Abstract
Background
Long-term ventilation in intensive care units (ICUs) is associated with several problems such as increased mortality, increased rates of ventilator-associated pneumonia (VAP), and prolonged time of hospitalization, and thus leads to enormous healthcare expenditure. While the influence of tracheostomy on VAP incidence, duration of ventilation, and time of hospitalization has already been analyzed in several studies, the timing of the tracheostomy procedure on patient’s mortality is still controversial. The aim of our study was to investigate whether early tracheostomy improved outcome in critically ill patients.
Materials and methods
Within 2 years, 100 critically ill, predominantly surgical patients entered this prospective randomized study. A percutaneous dilatational tracheostomy was performed either early (≤4 days, 2.8 days median) or late (≥6 days, 8.1 days median) after intubation.
Results
We could demonstrate that mortality was not significantly reduced in the early tracheostomy (ET) group in contrast to the late tracheostomy (LT) group. ET was associated with decreased VAP incidence (ET 38% vs. LT 64%), decreased duration of ventilation (ET 367.5 h vs LT 507.5 h), and shorter time of hospitalization both in hospital (ET 31.5 days vs LT 68 days) and in ICU (ET 21.5 days vs LT 27 days).
Conclusion
Despite many advantages like reduced time of ventilation and hospitalization, early tracheostomy is not associated with decreased mortality in critically ill patients.
Similar content being viewed by others
Introduction
Long-term ventilation of critically ill patients is associated with several complications. Despite improved hygiene in ICUs, ventilator-associated pneumonia (VAP) is still a major cause of patient death [1, 2]. Long-term ventilation leads to an increased risk of mechanical complications, such as tube disconnection, mucus impaction, and laryngeal and tracheal ulcera [3–5]. To resolve these problems, enormous manpower and materials are necessary that are associated with increased costs of treatment [6, 7]. Thus, both patients and hospital would profit from shortened duration of ventilation and hospitalization in general.
The percutaneous dilatational tracheostomy (PDT) is one standard procedure in airway management of long-term ventilated ICU patients [8–10]. Both open and percutaneous dilatational tracheostomies provide a safe airway, lower airway resistance, improved bronchial drainage, and high patient comfort with decreased need for sedation and a shortened weaning phase [8–11]. Furthermore, the PDT has at least three additional advantages: (a) the PDT is a bedside procedure (decreased need for human resources of the operation room) [12, 13], (b) the PDT is a safe, established method, with lower rates of mortality [14, 15], and (c) the PDT provides an adequate cosmetic result after tube removal [9, 12, 16, 17].
Although several studies have analyzed the advantages of the tracheostomy procedure, the optimal timing for the tracheostomy performance is still controversial [18–23]. This is at least partially caused by the lack of randomized, prospective studies and the heterogeneity in the studies that have been performed so far. While some studies included both surgical tracheostomy and PDT [24], other authors did not even mention the exact tracheostomy technique [25]. In most studies conducted at medical ICUs, surgical trauma patients have been excluded by the admission policy [26]. Furthermore, studies with large numbers of cases were mostly retrospective [27], while prospective studies with adequate case numbers normally excluded surgical patients [28]. While the positive impact of an ET on duration of hospitalization, on duration of ventilation, and on the VAP incidence has been shown in many studies, data concerning the mortality remain contradictory [26]. Only one retrospective study analyzed the long-term outcome of early and late tracheostomy regarding mortality [29]. Considering all the abovementioned facts, it stays nebulous if a PDT performance early after a trauma or an operation really improves the outcome of our critically ill patients whom we treat daily with this technique. The aim of this prospective study is to investigate whether an early PDT performance improves the mortality, the VAP incidence, and the time of hospitalization of mainly surgical critically ill patients.
