and granular cells. Marked expression of ABCD1 (ALDP) mRNA in cerebellar white matter contrasted with a weak signal of ABCD2 (ALDR) mRNA in this area. These results suggest a predominant neuronal expression of ABCD2 (ALDR) mRNA and a predominantly global cell expression of ABCD1 (ALDP) mRNA.
In addition to mRNA expression studies, Troffer-Charlier et al. [87] also performed immunohistochemical studies. These studies revealed that within the brain, virtually no ALDP can be detected in neurons of the cerebral cortex, hippocampus, Purkinje, and granular cells (Table 2). In contrast, ALDP immunoreactivity was detectable in astrocytes of cerebellum (Bergmann glia and white matter astrocytes) and cerebral white matter, and in protoplasmic astrocytes of cerebral cortex. Marked expression of ALDP was also found in microglia labelled with a Mac-1 antibody, endothelial cells, and choroid plexus. Remarkably, only a subset of oligodendrocytes localized in the white matter of the cerebral hemispheres and cerebellum showed ALDP immunoreactivity. Based on these findings, which indicated that ALDP and ALDR have strikingly different expression profiles in most mouse tissues (as well as in different human cell lines, as studied in the same paper), Troffer-Charlier et al. [87] concluded that ALDP and ALDR are unlikely to function as obligatory partners in a ALDP/ALDR heterodimer, but may rather fulfil similar functions in different cells. This is concluded from the fact that certain cells (neurons, adrenocortical and chromaffin cells, endothelial cells, and fibroblasts) may express one type of protein, but not the other (Table 2). It should be pointed out that the similar absence of coordinated expression was previously demonstrated for PMP70 and ALDP [67].
Inducibility of the expression of the four mammalian ABCDs
The expression of the different mammalian ABCDs differs wildly, not only from tissue to tissue, but also within a certain tissue. Furthermore, the expression of the different mammalian ABCDs can vary depending upon the feeding conditions. Indeed, early studies already showed that the expression of PMP70 is markedly induced by peroxisome proliferators, including fibrates, such as ciprofibrate [13], fenofibrate [1, 23], and plasticizers such as di(2-ethylhexyl)phthalate [38]. Albet et al. [1] have shown that, at least in mice, fibrates have a differential effect on the expression of the Abcd1, Abcd2, and Abcd3 genes, with (1) virtually no effect on Abcd1 mRNA, (2) induced expression of Abcd2 mRNA, especially in the liver (>tenfold), and (3) induced expression of Abcd3 mRNA, notably in the liver and even more so in the intestine. Similar results were obtained by Netik et al. [60] for Abcd2 and Abcd3 expression. Table 2 summarizes these data.
To determine whether the fenofibrate-induced expression of the Abcd2 (Aldr) and Abcd3 (Pmp70) genes is PPARalpha-dependent, Fourcade et al. [23] performed experiments in the PPARalpha (−/−) mouse, which clearly showed marked induction of both Abcd2 and Abcd3 mRNA in the wild type (+/+) but not in the (−/−) mouse. Promoter analysis revealed the presence of several candidate PPAR response elements (PPREs), but subsequent studies, which included electrophoretic mobility shift assay (EMSA) analysis, indicated that none of the candidate PPREs is actually functional. This led Fourcade et al. [23] to conclude that the fibrate-induced expression of Abcd2, at least in the rat, is indirect and does not follow the classical pathway in which the PPARalpha/retinoid X receptor (RXR)-dimer binds to a specific consensus sequence (-AGGTCA(A) AGGTCA-) called PPRE. It should be noted that the human ABCD3 (PMP70) promoter also lacks an apparent PPRE [28]. In recent years, many examples of genes have been identified, the expression of which is induced by fibrates, but which lack such a PPRE [52]. One example is pyruvate dehydrogenase kinase 4 (PDK4). Recent studies by Wende and co-workers [98] have shown that the estrogen-related receptor (ERR) plays a key role in the induction of PDK4 by fibrates. Additional studies will be needed to show whether the ERR-mediated pathway also controls the expression of other known fibrate-induced genes.
Rampler et al. [72] performed similar promoter studies as performed by Fourcade et al. [23] in the mouse. These authors identified four putative PPREs in the mouse Abcd2 promoter, which all turned out to be non-functional. In search of the possible mechanism behind the PPRE-independent induction of Abcd2 expression, Rampler et al. [72] identified a sterol regulatory element (SRE), which led to the suggestion that the effect of PPARalpha may be mediated via the SRE binding protein (SREBP) pathway. Interestingly, SREBP2 mRNA levels were markedly induced by fenofibrate in the wild-type (+/+) mice, but not in the PPARalpha (−/−) mice, whereas SREBP1c expression was downregulated by fenofibrate in a PPARalpha-independent way. These data suggested that the PPARalpha agonist mediated induction of Abcd2 expression may occur via an SREBP2-dependent mechanism. Studies by Weinhofer et al. [96] clearly established that the Abcd2 promoter indeed contains a functional SRE. The presence of the SRE also explains why the expression of human ABCD2 is induced by lowering cholesterol, such as by growing fibroblasts in a sterol-depleted medium. Earlier studies already showed that the expression of both the human (ABCD2) and mouse (Abcd2) genes is also controlled by thyroid hormone. Indeed, Fourcade et al. [24] identified a thyroid response element (TRE) representing a direct repeat hexameric sequence of the DR-4 type capable of binding a RXR/thyroid hormone receptor (TR)β-heterodimer, which mediates the T3 response of the ABCD2 gene. Interestingly, the SRE and DR-4 motifs of both the human and murine ABCD2 and Abcd2 promoters overlap. Recent studies by Weinhofer et al. [97] showed that the regulation of the ABCD2 gene is even more complicated as originally believed and involves different players, including LXR, RXR, TR, and SREBP.
One puzzling finding has been the lack of response in the brain by fenofibrate and other PPARalpha ligands. Berger et al. [8] postulated that this is due to the fact that fenofibrate is actually removed from the brain by the multidrug transporter P-glycoprotein, localized at the blood–brain barrier. To test this hypothesis P-glycoprotein-deficient mice [Mdr1a (−/−) mice] were treated with fenofibrate, followed by mRNA analysis from brain and liver tissue. Northern blotting demonstrated that in contrast to wild-type mice, Abcd2 (Aldr) gene expression was increased by fenofibrate, also in the brain from the Mdr1a (−/−) mice, strongly supporting the notion that fenofibrate is a substrate for the multidrug transporter P-glycoprotein and is actively removed from the brain compartment.
Functional role of the mammalian ABCDs
ABCD1 (ALDP)
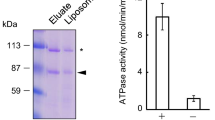
The functional role of none of the mammalian ABCDs has been established with certainty. Based on their studies in S. cerevisiae, Hettema et al. [33] suggested that the Pxa1p/Pxa2p heterodimer transports acyl–CoA esters. This possibility was directly tested by Verleur et al. [91] in S. cerevisiae cells permeabilized with digitonin. In this system, uptake of oleyl–CoA, although measured indirectly, was both ATP- and Pxa1p- and/or Pxa2p-dependent, indicating that the Pxa1p Pxa2p couple is indeed involved in acyl–CoA uptake. Based on these data, it has been proposed that ALDP, which is more similar to Pxa1p and Pxa2p than to any other yeast transporter, is involved in the uptake of activated VLCFAs into mammalian peroxisomes either as homo- or heterodimer (Fig. 3b).
