Abstract
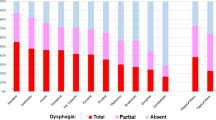
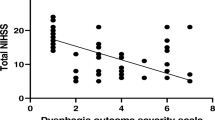
Dysphagia is found in up to 80% of acute stroke patients. To date most studies have focused on ischemic stroke only. Little is known about the incidence and pattern of dysphagia in hemorrhagic stroke. Here we describe the characteristics of dysphagia in patients with striatocapsular hemorrhage. Fiberoptic Endoscopic Evaluation of Swallowing (FEES) was carried out in 30 patients with acute striatocapsular hemorrhage. Dysphagia was classified according to the six-point Fiberoptic Endoscopic Dysphagia Severity Scale (FEDSS) within 72 h after admission. Lesion volume, hemisphere and occurrence of ventricular rupture were determined from computer tomography scans. Data on initial NIH-SS, clinical symptoms, need for endotracheal intubation, diagnosis of pneumonia and feeding status on discharge were recorded. Swallowing impairment was observed in 76.7% of patients (n = 23). Mean FEDSS score was 3.1 ± 1.5. Main findings were penetration or aspiration of liquids as well as leakage to valleculae and piriform sinus. Incidence of pneumonia was 30.0% (n = 9). Age, NIH-SS and hematoma volume did not correlate with dysphagia severity. None of the clinical characteristics was predictive for dysphagia. On discharge after 12.9 ± 5.3 days, a two-point improvement on the FEDSS was seen in seven patients, (30.4%) and five patients (21.7%) had gained at least one point. In striatocapsular hemorrhage, dysphagia is a common and so far underrecognized symptom. FEES results indicate predominant impairment of oral motor control. Swallowing impairment is not related to other clinical deficits, stroke severity or lesion characteristics. Thus, detailed dysphagia assessment is indicated in all cases.
Similar content being viewed by others
References
Alberts MJ, Horner J, Gray L, Brazer SR (1992) Aspiration after stroke: lesion analysis by brain MRI. Dysphagia 7:170–173
Arboix A, Vall-Llosera A, Garcia-Eroles L, Massons J, Oliveres M, Targa C (2002) Clinical features and functional outcome of intracerebral hemorrhage in patients aged 85 and older. J Am Geriatr Soc 50:449–454
Aydogdu I, Ertekin C, Tarlaci S, Turman B, Kiylioglu N, Secil Y (2001) Dysphagia in lateral medullary infarction (Wallenberg’s syndrome): an acute disconnection syndrome in premotor neurons related to swallowing activity? Stroke 32:2081–2087
Badjatia N, Rosand J (2005) Intracerebral hemorrhage. Neurologist 11:311–324
Barer DH (1989) The natural history and functional consequences of dysphagia after hemispheric stroke. J Neurol Neurosurg Psychiatry 52:236–241
Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster G (1993) Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke 24:987–993
Brott T, Adams HP Jr, Olinger CP, Marler JR, Barsan WG, Biller J, Spilker J, Holleran R, Eberle R, Hertzberg V (1989) Measurements of acute cerebral infarction: a clinical examination scale. Stroke 20:864–870
Carnaby G, Hankey GJ, Pizzi J (2006) Behavioural intervention for dysphagia in acute stroke: a randomised controlled trial. Lancet Neurol 5:31–37
Chung CS, Caplan LR, Yamamoto Y, Chang HM, Lee SJ, Song HJ, Lee HS, Shin HK, Yoo KM (2000) Striatocapsular haemorrhage. Brain 123(Pt 9):1850–1862
Cola MG, Daniels SK, Corey DM, Lemen LC, Romero M, Foundas AL (2010) Relevance of subcortical stroke in dysphagia. Stroke 41:482–486
Davalos A, Ricart W, Gonzalez-Huix F, Soler S, Marrugat J, Molins A, Suner R, Genis D (1996) Effect of malnutrition after acute stroke on clinical outcome. Stroke 27:1028–1032
Dennis M (2000) Nutrition after stroke. Br Med Bull 56:466–475
Dennis MS (2003) Outcome after brain haemorrhage. Cerebrovasc Dis 16(Suppl 1):9–13
Ding R, Logemann JA (2000) Pneumonia in stroke patients: a retrospective study. Dysphagia 15:51–57
Dziewas R, Ritter M, Schilling M, Konrad C, Oelenberg S, Nabavi DG, Stogbauer F, Ringelstein EB, Ludemann P (2004) Pneumonia in acute stroke patients fed by nasogastric tube. J Neurol Neurosurg Psychiatry 75:852–856
Dziewas R, Warnecke T, Olenberg S, Teismann I, Zimmermann J, Kramer C, Ritter M, Ringelstein EB, Schabitz WR (2008) Towards a basic endoscopic assessment of swallowing in acute stroke—development and evaluation of a simple dysphagia score. Cerebrovasc Dis 26:41–47