Patients and methods
After approval by the ethics committee, 100 critically ill patients of the surgical, neurosurgical, and neurologic ICU entered this prospective, randomized study, which was performed within 2 years in the Department of Anaesthesiology, Intensive Care Medicine and Pain Therapy of the University Hospital of Gießen, Germany. Study registration number is ISRCTN01157856 and was performed after study completion.
All study patients had either been hospitalized after intubation or were intubated during hospital stay. Inclusion criteria were (a) age > 18 years, (b) an expected time of ventilation > 21 days (, which was decided by two independent intensivists, who were not involved in the study), and (c) an informed consent that the patient may be included into the study.
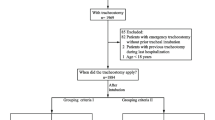
Patients were excluded from this study if they have met one of the following criteria: (a) anatomic variants or deformities of the larynx, trachea, and collum; (b) a pre-existing tracheostomy; (c) pre-existing pneumonia; (d) a critical trauma of the cervical vertebral column; (d) a coagulopathy (thrombocytes < 60,000 μL, prothrombin time > 40 s, international normalized ratio > 1.4); (e) estimated to die within the next 24 h; (f) a planned permanent tracheostomy (after laryngectomy); and (g) more than 3 days of ventilation before entry into the study. Consent was obtained for the study enrollment and the performance of PDT procedure. Due to the fact that all patients were intubated, we always established a legal guardian (or relatives receiving the status of a legal guardian by the court) in all cases. He/she representatively signed the informed consent.
After endotracheal intubation, patients were included into the study and subdivided into two groups. Patients were enrolled in a high-injury severity group with APACHE II score > 25 or the low-injury severity group with APACHE II score < 25. The APACHE II score is an established, standardized ICU prediction score and was calculated as published previously [30]. Patients were further randomized according to two computer-based, independent lists and either entered the ET (PDT ≤4 days after intubation) or LT (PDT ≥6 days after intubation) tracheostomy trunk of this study. To maintain allocation concealment, these lists were only available to the study team, which had no contact to the ICU team.
PDT was performed according to the operating procedure published by Ciaglia in 1985. Besides the different timing of PDT performance, all co-interventions were similar in both groups. Primary endpoint of this study was the death of a patient. After discharge from hospital, patients left the observation automatically.
All patients were weaned according to an established standardized weaning protocol. End of ventilation was defined as point of time at which the patient was independent from any ventilatory support (such as continuous positive airway pressure) and did not require it again during hospitalization. This, of course, does not automatically coincide with decannulation of the patient. All patients were weaned according to a standardized weaning protocol. The assessment of the data of mandatory ventilation was performed by an intensive care doctor, who was not a member of the study team. Death of a patient was determined clinically. In some cases, an autopsy was performed.
Occurrence of VAP was identified by calculation of the Clinical Pulmonary Infection Score (CPIS). As described previously [31], the CPIS is an established clinical score to identify a VAP of critically ill patients and was calculated at every day after tracheostomy. To exclude a preexisting VAP, the CPIS was calculated once before PDT performance. Data assessment was performed by a medical doctor experienced in intensive care medicine, who was not part of the study team. This observer was not informed about the time point of tracheostomy performance to avoid ascertainment bias.
Statistical analyses were performed with SPSS software for Windows (Statistical Product and Service Solutions, version 15.0.0, SSPS Inc, Chicago, IL, USA). For mortality, the Fisher exact test for hospitalization and time of ventilation the Mann–Whitney U test and the Shapiro–Wilk test were performed. Incidence of VAP was evaluated with the chi-square test.
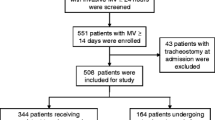
Figure 1 provides a CONSORT flow chart summarizing the patient enrollment.
Results
One hundred patients (64 females, 36 males) with different patterns of injury were included in this study (Fig. 2). Sixty-five patients from a surgical ICU, 24 patients from a neurosurgical, and 11 patients from a neurological ICU have been enrolled to this prospective study.