In the absence of conclusive evidence for a role of Pxa1p and Pxa2p as well as ALDP as transporters of acyl–CoA esters, alternative explanations have been forwarded. McGuinness and co-workers [55] have suggested that the accumulation of VLCFAs in X-ALD patients and Abcd1(−/−) mice is secondary to mitochondrial abnormalities, knowing that the peroxisomal beta-oxidation system requires properly functioning mitochondria for (1) reoxidation of the NADH generated in peroxisomes and (2) final oxidation of the end products of peroxisomal beta-oxidation. Although some evidence for this postulate has been brought forward, recent work from Oezen et al. [62] has failed to identify mitochondrial abnormalities in the Abcd1 (−/−) mouse, which argues against this hypothesis.
Yamada et al. [99] suggested that ALDP is required for correct targeting of the activating enzyme very-long-chain acyl–CoA synthetase (VLACS) to peroxisomes. Apart from the fact that the reduction in the amount of Vlacs protein in peroxisomes isolated from livers of Abcd1 (−/−) mice was only minimal (30% reduction), it is now known that VLACS plays no role in VLCFA activation nor beta-oxidation. This is concluded from the fact that Vlacs (−/−) mice do not show any VLCFA abnormality [32]. Furthermore, available evidence shows that VLCFAs are activated outside peroxisomes by one of the long-chain acyl–CoA synthetases of the ACSL family [53] and/or one of the VLACS of the ACSVL/FATP family [65]. In this respect it is important to mention that peroxisomes contain abundant VLCFA–CoA synthetase activity of which the bulk (>95%) is exposed to the cytosol [45]. Which synthetase actually is responsible for this activity is unknown at present. A good candidate would be acyl–CoA synthetase 4, which is a peripheral-membrane protein located in two distinct subcellular organelles, including peroxisomes and mitochondria-associated membrane (MAM) [47].
ABCD2 (ALDRP)
Overexpression of ABCD2 in human ABCD1 (−/−) cells and mouse Abcd1 (−/−) cells is associated with the increased oxidation of C24:0 and C26:0 [20, 41, 60] and normalisation of VLCFA levels [41]. These data suggest that ALDP and ALDR exhibit overlapping substrate specificities, which implies that if ALDP transports VLCFA–CoAs, ALDR can do the same, although with a much reduced catalytic efficiency, as concluded from the marked overexpression needed to achieve correction. Interestingly, ALDR can also compensate for the loss of ALDP under in vivo conditions, as shown by Pujol and co-workers [70]. Conversely, Abcd2 (−/−) mice show no abnormalities in VLCFA metabolism, indicating that ALDP and not ALDR is the key player in VLCFA metabolism, which leaves the true physiological function of ALDR unresolved.
ABCD3 (PMP70)
It was originally thought that PMP70, at least in humans, would play a key role in peroxisome biogenesis. This was concluded from the finding of mutations in the PMP70 gene in a patient affect by Zellweger syndrome belonging to complementation group 1 [27]. Later studies, however, revealed that PEX1 is the gene mutated in complementation group 1 and not PMP70. To study the role of PMP70, Imanaka et al. [35] transfected the cDNA of rat Abcd3 (Pmp70) into Chinese hamster ovary (CHO) cells and, thus, established cell lines stably overexpressing PMP70. The overexpressed Pmp70 (five- to tenfold) was correctly targeted to peroxisomes. Fatty acid oxidation measurements in intact cells revealed that oxidation of C16:0 is induced two- to threefold, whereas oxidation of C24:0 was actually reduced by 50%. CHO cells stably overexpressing mutant Pmp70s exhibited reduced oxidation of C16:0 in intact cells. One of the mutants included in these studies involved a mutant in which the lysine at position 479 within the Walker A motif was mutated into an alanine. A second mutant contained a Pmp70 lacking the carboxy-terminal 84 amino acids, thus showing that the C terminus is essential for activity of PMP70. Based on these results Imanaka et al. [35] concluded that PMP70 is transporting long-chain acyl–CoAs (LCFA–CoAs) across the peroxisomal membrane. Whether this is also the true physiological role of PMP70 under in vivo conditions remains to be established. Characterization of the recently generated Pmp70 (−/−) mice may help in this respect [36].
ABCD4 (PMP69)
There is no information in literature regarding the physiological role of this peroxisomal half-ABC transporter. No Pmp69 (−/−) mouse model has been described so far.
Human ABCDs and disease
So far only a single disease has been attributed to one of the ABCDs. The disease involved is X-ALD, which is due to mutations in the ABCD1 gene. At present at least six phenotypic variants have been distinguished. The classification of different phenotypes of X-ALD is somewhat arbitrary and is based upon the age of onset and the organs principally affected. Childhood cerebral ALD (CCALD) and adrenomyeloneuropathy (AMN) are the two most frequent phenotypes, together accounting for more than 80% of all cases. CCALD is characterized by rapidly progressive cerebral demyelination. The onset is between 3 and 10 years of age. Frequent early neurologic symptoms are behavioural disturbances, a decline in school performance, deterioration of vision, and impaired auditory discrimination. The course is relentlessly progressive, and seizures, spastic tetraplegia, and dementia develop within months. Most patients die within 2 to 3 years after the onset of neurological symptoms. Adrenomyeloneuropathy is much less severe as compared with CCALD. The onset of neurological symptoms in this phenotype usually occurs in the third and fourth decade. Neurologic deficits are primarily due to the myelopathy and, to a lesser extent, to neuropathy. Patients gradually develop a spastic paraparesis, often in combination with disturbed vibration sense in the legs, and sphincter dysfunction. Approximately 50% of AMN patients show mild to moderate cerebral involvement on magnetic resonance (MR) imaging, and in some, the white matter abnormalities may resemble the demyelisation seen in CCALD. The spinal cord frequently is atrophic [4, 57].
X-ALD is characterized biochemically by elevated plasma and tissue levels of saturated straight-chain VLCFAs, notably C24:0 and C26:0, although monounsaturated VLCFAs, including C26:1, are also elevated. The elevated levels of VLCFAs are the result of the reduced oxidation of VLCFAs in peroxisomes. Based on the finding that the actual peroxisomal beta-oxidation machinery required for the oxidation of C26:0-CoA is completely normal in X-ALD patients, it has been suggested that ALDP is responsible for the transport of VLCFAs across the peroxisomal membrane, probably in their activated CoA bound form.
X-ALD is caused by mutations in the ABCD1 gene. As of April 2006, the X-ALD mutation database (http://www.x-ald.nl/) contains 866 mutations which have been identified by various groups around the world (for mutation references, see http://www.x-ald.nl/references.htm). Of the 866 mutations, 526 (61%) are missense mutations, 196 (23%) are frame shifts, 84 (10%) are nonsense mutations, 32 (4%) are amino acid insertions or deletions, and 28 (4%) are large deletions of one or more exons. The majority of X-ALD kindreds have a unique mutation. Four hundred and thirty-five (50%) non-recurrent mutations have been identified.