Elijovich L, Patel PV, Hemphill JC 3rd (2008) Intracerebral hemorrhage. Semin Neurol 28:657–667
Elmstahl S, Bulow M, Ekberg O, Petersson M, Tegner H (1999) Treatment of dysphagia improves nutritional conditions in stroke patients. Dysphagia 14:61–66
Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, Pedace C, Lenzi L (2009) Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis 18:329–335
Finestone HM, Greene-Finestone LS, Wilson ES, Teasell RW (1995) Malnutrition in stroke patients on the rehabilitation service and at follow-up: prevalence and predictors. Arch Phys Med Rehabil 76:310–316
Finestone HM, Woodbury MG, Foley NC, Teasell RW, Greene-Finestone LS (2002) Tracking clinical improvement of swallowing disorders after stroke. J Stroke Cerebrovasc Dis 11:23–27
Foley N, Teasell R, Salter K, Kruger E, Martino R (2008) Dysphagia treatment post stroke: a systematic review of randomised controlled trials. Age Ageing 37:258–264
Gebel JM, Sila CA, Sloan MA, Granger CB, Weisenberger JP, Green CL, Topol EJ, Mahaffey KW (1998) Comparison of the ABC/2 estimation technique to computer-assisted volumetric analysis of intraparenchymal and subdural hematomas complicating the GUSTO-1 trial. Stroke 29:1799–1801
Ghika JA, Bogousslavsky J, Regli F (1990) Deep perforators from the carotid system. Template of the vascular territories. Arch Neurol 47:1097–1100
Gonzalez-Fernandez M, Kleinman JT, Ky PK, Palmer JB, Hillis AE (2008) Supratentorial regions of acute ischemia associated with clinically important swallowing disorders: a pilot study. Stroke 39:3022–3028
Hamdy S, Mikulis DJ, Crawley A, Xue S, Lau H, Henry S, Diamant NE (1999) Cortical activation during human volitional swallowing: an event-related fMRI study. Am J Physiol 277:G219–G225
Hamdy S, Rothwell JC, Brooks DJ, Bailey D, Aziz Q, Thompson DG (1999) Identification of the cerebral loci processing human swallowing with H2(15)O PET activation. J Neurophysiol 81:1917–1926
Han DS, Chang YC, Lu CH, Wang TG (2005) Comparison of disordered swallowing patterns in patients with recurrent cortical/subcortical stroke and first-time brainstem stroke. J Rehabil Med 37:189–191
Hinchey JA, Shephard T, Furie K, Smith D, Wang D, Tonn S, Stroke Practice Improvement Network Investigators (2005) Formal dysphagia screening protocols prevent pneumonia. Stroke 36:1972–1976
Ickenstein GW, Stein J, Ambrosi D, Goldstein R, Horn M, Bogdahn U (2005) Predictors of survival after severe dysphagic stroke. J Neurol 252:1510–1516
Kaji R (2001) Basal ganglia as a sensory gating devise for motor control. J Med Invest 48:142–146
Kiphuth IC, Kuramatsu JB, Lucking H, Kloska S, Schwab S, Huttner HB (2011) Predictive factors for percutaneous endoscopic gastrostomy in patients with spontaneous intracranial hemorrhage. Eur Neurol 65:32–38
Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M, Khoury J (1996) The ABCs of measuring intracerebral hemorrhage volumes. Stroke 27:1304–1305
Kwon M, Lee JH, Kim JS (2005) Dysphagia in unilateral medullary infarction: lateral vs medial lesions. Neurology 65:714–718
Langmore SE (2001) Endoscopic Evaluation and Treatment of Swallowing Disorders. Thieme, New York/Stuttgart
Langmore SE (2003) Evaluation of oropharyngeal dysphagia: which diagnostic tool is superior? Curr Opin Otolaryngol Head Neck Surg 11:485–489
Langmore SE, Schatz K, Olsen N (1988) Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia 2:216–219
Lim SH, Lieu PK, Phua SY, Seshadri R, Venketasubramanian N, Lee SH, Choo PW (2001) Accuracy of bedside clinical methods compared with fiberoptic endoscopic examination of swallowing (FEES) in determining the risk of aspiration in acute stroke patients. Dysphagia 16:1–6
Logemann JA, Shanahan T, Rademaker AW, Kahrilas PJ, Lazar R, Halper A (1993) Oropharyngeal swallowing after stroke in the left basal ganglion/internal capsule. Dysphagia 8:230–234
Mann G, Hankey GJ, Cameron D (1999) Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke 30:744–748
Mann G, Hankey GJ, Cameron D (2000) Swallowing disorders following acute stroke: prevalence and diagnostic accuracy. Cerebrovasc Dis 10:380–386