Subgroups of different injury or disease undergoing tracheostomy in this study. We included patients suffering from neurological disorders (mainly: cerebral infarction), neurosurgical injuries (mainly cerebral bleeding), non-septic patients after visceral surgery (large operations together with multiple preexisting medical disorders), septic patients with a peritonitis, trauma patients with multiple, different injury patterns, patients after visceral surgery who developed respiratory problems (COPD, emphysema, fibrosis, pneumonia), one patient with cardiac decompensation, and three patients suffering from urosepsis
Tracheostomy was performed 2.8 days (interquartile range (IQR) [2.2–3.6]) after intubation in the ET group. In the LT group, patients were tracheostomized after 8.1 days (IQR [6.1–10.6]) (Fig. 3). With APACHE II scores of 21 (IQR [12–31]) in the ET group and 22.3 (IQR [10–33]) in the LT group, both groups did not show a statistical difference in severity of illness (Table 1).
Hospital mortality was the primary endpoint of the study. Considering the total hospital mortality (ET, 20%; LT, 22%) the majority of patients died in the ICU. Analysis of the subpopulations did not reveal a difference in mortality between ET and LT both in the subpopulation with APACHE > 25 and APACHE < 25 (Fig. 4). As for the hospital mortality (P = .81), there was no significant difference in ICU mortality between the ET (9 patients, 18%) and the LT group (7 patients, 14%) (P = .79). Table 2 summarizes the causes of death by treatment group. Time of hospitalization in the ICU was significantly reduced in the ET group (21.5 days, IQR [15–30]) compared to the LT group (27 days, IQR [22–37]) (P ≤ .05) (Table 1). While patients of the LT group were hospitalized for 68 days average (IQR [24.5–124]), the time of hospitalization was significantly shortened in the ET group (31.5 days, IQR [22.5–59.5]) (P ≤ .05) (Table 1). Time of ventilation was even significantly reduced in the ET group (367.5 h, IQR [219–475.5]) compared to the LT group (507.5 h, IQR [323–670.5]) (P ≤ .01) (Table 1).
With 38.5%, VAP incidence was significantly decreased in the ET group compared with the LT group (64%) (Table 1). Patients developed a late-onset VAP, with a bacterial spectrum mainly consisting of Pseudomonas aeruginosa, methicillin-resistant Staphylococcus aureus, Klebsiella pneumoniae, and gram-negative bacteria.
Table 1 shows a summary of the data generated by this study.
Discussion
Mortality rate in the ET group indicated a relative decrease of 10% compared to the LT group. In our study, with a limited number of patients, this does not lead to a significant difference in patients’ mortality. Nevertheless, patients of the early group spent significantly less time in the ICU and in hospital in general. In this prospective, randomized study, we tried to include patients of ICUs of different medical specialty. We thus present the first prospective, randomized study on surgical patients analyzing the impact of early PDT performance. Due to the fact that no study with a sufficient case number was performed comparing early and late tracheostomy on surgical patients prospectively, our analysis has a pilot study character. Thus, a sample size estimation was not performed. The inclusion of 100 critically ill patients into this study seemed to be adequate for this pilot study design.
Both retrospective and prospective studies that analyze the impact of timing of PDT performance have been published. To the best of our knowledge, most prospective studies including surgical patients present only low numbers of patients [32, 33]. In contrast, retrospective studies were able to recruit up to 10,927 patients [24, 29] but included only patients from medical ICUs. In the study presented, we included patients who were not recruited from medical ICUs on the one hand, but suffered from a great variety of disorders (Fig. 2) (trauma, visceral surgery, neurosurgery, neurological) on the other hand. This broad spectrum of patients could, of course, bias the results. Nevertheless, this prospective pilot study gives first interesting results. For a multi-center approach analyzing the impact of an early tracheostomy performance on critically ill surgical patients, another study design could be helpful to reduce this inhomogeneity in the study groups.