The biochemical defect in X-ALD
As described above, oxidation of VLCFAs, notably C24:0 and C26:0, is deficient in fibroblasts from X-ALD patient. Indeed, incubation of intact X-ALD fibroblasts with radio-labelled C26:0 revealed decreased production of both [14C] C02 and radio-labelled acid-soluble products (acetate, Krebs cycle intermediates, etc.), whereas oxidation of radiolabeled palmitate, known to be oxidized predominantly (>95%) via the mitochondrial beta-oxidation system, was fully normal in X-ALD cells. Recent results by Kemp et al. [42] have shown the same with deuterated C24:0 as substrate. These results, first reported by Singh et al. [81], suggested that the accumulation of VLCFAs in X-ALD patients is directly explained by the depressed oxidation of C26:0 in peroxisomes in X-ALD cells. Studies, notably by McGuinness and co-workers [55] have challenged this conclusion. The basis for this different view comes from experiments by McGuinness et al. [55], who determined the rates of C24:0 beta-oxidation in different tissues, including brain, adrenal, heart, liver, kidney, and fibroblasts, and also determined the VLCFA levels, notably the C26:0/C22:0 ratio. Whereas the C26:0/C22:0 ratio was clearly elevated in all tissues examined except the liver, C24:0 beta-oxidation was fully normal in all tissues studied except fibroblasts. These findings led McGuinness et al. [55] to conclude that the elevated levels of VLCFAs in X-ALD are not a consequence of impaired peroxisomal degradation of VLCFAs, and that ALDP plays no role in peroxisomal VLCFA beta-oxidation. Based on data described in the same paper, which showed that oxidation of C24:0 is (mildly) deficient in fibroblasts from patients with a defect in mitochondrial beta-oxidation at the level of carntine palmitoyltransferase 1 (CPT1) and very-long-chain dehydrogenase (VLCAD), the authors concluded that the reduced oxidation of C24:0 in X-ALD cells is due to the mitochondrial abnormalities in X-ALD, and that ALDP facilitates the interaction between peroxisomes and mitochondria. Subsequent studies, however, notably by Oezen et al. [62], have shown that mitochondria isolated from Abcd1 (−/−) mice are indistinguishable from wild-type mitochondria in all aspects studied, which includes normal rates of oxidative phosphorylation and normal P/O ratios.
It should be noted that the FA oxidation measurements by McGuinness et al. [55] have not been done with intact cells but with broken cell preparations, including total homogenates, post-nuclear supernatants, and peroxisomal fractions. Because peroxisomes are well known to be extremely fragile with loss of membrane integrity upon tissue homogenisation, it is doubtful whether beta-oxidation measurements in such preparations are a true reflection of the situation in intact cells. To resolve this important issue the experiments of McGuinness et al. [55] need to be repeated to compare homogenates with intact cell preparations.
Correction of the biochemical defect in X-ALD by overexpression of ALDR and PMP70 and by other means
Ever since the discovery that VLCFAs accumulate in tissues and plasma from X-ALD patients, efforts have been undertaken to correct the defect by different manipulations. One of the first successful efforts to correct the accumulation of VLCFAs in X-ALD fibroblasts was performed by Rizzo et al. [73], who found that addition of monounsaturated FAs, like oleic acid and erucic acid, led to a full normalisation of VLCFA levels and X-ALD fibroblasts, possibly due to the inhibition of chain elongation of LCFAs to VLCFAs. In fact, this observation was the basis for starting a dietary therapy in X-ALD patients called Lorenzo’s oil therapy. Other efforts include:
-
1.
Overexpression of PMP70 and ALDR. As first shown by Braiterman et al. [10], the defect in C24:0 beta-oxidation in X-ALD cells can be corrected by overexpression of PMP70. This was soon followed by the finding that overexpression of ALDR can also restore C24:0 beta-oxidation. This led to the conclusion that ALDP, ALDR, and PMP70 exhibit overlapping substrate specificities, which each half transporter having its own preferred substrate, which are the VLCFAs for ALDP. As described above, Pujol et al. [70] found that ALDR can also compensate for the loss of ALDP under in vivo conditions in the Abcd1 (−/−) mice. These important findings suggest that a therapy based on the pharmacological induction of ABCD2 in X-ALD patients may well be conceivable.
-
2.
Forskolin, rolipram, and 8-bromo-cyclic adenosine monophosphate. Pahan et al. [63] have shown that compounds, like forskolin, 8-bromo-cyclic adenosine monophosphate (cAMP), and rolipram, which all induce an increase in intracellular cAMP levels, stimulate C24:0 beta-oxidation and normalize VLCFA levels in X-ALD cells. On the other hand, compounds like H-89 and myristoylated PKA that decrease cAMP levels and PKA activity inhibit the peroxisomal beta-oxidation of C24:0. The mechanism behind these effects has remained obscure, although studies by Pujol et al. [68] suggested that forskolin may have a direct effect on ABCD2 expression. Unfortunately, the data of Pahan et al. [63] could not be duplicated in another study performed by Netik et al. [61]. Furthermore, rolipram did not normalize VLCFA levels in the Abcd1 (−/−) mouse [61].
-
3.
Statins, cholesterol-lowering, and C24:0 beta-oxidation. Singh et al. [83] have reported that C24:0 beta-oxidation in X-ALD fibroblasts is restored in the presence of lovastatin and sodium phenylacetate. Lovastatin and phenylacetate are inhibitors of human menopausal gonadotropin (HMG)–CoA reductase and mevalonate pyrophosphate decarboxylase, respectively, and inhibit de novo cholesterol biosynthesis. Subsequent studies by Weinhofer et al. [96] showed that growth of X-ALD fibroblasts in cholesterol-depleted medium also restored C24:0 beta-oxidation, which may be due to the increased expression of ABCD2 via the SREBP system. Unfortunately, statins do not normalize VLCFAs in the Abcd (−/−) mouse [12, 100]. Studies in human X-ALD patients have shown conflicting results [64, 82, 92].
-
4.
4-Phenylbutyrate. Kemp et al. [41] showed that 4-phenylbutyrate was able to restore oxidation of C24:0 in X-ALD fibroblasts and restored VLCFA levels to normal. 4-PBA treatment of X-ALD cells resulted in the induced expression of ABCD2 and peroxisome proliferation both in fibroblasts from X-ALD patients and in Abcd1 (−/−) mouse fibroblasts. These results suggested that the effect of 4-PBA might be mediated via ABCD2. Subsequent experiments led McGuinness et al. [54] to conclude that 4-PBA exerts its effect via an ABCD2-independent mechanism [54], which may well involve mitochondria because 4-PBA also had a marked stimulatory effect on mitochondrial beta-oxidation. Importantly, 4-PBA was able to normalize VLCFA levels in the brain and adrenal gland of the Abcd1 (−/−) mouse. These results formed the basis for a small clinical trial involving seven AMN patients in which no effect was observed on the VLCFA levels in plasma from patients [58].
-
5.