Martin RE, Goodyear BG, Gati JS, Menon RS (2001) Cerebral cortical representation of automatic and volitional swallowing in humans. J Neurophysiol 85:938–950
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R (2005) Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 36:2756–2763
Meng NH, Wang TG, Lien IN (2000) Dysphagia in patients with brainstem stroke: incidence and outcome. Am J Phys Med Rehabil 79:170–175
Minnerup J, Wersching H, Brokinkel B, Dziewas R, Heuschmann PU, Nabavi DG, Ringelstein EB, Schabitz WR, Ritter MA (2010) The impact of lesion location and lesion size on poststroke infection frequency. J Neurol Neurosurg Psychiatry 81:198–202
Mosier K, Bereznaya I (2001) Parallel cortical networks for volitional control of swallowing in humans. Exp Brain Res 140:280–289
Mosier K, Patel R, Liu WC, Kalnin A, Maldjian J, Baredes S (1999) Cortical representation of swallowing in normal adults: functional implications. Laryngoscope 109:1417–1423
Perlman AL, Booth BM, Grayhack JP (1994) Videofluoroscopic predictors of aspiration in patients with oropharyngeal dysphagia. Dysphagia 9:90–95
Power ML, Hamdy S, Goulermas JY, Tyrrell PJ, Turnbull I, Thompson DG (2009) Predicting aspiration after hemispheric stroke from timing measures of oropharyngeal bolus flow and laryngeal closure. Dysphagia 24:257–264
Qureshi AI, Tuhrim S, Broderick JP, Batjer HH, Hondo H, Hanley DF (2001) Spontaneous intracerebral hemorrhage. N Engl J Med 344:1450–1460
Ropper AH, Samuels MA (2009) Adams and Victor’s Principles of Neurology. McGraw Hill Medical, New York
Smithard DG, O’Neill PA, Parks C, Morris J (1996) Complications and outcome after acute stroke. Does dysphagia matter? Stroke 27:1200–1204
Smithard DG, Smeeton NC, Wolfe CD (2007) Long-term outcome after stroke: does dysphagia matter? Age Ageing 36:90–94
Steinhagen V, Grossmann A, Benecke R, Walter U (2009) Swallowing disturbance pattern relates to brain lesion location in acute stroke patients. Stroke 40:1903–1906
Suzuki M, Asada Y, Ito J, Hayashi K, Inoue H, Kitano H (2003) Activation of cerebellum and basal ganglia on volitional swallowing detected by functional magnetic resonance imaging. Dysphagia 18:71–77
Teasell R, Foley N, Fisher J, Finestone H (2002) The incidence, management, and complications of dysphagia in patients with medullary strokes admitted to a rehabilitation unit. Dysphagia 17:115–120
Walter U, Knoblich R, Steinhagen V, Donat M, Benecke R, Kloth A (2007) Predictors of pneumonia in acute stroke patients admitted to a neurological intensive care unit. J Neurol 254:1323–1329
Warnecke T, Oelenberg S, Teismann I, Hamacher C, Lohmann H, Ringelstein EB, Dziewas R (2010) Endoscopic characteristics and levodopa responsiveness of swallowing function in progressive supranuclear palsy. Mov Disord 25:1239–1245
Warnecke T, Ritter MA, Kroger B, Oelenberg S, Teismann I, Heuschmann PU, Ringelstein EB, Nabavi DG, Dziewas R (2009) Fiberoptic endoscopic Dysphagia severity scale predicts outcome after acute stroke. Cerebrovasc Dis 28:283–289
Warnecke T, Teismann I, Oelenberg S, Hamacher C, Ringelstein EB, Schabitz WR, Dziewas R (2009) The safety of fiberoptic endoscopic evaluation of swallowing in acute stroke patients. Stroke 40:482–486
Warnecke T, Teismann I, Oelenberg S, Hamacher C, Ringelstein EB, Schabitz WR, Dziewas R (2009) Towards a basic endoscopic evaluation of swallowing in acute stroke—identification of salient findings by the inexperienced examiner. BMC Med Educ 9:13
Wong EH, Pullicino PM, Benedict R (2001) Deep cerebral infarcts extending to the subinsular region. Stroke 32:2272–2277
Zald DH, Pardo JV (1999) The functional neuroanatomy of voluntary swallowing. Ann Neurol 46:281–286
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sonja Suntrup and Tobias Warnecke contributed equally to this work.
Rights and permissions
About this article
Cite this article
Suntrup, S., Warnecke, T., Kemmling, A. et al. Dysphagia in patients with acute striatocapsular hemorrhage. J Neurol 259, 93–99 (2012). https://doi.org/10.1007/s00415-011-6129-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6129-3