Furthermore, the definition of the ET timing varies depending on the different study protocols [23, 25, 28, 34–37]. Reviewing the literature of the last years, the definition of an ET interestingly shifted from 3 weeks to few days after intubation. As a consequence, we decided to define an ET as a PDT performed within up to 4 days after intubation, and thus chose a very short time span between intubation and PDT compared to the literature. The establishment of a legal guardian made a tracheostomy immediately after intubation impossible. ET was done after 2.8 days of intubation median. LT is defined as a tracheostomy >14 days after trauma in most studies. This, of course, strengthens the disadvantages of long-term intubation and—to the authors’ opinion—does not state the best patients’ care in ICU medicine. In our study, the LT patients were tracheostomized 8.1 days after intubation median.
In the study of Rumbak and colleagues [26], ET was performed within 48 h after intubation. Late tracheostomy was done after 14 days. This great difference of course strengthens the effects of the tracheostomy timing. Compared to Rumbak, who only included critically ill patients from medical ICUs, we analyzed patients from a mainly surgical spectrum of injury pattern. In the study of Arabi and colleagues [23], day 7 after intubation is the limit for early and the beginning of the late tracheostomy. It is impossible to predict whether a different definition of ET (like within 24 h, 48 h, or even immediately after intubation) will effect mortality or not. Considering the LT group in more detail, there were also some patients included who underwent tracheostomy 21 days (n = 1) or even 24 days (n = 1) after intubation. Thus, we must also diminish the inhomogeneity within the LT group in future studies. Nevertheless, these single cases of a very late tracheostomy reflect the clinical situation in our university hospital. Due to the heterogeneity of the different study populations and the different definitions of early and late tracheostomy, none of the studies published up to now can be easily compared to each other. Further evaluation in prospective studies is required.
Additionally, the different severity and manner of disorder or trauma leads to a lack of comparability of the studies published so far. Compared to our study, reports with both higher and lower APACHE II scores exist [26, 38]. To the best of our knowledge, this inhomogeneity in injury is not discussed in the reviews published. The duration of ventilation is currently affected by the pattern of injury before intubation and by PDT performance, respectively. Obviously, the outcome of ET timing differs between patients with primary pulmonary disorders and patients whose injuries secondarily require ventilatory assistance. Despite a sufficient, spontaneous ventilation, some neurosurgical patients in our study have required a tracheostomy caused by permanent neuromotoric dysphagia. In these cases, persistent tracheostomy serves as a protection against aspiration, and thus, these patients would have caused false results of respirator dependency. To avoid this effect, the end of ventilation was not defined as point of decannulation but as postoperative time point at which spontaneous ventilation (T piece) occurred in this study. As shown in Table 1, we were quite successful to reach equal APACHE II scores in both the ET and the LT groups. Nevertheless, it is a well-known fact that especially patients suffering from a septic process form a very inhomogeneous group. The review of literature reveals that the APACHE II score is a good but still not the optimal score to equalize the groups concerning their severity of disorder.
In a prospective study, Rumbak and colleagues analyzed 120 critically ill patients from medical ICUs concerning the time point of tracheostomy. Mortality was reduced by approximately 50% [26]. In contrast to our study, only nonsurgical patients from medical ICUs were analyzed. Additionally, the level of impairment measured by APACHE II was higher (APACHE II of ET group 27, in LT group 26) in comparison to our study (APACHE II of ET group 22.8, in LT group 22.3). Consequently, an increased mortality of the LT group (61.7% vs. 18% in our study) served as the basis of mortality of the ET group. The reduction of mortality of the ET group thus referred to a dramatically high “basal” mortality of the LT group (50% reduction of mortality vs 0% in our study).