Fibrates. Dietary supplementation of PPAR agonists, like fenofibrate, a hypolipidaemic drug used to treat hypertriglyceridaemia patients, to mice and rats gives rise to a marked induction of Abcd2 and Abcd3 expression with increased Aldr and Pmp70 protein levels. Interestingly, there was a partial correction of C24:0 beta-oxidation capacity in the liver of Abcd1 (−/−) mice by fenofibrate [60]. No studies have been published in which the effect of fenofibrate was studied on VLCFA levels in different mouse tissues.
Mouse models
Mutant mice have been reported with Abcd1, Abcd2, and Abcd3 disrupted. Abcd1 (−/−) mice have been generated through homologous recombination by three different groups [22, 43, 51]. Forss-Petter et al. [22] and Kobayashi et al. [43] targeted the neocassette to exon 1, whereas exon 2 was targeted in the mouse generated by Lu et al. [51]. Inactivation of the murine Abcd1 gene did not lead to a detectable phenotype up to 6 months despite the accumulation of VLCFAs in tissues, similar to that observed in X-ALD patients. Studies by Pujol et al. [69], in which the mouse generated by Lu et al. [51] was switched from a pure 129Sv background to a mixed 129Sv/C57BL/6J background, showed that older mice exhibited an abnormal neurological and behavioural phenotype starting at around 15 months of age. Knockout mice showed a slower nerve conduction with abnormal myelin and axonal loss in both the spinal cord and sciatic nerve. Axonal damage occurs as a first pathological event in Abcd1 (−/−) mice followed by myelin degeneration. Taken together, the late-onset progressive neurogenerative phenotype of Abcd1 (−/−) mice mimics the phenotype of AMN but not CCALD.
To study whether overexpression of ABCD2, known to be able to correct the defect in X-ALD fibroblasts, is also able to accomplish this in vivo, Pujol et al. [70] achieved overexpression of the Abcd2 gene by means of the strong chicken beta-actin promoter in the Abcd1 (−/−) mouse. Overexpression of ALDR in mice lacking ALDP was found to prevent both the accumulation of VLCFAs and the neurogenerative features. On the other hand, double mutants, in which both Abcd1 and Abcd2 were disrupted, were found to exhibit an earlier onset and more severe disease, including signs of an inflammatory reaction when compared with the single mutants. Taken together, these results provide direct evidence for functional redundancy between ALDP and ALDR under in vivo conditions and highlight ALDR as a therapeutic target for treatment of X-ALD.
Ferrer and co-workers [19] have also generated Abcd2 (−/−) mice. These mice show a late-onset cerebellar and sensory ataxia with loss of cerebellar Purkinje cells and dorsal root ganglia cell degeneration, correlating with the accumulation of VLCFAs in the latter cellular populations. Axonal degeneration was present in the dorsal and ventral columns in the spinal cord. Furthermore, mitochondrial, Golgi, and endoplasmic reticulum abnormalities were observed, indicative of a disturbed organellar network, which may be at the origin of the pathological cascade [19].
In addition to the mouse models described above, Abcd3 (−/−) mice have also been created. Although no full report on this mouse has yet appeared, it is clear that Abcd3 (−/−) mice have a non-shivering thermogenesis defect, which may be related to a disturbance in fasting fuel homeostasis. In addition, abnormalities have been observed in the peroxisomal metabolism of bile acid intermediates as well as pristanic acid and phytanic acid. These findings may help to unravel the function of PMP70 [36].
Plant ABCDs
Arabidopsis thaliana contains more than 100 ABC transporters, of which only two appear to belong to the ABCD branch. The first gene (AT4G39850) was identified independently by three groups of investigators, which explains the three different names PXA1 [101], PED3 [31], and CTS [21]. Interestingly, the PXA1/PED3/CTS gene encodes a full-size transporter (1,338 amino acids), with both halves (1–679 and 680–1,338) of the protein showing significant sequence identity to the human ABCDs (45% identity with human PMP70, 42% with human ALDR and ALDP, and 36% with human PMP69). The Arabidopsis genome contains another gene (AT1G54350) which codes for a hemitransporter containing one transmembrane domain followed by a single NBF that shares sequence similarity to PXA1. The identity between the two Arabidopsis proteins (21%) is less than the identity between PXA1 and the yeast (24–30%) and mammalian (36–45%) proteins. Hayashi et al. [31] identified the PXA1/PED3/CTS mutant in a collection of mutants with compromised beta-oxidation capacity as measured by the insensitivity of the mutant towards the synthetic auxin 2,4-dichlorophenoxybutyric acid (2,4-DB), which undergoes beta-oxidation to 2,4-dichlorophenoxyacetic acid in peroxisomes. Zolman et al. [101] identified the mutant in a collection of 14 Arabidopsis mutants resistant to the auxin indole-3-butyric acid (IBA), which upon beta-oxidation produces indole-3-acetic acid (IAA). Adult pxa1 plants grow slowly compared with wild type, with smaller rosettes, fewer leaves, and shorter inflorescence stems, indicating that PXA1 is important throughout development. The pxa1 mutant is resistant to the inhibition of root elongation by IBA but remains sensitive to inhibition by IAA. Similarly, the pxa1 mutant is also resistant to the inhibitory effects of 2,4-DB but is sensitive to 2,4-dichlorophenoxyacetic acid. Footitt et al. [21] showed that the germination potential of intact CTS1 seeds, in which PXA1 function is fully lost due to an insertion disruption within the Walker A motif, can be corrected by adding shorter-chain FAs, like butyrate and propionate. These results suggest that peroxisomal beta-oxidation is functional in the cts-1 mutant, and the failure to metabolise triglyceride-derived acyl–CoAs is a consequence of a defect in the transport of FAs into the peroxisome. Supportive evidence has come from the analysis of acyl–CoA esters by Footitt et al. [21], which revealed an increased acyl–CoA pool size in cts mutants with marked accumulation of the 20:1, 20:0, and 22:1 acyl–CoA esters. Recent studies by Fulda et al. [25] showed that the situation may actually be more difficult. This is concluded from studies on the two peroxisomal acyl–CoA synthetases known to be present in peroxisomes of Arabidopsis named LACS-6, a PTS1 protein, and LACS-7, a protein with both a PTS1 and PTS2 targeting signal. The single mutants, lacs6-1 and lacs7-1, were indistinguishable from the wild type in terms of germination, growth, and reproductive development. In contrast, the lacs6-1, lacs7-1 double mutant was specifically defective in seed lipid mobilisation and required exogenous sucrose for seedling establishment. This phenotype is similar to the A. thaliana pxa1 mutants deficient in the peroxisomal ABC transporter and other mutants deficient in beta-oxidation. These results indicate that peroxisomal LACS activity and the PXA1 transporter are essential for early seedling growth. The peroxisomal LACS activity would be necessary if the PXA1 transporter delivered unesterified FAs into the peroxisomal matrix. Alternatively, PXA1 and LACS6/LACS7 may act in parallel pathways that are both required to ensure adequate delivery of acyl–CoA substrates for beta-oxidation and successful seedling establishment.