Arabi and colleagues [23] (653 trauma patients) and Bouderka and colleagues [32] (62 neurosurgical patients) could not prove any impact of ET on mortality either. In contrast, Scales and colleagues demonstrated a minor advantage of ET compared to LT after 90 days or even 1 year after intervention [29]. In conclusion, the heterogeneity of all preexisting studies analyzing the impact of ET on mortality is the dominating cause for the differences in the respective results: study design, severity, and pattern of injury or disorder, as well as differences in the specialty of the ICUs that have been set.
In our prospective study, incidence of pneumonia was significantly reduced by a PDT performed shortly after intubation. In respect of this result, our study is in concordance with many previously published studies. The effect of VAP incidence reduction differs between these studies, which can be attributed to the inhomogeneous definition of “early tracheostomy” [22]. Our study demonstrated a shortening of ventilator dependency by 140 h for the ET group compared to the LT group, which has been a significant effect. Nevertheless, the cause of reduction by tracheostomy (reduction of airway resistance, improved bronchial lavage, reduced VAP incidence) needs to be evaluated. Although a reduction of VAP incidence and duration of ventilation by ET is a well-known fact in ICU, it is still a matter of discussion why there is no influence on mortality. As published recently, there is a lack of data concerning mortality due to VAP in patients with trauma or acute respiratory distress syndrome [39]. Nevertheless, a correlation between mortality and VAP incidence in certain subgroups of ICU patients can be assumed. Bonten and colleagues recommend a more detailed subgroup analysis to clarify the attributable mortality of VAP in the ICU [39].
Both time of hospitalization in the ICU and length of hospital care were significantly decreased by early PDT performance. Like in many other studies, hospitalization was reduced by more than 50%, but again, literature is characterized by a strong inhomogeneity of study design with large differences in the outcome [23, 26, 33]. In some studies, ventilated patients were discharged from the ICU and hospitalized on intermediate care units [26]. Our study protocol allowed a transfer of patients to the neurologic rehabilitation hospitals without discontinuation of data collection.
We showed that long-term ventilated patients profit from early PDT performance and have significantly reduced incidence of VAP, and times of mechanical ventilation and hospitalization, but no significant decrease in mortality. The contradiction to some studies that could demonstrate an advantage of ET on patients’ survival could support the hypothesis that certain subpopulations with special disorders strongly profit from ET. This is in line with data from Melsen et al., who came to the same conclusion recently [39]. Our prospective single-center study included 100 patients undergoing tracheostomy. To detect a meaningful difference between early and late tracheostomy in mortality, this study is probably underpowered. Only a prospective multicenter study with higher case numbers could draw a homogenous, clear picture of the clinical impact, which an early PDT has on critically ill patients.
Conclusions
Long-term mechanical ventilation in intensive care units is associated with increased mortality, increased rates of VAP, and prolonged time of hospitalization. While there is no doubt that tracheostomy is beneficial for ICU patients, we wanted to analyze the impact of early tracheostomy performance on surgical intensive care patients.
Results revealed that ET is associated with a decreased VAP incidence and a decreased duration of mechanical ventilation on ICU. Furthermore, patients of the ET group had shorter times of hospitalization both in hospital and in ICU. Considering all these important differences, the authors draw the conclusion that surgical intensive care patients benefit from an early performance of PDT if a long-term ventilation is to be expected. Whether the advantages of an ET have an impact on a potentially decreased mortality should be analyzed in a prospective randomized multicenter study.
Key messages
-
In contrast to late tracheostomy (≥6 days after intubation), the performance of percutaneous dilatational tracheostomy (PDT) early (≤4 days) after intubation is associated with decreased VAP incidence.
-
Early tracheostomy patients have a shorter time of hospitalization both in ICU and in hospital.
-
Early tracheostomy is associated with a decreased duration of ventilatory support.
-
Mortality is not significantly reduced by early performance of PDT.