In summary, although our knowledge about the peroxisomal half-ABC transporters is still only limited, much has been learned in recent years about the functional characteristics of at least some of the ABCDs, notably in the yeast S. cerevisiae. It is clear that much remains to be learned, however, about these transport proteins, which are not only present in some organisms, like yeast, plants, and mammals but show a much wider distribution as concluded from phylogenetic analyses by Sheps et al. [80] (Fig. 4).
Phylogenetic relation between reported and putative peroxisomal ABC transporters from humans (Hs), mice (Mm), Caenorhabditis elegans (Cc), Drosophila melanogaster (Dm), A. thaliana (At), and S. cerevisiae (Sc). The tree was created using the Clustal W program with default setting at the EBI server. Gen Bank accession numbers: Hs_ALDP (D1), CAA79922; Mm_ALDP (D1), NP_031461; Hs_ALDR (D2), NP_005155; Mm_ALDR (D2), NP_036124; Dm_CG2316, AAF59367; Hs_PMP70 (D3), CAA41416; Mm_PMP70 (D3), NP_033017; Dm_CG12703, AAF49018; Ce_P1, AAA68339; Ce_P2, AAA68340; Hs_PMP69 (D4), AF009746; Mm_PMP69 (D4), O89016; Ce_C54G10.3, CAA99810; At_PXA1, NP_568072; Sc_Pxa2, NP_012733; Sc_Pxa1, NP_015178
References
Albet S, Causeret C, Bentejac M, Mandel JL, Aubourg P, Maurice B (1997) Fenofibrate differently alters expression of genes encoding ATP-binding transporter proteins of the peroxisomal membrane. FEBS Lett 405:394–397
Albet S, Bentejac M, Savary S, Gondcaille C, Netik A, Berger J, Szpirer C, Troffer-Charlier N, Bugaut M (2001) Rat adrenoleukodystrophy-related (ALDR) gene: full-length cDNA sequence and new insight in expression. Biochim Biophys Acta 1517:257–269
Antonenkov VD, Van Veldhoven PP, Waelkens E, Mannaerts GP (1997) Substrate specificities of 3-oxoacyl-CoA thiolase A and sterol carrier protein 2/3-oxoacyl-CoA thiolase purified from normal rat liver peroxisomes. Sterol carrier protein 2/3-oxoacyl-CoA thiolase is involved in the metabolism of 2-methyl-branched fatty acids and bile acid intermediates. J Biol Chem 272:26023–26031
Aubourg P, Adamsbaum C, Lavallard-Rousseau MC, Lemaitre A, Boureau F, Mayer M, Kalifa G (1992) Brain MRI and electrophysiologic abnormalities in preclinical and clinical adrenomyeloneuropathy. Neurology 42:85–91
Baes M, Huyghe S, Carmeliet P, Declercq PE, Collen D, Mannaerts GP, Van Veldhoven PP (2000) Inactivation of the peroxisomal multifunctional protein-2 in mice impedes the degradation of not only 2-methyl-branched fatty acids and bile acid intermediates but also of very long chain fatty acids. J Biol Chem 275:16329–16336
Baes M, Van Veldhoven PP (2003) Lessons from knockout mice. I: Phenotypes of mice with peroxisome biogenesis disorders. Adv Exp Med Biol 544:113–122
Baumgart E, Fahimi HD, Stich A, Volkl A (1996) L-Lactate dehydrogenase A4- and A3B isoforms are bona fide peroxisomal enzymes in rat liver. Evidence for involvement in intraperoxisomal NADH reoxidation. J Biol Chem 271:3846–3855
Berger J, Albet S, Bentejac M, Netik A, Holzinger A, Roscher AA, Bugaut M, Forss-Petter S (1999) The four murine peroxisomal ABC-transporter genes differ in constitutive, inducible and developmental expression. Eur J Biochem 265:719–727
Bossier P, Fernandes L, Vilela C, Rodrigues-Pousada C (1994) The yeast YKL741 gene situated on the left arm of chromosome XI codes for a homologue of the human ALD protein. Yeast 10:681–686
Braiterman LT, Zheng S, Watkins PA, Geraghty MT, Johnson G, McGuinness MC, Moser AB, Smith KD (1998) Suppression of peroxisomal membrane protein defects by peroxisomal ATP binding cassette (ABC) proteins. Hum Mol Genet 7:239–247
Brites P, Wanders RJA, Waterham HR (2004) The mouse as a model to understand peroxisomal biogenesis and its disorders. Drug Discov Today 1:193–198
Cartier N, Guidoux S, Rocchiccioli F, Aubourg P (2000) Simvastatin does not normalize very long chain fatty acids in adrenoleukodystrophy mice. FEBS Lett 478:205–208
Causeret C, Bentejac M, Bugaut M (1993) Proteins and enzymes of the peroxisomal membrane in mammals. Biol Cell 77:89–104
Contreras M, Sengupta TK, Sheikh F, Aubourg P, Singh I (1996) Topology of ATP-binding domain of adrenoleukodystrophy gene product in peroxisomes. Arch Biochem Biophys 334:369–379
Eaton S, Bartlett K, Pourfarzam M (1996) Mammalian mitochondrial beta-oxidation. Biochem J 320:345–357
Fan CY, Pan J, Chu R, Lee D, Kluckman KD, Usuda N, Singh I, Yeldandi AV, Rao MS, Maeda N, Reddy JK (1996) Hepatocellular and hepatic peroxisomal alterations in mice with a disrupted peroxisomal fatty acyl–coenzyme A oxidase gene. J Biol Chem 271:24698–24710
Ferdinandusse S, Denis S, Mooyer PA, Dekker C, Duran M, Soorani-Lunsing RJ, Boltshauser E, Macaya A, Gartner J, Majoie CB, Barth PG, Wanders RJ, Poll-The BT (2006) Clinical and biochemical spectrum of D-bifunctional protein deficiency. Ann Neurol 59:92–104
Ferdinandusse S, Ylianttila MS, Gloerich J, Koski MK, Oostheim W, Waterham HR, Hiltunen JK, Wanders RJA, Glumoff T (2006) Mutational spectrum of D-bifunctional protein deficiency and structure based genotype–phenotype analysis. Am J Hum Genet 78:112–124
Ferrer I, Kapfhammer JP, Hindelang C, Kemp S, Troffer-Charlier N, Broccoli V, Callyzot N, Mooyer PAW, Selhorst J, Vreken P, Wanders RJA, Mandel JL, Pujol A (2005) Inactivation of the peroxisomal ABCD2 transporter in the mouse leads to late-onset ataxia involving mitochondria, Golgi and endoplasmic reticulum damage. Hum Mol Genet 14:3565–3577
Flavigny E, Sanhaj A, Aubourg P, Cartier N (1999) Retroviral-mediated adrenoleukodystrophy-related gene transfer corrects very long chain fatty acid metabolism in adrenoleukodystrophy fibroblasts: implications for therapy. FEBS Lett 448:261–264
Footitt S, Slocombe SP, Larner V, Kurup S, Wu Y, Larson T, Graham I, Baker A, Holdsworth M (2002) Control of germination and lipid mobilization by COMATOSE, the Arabidopsis homologue of human ALDP. EMBO J 21:2912–2922
Forss-Petter S, Werner H, Berger J, Lassmann H, Molzer B, Schwab MH, Bernheimer H, Zimmermann F, Nave KA (1997) Targeted inactivation of the X-linked adrenoleukodystrophy gene in mice. J Neurosci Res 50:829–843
Fourcade S, Savary S, Albet S, Gauthe D, Gondcaille C, Pineau T, Bellenger J, Bentejac M, Holzinger A, Berger J, Bugaut M (2001) Fibrate induction of the adrenoleukodystrophy-related gene (ABCD2): promoter analysis and role of the peroxisome proliferator-activated receptor PPARalpha. Eur J Biochem 268:3490–3500
Fourcade S, Savary S, Gondcaille C, Berger J, Netik A, Cadepond F, El EM, Molzer B, Bugaut M (2003) Thyroid hormone induction of the adrenoleukodystrophy-related gene (ABCD2). Mol Pharmacol 63:1296–1303
Fulda M, Schnurr J, Abbadi A, Heinz E, Browse J (2004) Peroxisomal Acyl–CoA synthetase activity is essential for seedling development in Arabidopsis thaliana. Plant Cell 16:394–405
Gartner J, Valle D (1993) The 70 kDa peroxisomal membrane protein: an ATP-binding cassette transporter protein involved in peroxisome biogenesis. Semin Cell Biol 4:45–52
Gartner J, Moser H, Valle D (1992) Mutations in the 70K peroxisomal membrane protein gene in Zellweger syndrome. Nat Genet 1:16–23
Gartner J, Kearns W, Rosenberg C, Pearson P, Copeland NG, Gilbert DJ, Jenkins NA, Valle D (1993) Localization of the 70-kDa peroxisomal membrane protein to human 1p21–p22 and mouse 3. Genomics 15:412–414
Graham IA, Eastmond PJ (2002) Pathways of straight and branched chain fatty acid catabolism in higher plants. Prog Lipid Res 41:156–181
Guimaraes CP, Domingues P, Aubourg P, Fouquet F, Pujol A, Jimenez-Sanchez G, Sa-Miranda C, Azevedo JE (2004) Mouse liver PMP70 and ALDP: homomeric interactions prevail in vivo. Biochim Biophys Acta 1689:235–243
Hayashi M, Nito K, Takei-Hoshi R, Yagi M, Kondo M, Suenaga A, Yamaya T, Nishimura M (2002) Ped3p is a peroxisomal ATP-binding cassette transporter that might supply substrates for fatty acid beta-oxidation. Plant Cell Physiol 43:1–11
Heinzer AK, Watkins PA, Lu JF, Kemp S, Moser AB, Li YY, Mihalik S, Powers JM, Smith KD (2003) A very long-chain acyl–CoA synthetase-deficient mouse and its relevance to X-linked adrenoleukodystrophy. Hum Mol Genet 12:1145–1154
Hettema EH, van Roermund CWT, Distel B, van den Berg M, Vilela C, Rodrigues-Pousada C, Wanders RJA, Tabak HF (1996) The ABC transporter proteins Pat1 and Pat2 are required for import of long-chain fatty acids into peroxisomes of Saccharomyces cerevisiae. EMBO J 15:3813–3822
Holzinger A, Kammerer S, Roscher AA (1997) Primary structure of human PMP69, a putative peroxisomal ABC-transporter. Biochem Biophys Res Commun 237:152–157
Imanaka T, Aihara K, Takano T, Yamashita A, Sato R, Suzuki Y, Yokota S, Osumi T (1999) Characterization of the 70-kDa peroxisomal membrane protein, an ATP binding cassette transporter. J Biol Chem 274:11968–11976
Jimenez-Sanchez G, Hebron KJ, Silva-Zolezzi I, Mihalik S, Watkins P, Espeel M, Moser A, Thomas G, Roels F, Valle D (2000) Fasting fuel homeostasis triggered by defective phytanic and pristanic acids metabolism in the 70 kDa peroxisomal membrane protein (PMP70) deficient mice. Am J Hum Genet 67:65
Johnson DR, Knoll LJ, Levin DE, Gordon JI (1994) Saccharomyces cerevisiae contains four fatty acid activation (FAA) genes: an assessment of their role in regulating protein N-myristoylation and cellular lipid metabolism. J Cell Biol 127:751–762
Kamijo K, Taketani S, Yokota S, Osumi T, Hashimoto T (1990) The 70-kDa peroxisomal membrane protein is a member of the Mdr (P-glycoprotein)-related ATP-binding protein superfamily. J Biol Chem 265:4534–4540
Kamijo K, Kamijo T, Ueno I, Osumi T, Hashimoto T (1992) Nucleotide sequence of the human 70 kDa peroxisomal membrane protein: a member of ATP-binding cassette transporters. Biochim Biophys Acta 1129:323–327
Kashiwayama Y, Morita M, Kamijo K, Imanaka T (2002) Nucleotide-induced conformational changes of PMP70, an ATP binding cassette transporter on rat liver peroxisomal membranes. Biochem Biophys Res Commun 291:1245–1251
Kemp S, Wei HM, Lu JF, Braiterman LT, McGuinness MC, Moser AB, Watkins PA, Smith KD (1998) Gene redundancy and pharmacological gene therapy: implications for X-linked adrenoleukodystrophy. Nat Med 4:1261–1268
Kemp S, Valianpour F, Mooyer PA, Kulik W, Wanders RJA (2004) Method for measurement of peroxisomal very-long-chain fatty acid beta-oxidation in human skin fibroblasts using stable-isotope-labeled tetracosanoic acid. Clin Chem 50:1824–1826
Kobayashi T, Shinnoh N, Kondo A, Yamada T (1997) Adrenoleukodystrophy protein-deficient mice represent abnormality of very long chain fatty acid metabolism. Biochem Biophys Res Commun 232:631–636
Kunau WH, Dommes V, Schulz H (1995) Beta-oxidation of fatty acids in mitochondria, peroxisomes, and bacteria: a century of continued progress. Prog Lipid Res 34:267–342
Lageweg W, Tager JM, Wanders RJA (1991) Topography of very-long-chain-fatty-acid-activating activity in peroxisomes from rat liver. Biochem J 276:53–56
Langmann T, Mauerer R, Zahn A, Moehle C, Probst M, Stremmel W, Schmitz G (2003) Real-time reverse transcription–PCR expression profiling of the complete human ATP-binding cassette transporter superfamily in various tissues. Clin Chem 49:230–238
Lewin TM, Van Horn CG, Krisans SK, Coleman RA (2002) Rat liver acyl–CoA synthetase 4 is a peripheral-membrane protein located in two distinct subcellular organelles, peroxisomes, and mitochondrial-associated membrane. Arch Biochem Biophys 404:263–270
Li X, Gould SJ (2002) PEX11 promotes peroxisome division independently of peroxisome metabolism. J Cell Biol 156:643–651
Liu LX, Janvier K, Berteaux-Lecellier V, Cartier N, Benarous R, Aubourg P (1999) Homo- and heterodimerization of peroxisomal ATP-binding cassette half-transporters. J Biol Chem 274:32738–32743