References
Rello J, Ollendorf DA, Oster G, Vera-Llonch M, Bellm L, Redman R et al (2002) Epidemiology and outcomes of ventilator-associated pneumonia in a large US database. Chest 122(6):2115–2121
Smith RL, Sawyer RG, Pruett TL (2003) Hospital-acquired infections in the surgical intensive care: epidemiology and prevention. Zentralbl Chir 128(12):1047–1061
Whited RE (1984) A prospective study of laryngotracheal sequelae in long-term intubation. Laryngoscope 94(3):367–377
Gaynor EB, Greenberg SB (1985) Untoward sequelae of prolonged intubation. Laryngoscope 95(12):1461–1467
Aadahl P, Nordgard S (1999) Percutaneous dilatational tracheostomy in a patient with thyroid cancer and severe airway obstruction. Acta Anaesthesiol Scand 43(4):483–485
Warren DK, Shukla SJ, Olsen MA, Kollef MH, Hollenbeak CS, Cox MJ et al (2003) Outcome and attributable cost of ventilator-associated pneumonia among intensive care unit patients in a suburban medical center. Crit Care Med 31(5):1312–1317
Cocanour CS, Ostrosky-Zeichner L, Peninger M, Garbade D, Tidemann T, Domonoske BD et al (2005) Cost of a ventilator-associated pneumonia in a shock trauma intensive care unit. Surg Infect (Larchmt ) 6(1):65–72
Mansharamani NG, Koziel H, Garland R, LoCicero J III, Critchlow J, Ernst A (2000) Safety of bedside percutaneous dilatational tracheostomy in obese patients in the ICU. Chest 117(5):1426–1429
Freeman BD, Isabella K, Cobb JP, Boyle WA III, Schmieg RE Jr, Kolleff MH et al (2001) A prospective, randomized study comparing percutaneous with surgical tracheostomy in critically ill patients. Crit Care Med 29(5):926–930
Mittendorf EA, McHenry CR, Smith CM, Yowler CJ, Peerless JR (2002) Early and late outcome of bedside percutaneous tracheostomy in the intensive care unit. Am Surg 68(4):342–346
Ernst A, Critchlow J (2003) Percutaneous tracheostomy—special considerations. Clin Chest Med 24(3):409–412
Bowen CP, Whitney LR, Truwit JD, Durbin CG, Moore MM (2001) Comparison of safety and cost of percutaneous versus surgical tracheostomy. Am Surg 67(1):54–60
Cobean R, Beals M, Moss C, Bredenberg CE (1996) Percutaneous dilatational tracheostomy. A safe, cost-effective bedside procedure. Arch Surg 131(3):265–271
Waller EA, Aduen JF, Kramer DJ, Alvarez F, Heckman MG, Crook JE et al (2007) Safety of percutaneous dilatational tracheostomy with direct bronchoscopic guidance for solid organ allograft recipients. Mayo Clin Proc 82(12):1502–1508
Boonsarngsuk V, Kiatboonsri S, Choothakan S (2007) Percutaneous dilatational tracheostomy with bronchoscopic guidance: Ramathibodi experience. J Med Assoc Thai 90(8):1512–1517
Toye FJ, Weinstein JD (1986) Clinical experience with percutaneous tracheostomy and cricothyroidotomy in 100 patients. J Trauma 26(11):1034–1040
Freeman BD, Isabella K, Lin N, Buchman TG (2000) A meta-analysis of prospective trials comparing percutaneous and surgical tracheostomy in critically ill patients. Chest 118(5):1412–1418
Groves DS, Durbin CG Jr (2007) Tracheostomy in the critically ill: indications, timing and techniques. Curr Opin Crit Care 13(1):90–97
Marsh HM, Gillespie DJ, Baumgartner AE (1989) Timing of tracheostomy in the critically ill patient. Chest 96(1):190–193
McWhorter AJ (2003) Tracheotomy: timing and techniques. Curr Opin Otolaryngol Head Neck Surg 11(6):473–479
Pryor JP, Frankel HL, Reilly PM, Hanson CW, Schwab CW (2000) Bedside percutaneous versus open tracheostomy. Crit Care Med 28(9):3372–3373