Lombard-Platet G, Savary S, Sarde CO, Mandel JL, Chimini G (1996) A close relative of the adrenoleukodystrophy (ALD) gene codes for a peroxisomal protein with a specific expression pattern. Proc Natl Acad Sci U S A 93:1265–1269
Lu JF, Lawler AM, Watkins PA, Powers JM, Moser AB, Moser HW, Smith KD (1997) A mouse model for X-linked adrenoleukodystrophy. Proc Natl Acad Sci U S A 94:9366–9371
Mandard S, Muller M, Kersten S (2004) Peroxisome proliferator-activated receptor alpha target genes. Cell Mol Life Sci 61:393–416
Mashek DG, Bornfeldt KE, Coleman RA, Berger J, Bernlohr DA, Black P, DiRusso CC, Farber SA, Guo W, Hashimoto N, Khodiyar V, Kuypers FA, Maltais LJ, Nebert DW, Renieri A, Schaffer JE, Stahl A, Watkins PA, Vasiliou V, Yamamoto TT (2004) Revised nomenclature for the mammalian long-chain acyl–CoA synthetase gene family. J Lipid Res 45:1958–1961
McGuinness MC, Zhang HP, Smith KD (2001) Evaluation of pharmacological induction of fatty acid beta-oxidation in X-linked adrenoleukodystrophy. Mol Genet Metab 74:256–263
McGuinness MC, Lu JF, Zhang HP, Dong GX, Heinzer AK, Watkins PA, Powers J, Smith KD (2003) Role of ALDP (ABCD1) and mitochondria in X-linked adrenoleukodystrophy. Mol Cell Biol 23:744–753
Miyazawa S, Osumi T, Hashimoto T (1980) The presence of a new 3-oxoacyl-CoA thiolase in rat liver peroxisomes. Eur J Biochem 103:589–596
Moser HW, Loes DJ, Melhem ER, Raymond GV, Bezman L, Cox CS, Lu SE (2000) X-Linked adrenoleukodystrophy: overview and prognosis as a function of age and brain magnetic resonance imaging abnormality. A study involving 372 patients. Neuropediatrics 31:227–239
Moser HW et al (2001) X-Linked adrenoleukodystrophy. In: Scriver CR et al (eds) The metabolic & molecular bases of inherited disease, 8th edn. McGraw-Hill, New York
Mosser J, Douar AM, Sarde CO, Kioschis P, Feil R, Moser H, Poustka AM, Mandel JL, Aubourg P (1993) Putative X-linked adrenoleukodystrophy gene shares unexpected homology with ABC transporters. Nature 361:726–730
Netik A, Forss-Petter S, Holzinger A, Molzer B, Unterrainer G, Berger J (1999) Adrenoleukodystrophy-related protein can compensate functionally for adrenoleukodystrophy protein deficiency (X-ALD): implications for therapy. Hum Mol Genet 8:907–913
Netik A, Hobel A, Rauschka H, Molzer B, Forss-Petter S, Berger J (2000) Rolipram does not normalize very long-chain fatty acid levels in adrenoleukodystrophy protein-deficient fibroblasts and mice. J Inherit Metab Dis 23:615–624
Oezen I, Rossmanith W, Forss-Petter S, Kemp S, Voigtlander T, Moser-Thier K, Wanders RJA, Bittner RE, Berger J (2005) Accumulation of very long-chain fatty acids does not affect mitochondrial function in adrenoleukodystrophy protein deficiency. Hum Mol Genet 14:1127–1137
Pahan K, Khan M, Singh I (1998) Therapy for X-adrenoleukodystrophy: normalization of very long chain fatty acids and inhibition of induction of cytokines by cAMP. J Lipid Res 39:1091–1100
Pai GS, Khan M, Barbosa E, Key LL, Craver JR, Cure JK, Betros R, Singh I (2000) Lovastatin therapy for X-linked adrenoleukodystrophy: clinical and biochemical observations on 12 patients. Mol Genet Metab 69:312–322
Pei Z, Fraisl P, Berger J, Jia Z, Forss-Petter S, Watkins PA (2004) Mouse very long-chain acyl–CoA synthetase 3/fatty acid transport protein 3 catalyzes fatty acid activation but not fatty acid transport in MA-10 cells. J Biol Chem 279:54454–54462
Poll-The BT, Roels F, Ogier H, Scotto J, Vamecq J, Schutgens RBH, Wanders RJA, van Roermund CWT, van Wijland MJ, Schram AW, Tager JM, Saudubray JM (1988) A new peroxisomal disorder with enlarged peroxisomes and a specific deficiency of acyl–CoA oxidase (pseudo-neonatal adrenoleukodystrophy). Am J Hum Genet 42:422–434
Pollard H, Moreau J, Aubourg P (1995) Localization of mRNAs for adrenoleukodystrophy and the 70 kDa peroxisomal (PMP70) proteins in the rat brain during post-natal development. J Neurosci Res 42:433–437
Pujol A, Troffer-Charlier N, Metzger E, Chimini G, Mandel JL (2000) Characterization of the adrenoleukodystrophy-related (ALDR, ABCD2) gene promoter: inductibility by retinoic acid and forskolin. Genomics 70:131–139
Pujol A, Hindelang C, Callizot N, Bartsch U, Schachner M, Mandel JL (2002) Late onset neurological phenotype of the X-ALD gene inactivation in mice: a mouse model for adrenomyeloneuropathy. Hum Mol Genet 11:499–505
Pujol A, Ferrer I, Camps C, Metzger E, Hindelang C, Callizot N, Ruiz M, Pampols T, Giros M, Mandel JL (2004) Functional overlap between ABCD1 (ALD) and ABCD2 (ALDR) transporters: a therapeutic target for X-adrenoleukodystrophy. Hum Mol Genet 13:2997–3006
Qi Ch, Zhu Y, Pan J, Usada N, Maeda N, Yeldandi AV, Rao MS, Hashimoto T, Reddy JK (1999) Absence of spontaneous peroxisome proliferation in enoyl–CoA hydratase/L-3-hydroxyacyl-CoA dehydrogenase-deficient mouse liver. J Biol Chem 274:15775–15780
Rampler H, Weinhofer I, Netik A, Forss-Petter S, Brown PJ, Oplinger JA, Bugaut M, Berger J (2003) Evaluation of the therapeutic potential of PPARalpha agonists for X-linked adrenoleukodystrophy. Mol Genet Metab 80:398–407
Rizzo WB, Watkins PA, Phillips MW, Cranin D, Campbell B, Avigan J (1986) Adrenoleukodystrophy: oleic acid lowers fibroblast saturated C22–26 fatty acids. Neurology 36:357–361
Savary S, Troffer-Charlier N, Gyapay G, Mattei MG, Chimini G (1997) Chromosomal localization of the adrenoleukodystrophy-related gene in man and mice. Eur J Hum Genet 5:99–101
Seedorf U, Raabe M, Ellinghaus P, Kannenberg F, Fobker M, Engel T, Denis S, Wouters F, Wirtz KWA, Wanders RJA, Maeda N, Assmann G (1998) Defective peroxisomal catabolism of branched fatty acyl coenzyme A in mice lacking the sterol carrier protein-2/sterol carrier protein-x gene function. Genes Dev 12:1189–1201
Shani N, Valle D (1996) A Saccharomyces cerevisiae homolog of the human adrenoleukodystrophy transporter is a heterodimer of two half ATP- binding cassette transporters. Proc Natl Acad Sci USA 93:11901–11906
Shani N, Watkins PA, Valle D (1995) PXA1, a possible Saccharomyces cerevisiae ortholog of the human adrenoleukodystrophy gene. Proc Natl Acad Sci USA 92:6012–6016
Shani N, Sapag A, Valle D (1996) Characterization and analysis of conserved motifs in a peroxisomal ATP-binding cassette transporter. J Biol Chem 271:8725–8730
Shani N, Jimenez-Sanchez G, Steel G, Dean M, Valle D (1997) Identification of a fourth half ABC transporter in the human peroxisomal membrane. Hum Mol Genet 6:1925–1931
Sheps JA, Ralph S, Zhao Z, Baillie DL, Ling V (2004) The ABC transporter gene family of Caenorhabditis elegans has implications for the evolutionary dynamics of multidrug resistance in eukaryotes. Genome Biol 5:R15
Singh I, Moser AE, Goldfischer S, Moser HW (1984) Lignoceric acid is oxidized in the peroxisome: implications for the Zellweger cerebro-hepato-renal syndrome and adrenoleukodystrophy. Proc Natl Acad Sci USA 81:4203–4207
Singh I, Khan M, Key L, Pai S (1998) Lovastatin for X-linked adrenoleukodystrophy. N Engl J Med 339:702–703
Singh I, Pahan K, Khan M (1998) Lovastatin and sodium phenylacetate normalize the levels of very long chain fatty acids in skin fibroblasts of X-adrenoleukodystrophy. FEBS Lett 426:342–346
Smith KD, Kemp S, Braiterman LT, Lu JF, Wei HM, Geraghty M, Stetten G, Bergin JS, Pevsner J, Watkins PA (1999) X-Linked adrenoleukodystrophy: genes, mutations, and phenotypes. Neurochem Res 24:521–535
Swartzman EE, Viswanathan MN, Thorner J (1996) The PAL1 gene product is a peroxisomal ATP-binding cassette transporter in the yeast Saccharomyces cerevisiae. J Cell Biol 132:549–563
Tanaka AR, Tanabe K, Morita M, Kurisu M, Kasiwayama Y, Matsuo M, Kioka N, Amachi T, Imanaka T, Ueda K (2002) ATP binding/hydrolysis by and phosphorylation of peroxisomal ATP-binding cassette proteins PMP70 (ABCD3) and adrenoleukodystrophy protein (ABCD1). J Biol Chem 277:40142–40147
Troffer-Charlier N, Doerflinger N, Metzger E, Fouquet F, Mandel JL, Aubourg P (1998) Mirror expression of adrenoleukodystrophy and adrenoleukodystrophy related genes in mouse tissues and human cell lines. Eur J Cell Biol 75:254–264
van Roermund CWT, Elgersma Y, Singh N, Wanders RJA, Tabak HF (1995) The membrane of peroxisomes in Saccharomyces cerevisiae is impermeable to NAD(H) and acetyl–CoA under in vivo conditions. EMBO J 14:3480–3486
van Roermund CWT, Tabak HF, van den Berg M, Wanders RJA, Hettema EH (2000) Pex11p plays a primary role in medium-chain fatty acid oxidation, a process that affects peroxisome number and size in Saccharomyces cerevisiae. J Cell Biol 150:489–497
Vanhove GF, Van Veldhoven PP, Fransen M, Denis S, Eyssen HJ, Wanders RJA, Mannaerts GP (1993) The CoA esters of 2-methyl-branched chain fatty acids and of the bile acid intermediates di- and trihydroxycoprostanic acids are oxidized by one single peroxisomal branched chain acyl–CoA oxidase in human liver and kidney. J Biol Chem 268:10335–10344
Verleur N, Elgersma Y, van Roermund CWT, Tabak HF, Wanders RJA (1997) Cytosolic aspartate aminotransferase encoded by the AAT2 gene is targeted to the peroxisomes in oleate-grown Saccharomyces cerevisiae. Eur J Biochem 247:972–980
Verrips A, Willemsen MA, Rubio-Gozalbo E, De JJ, Smeitink JA (2000) Simvastatin and plasma very-long-chain fatty acids in X-linked adrenoleukodystrophy. Ann Neurol 47:552–553
Wanders RJA (2004) Metabolic and molecular basis of peroxisomal disorders: a review. Am J Med Genet 126A:355–375
Wanders RJA (2004) Peroxisomes, lipid metabolism, and peroxisomal disorders. Mol Genet Metab 83:16–27
Wanders RJA, Waterham HR (2006) Biochemistry of mammalian peroxisomes revisited. Annu Rev Biochem 75:295–332
Weinhofer I, Forss-Petter S, Zigman M, Berger J (2002) Cholesterol regulates ABCD2 expression: implications for the therapy of X-linked adrenoleukodystrophy. Hum Mol Genet 11:2701–2708
Weinhofer I, Kunze M, Rampler H, Bookout AL, Forss-Petter S, Berger J (2005) Liver X receptor alpha interferes with SREBP1c-mediated Abcd2 expression. Novel cross-talk in gene regulation. J Biol Chem 280:41243–41251
Wende AR, Huss JM, Schaeffer PJ, Giguere V, Kelly DP (2005) PGC-1alpha coactivates PDK4 gene expression via the orphan nuclear receptor ERRalpha: a mechanism for transcriptional control of muscle glucose metabolism. Mol Cell Biol 25:10684–10694
Yamada T, Taniwaki T, Shinnoh N, Uchiyama A, Shimozawa N, Ohyagi Y, Asahara H, Kira J (1999) Adrenoleukodystrophy protein enhances association of very long-chain acyl-coenzyme A synthetase with the peroxisome. Neurology 52:614–616
Yamada T, Shinnoh N, Taniwaki T, Ohyagi Y, Asahara H, Horiuchi, Kira J (2000) Lovastatin does not correct the accumulation of very long-chain fatty acids in tissues of adrenoleukodystrophy protein-deficient mice. J Inherit Metab Dis 23:607–614
Zolman BK, Silva ID, Bartel B (2001) The Arabidopsis pxa1 mutant is defective in an ATP-binding cassette transporter-like protein required for peroxisomal fatty acid beta-oxidation. Plant Physiol 127:1266–1278
Acknowledgements
The authors gratefully thank Mrs. Maddy Festen for expert preparation oft the manuscript, Mr. Jos Ruiter for preparation of the figures, and the following organizations for financial support: FP6 European Union Project ‘Peroxisome’ (project no. LSHG-CT-2004-512018); European Union Project ‘X-ALD’ (project no. LSHM-CT2004-502987X-ALD), and an ELA project entitled ‘Elongation of very-long-chain fatty acids in X-linked adrenoleukodystrophy: an option for a therapy’.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wanders, R.J.A., Visser, W.F., van Roermund, C.W.T. et al. The peroxisomal ABC transporter family. Pflugers Arch - Eur J Physiol 453, 719–734 (2007). https://doi.org/10.1007/s00424-006-0142-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-006-0142-x