Shirawi N, Arabi Y (2006) Bench-to-bedside review: early tracheostomy in critically ill trauma patients. Crit Care 10(1):201
Arabi Y, Haddad S, Shirawi N, Al Shimemeri A (2004) Early tracheostomy in intensive care trauma patients improves resource utilization: a cohort study and literature review. Crit Care 8(5):R347–R352
Hsu CL, Chen KY, Chang CH, Jerng JS, Yu CJ, Yang PC (2005) Timing of tracheostomy as a determinant of weaning success in critically ill patients: a retrospective study. Crit Care 9(1):R46–R52
Lesnik I, Rappaport W, Fulginiti J, Witzke D (1992) The role of early tracheostomy in blunt, multiple organ trauma. Am Surg 58(6):346–349
Rumbak MJ, Newton M, Truncale T, Schwartz SW, Adams JW, Hazard PB (2004) A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit Care Med 32(8):1689–1694
Blot F, Similowski T, Trouillet JL, Chardon P, Korach JM, Costa MA et al (2008) Early tracheotomy versus prolonged endotracheal intubation in unselected severely ill ICU patients. Intensive Care Med 34(10):1779–1787
D'Amelio LF, Hammond JS, Spain DA, Sutyak JP (1994) Tracheostomy and percutaneous endoscopic gastrostomy in the management of the head-injured trauma patient. Am Surg 60(3):180–185
Scales DC, Thiruchelvam D, Kiss A, Redelmeier DA (2008) The effect of tracheostomy timing during critical illness on long-term survival. Crit Care Med 36(9):2547–2557
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13(10):818–829
Gursel G, Demirtas S (2006) Value of APACHE II, SOFA and CPIS scores in predicting prognosis in patients with ventilator-associated pneumonia. Respiration 73(4):503–508
Bouderka MA, Fakhir B, Bouaggad A, Hmamouchi B, Hamoudi D, Harti A (2004) Early tracheostomy versus prolonged endotracheal intubation in severe head injury. J Trauma 57(2):251–254
Barquist ES, Amortegui J, Hallal A, Giannotti G, Whinney R, Alzamel H et al (2006) Tracheostomy in ventilator dependent trauma patients: a prospective, randomized intention-to-treat study. J Trauma 60(1):91–97
Rodriguez JL, Steinberg SM, Luchetti FA, Gibbons KJ, Taheri PA, Flint LM (1990) Early tracheostomy for primary airway management in the surgical critical care setting. Surgery 108(4):655–659
Armstrong PA, McCarthy MC, Peoples JB (1998) Reduced use of resources by early tracheostomy in ventilator-dependent patients with blunt trauma. Surgery 124(4):763–766
Brook AD, Sherman G, Malen J, Kollef MH (2000) Early versus late tracheostomy in patients who require prolonged mechanical ventilation. Am J Crit Care 9(5):352–359
Sugerman HJ, Wolfe L, Pasquale MD, Rogers FB, O'Malley KF, Knudson M et al (1997) Multicenter, randomized, prospective trial of early tracheostomy. J Trauma 43(5):741–747
Kollef MH, Ahrens TS, Shannon W (1999) Clinical predictors and outcomes for patients requiring tracheostomy in the intensive care unit. Crit Care Med 27(9):1714–1720
Melsen WG, Rovers MM, Bonten MJ (2009) Ventilator-associated pneumonia and mortality: a systematic review of observational studies. Crit Care Med 37(10):2709–2718
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Tillo Koch and Birgit Hecker equally contributed to this paper.
Rights and permissions
About this article
Cite this article
Koch, T., Hecker, B., Hecker, A. et al. Early tracheostomy decreases ventilation time but has no impact on mortality of intensive care patients: a randomized study. Langenbecks Arch Surg 397, 1001–1008 (2012). https://doi.org/10.1007/s00423-011-0873-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-011-0873-9