Abstract
Background
Studies about the influence of various factors on clinical therapy and course in acute coronary syndromes have shown that the outcome is related to admission time to the hospital, with an impaired prognosis in patients admitted out of regular working hours. However little is known about the impact of admission on weekend in hospitals with catheterisation laboratories.
Methods
We analyzed data of the prospective MITRA-PLUS registry of 11,516 patients with ST-elevation myocardial infarction (STEMI) admitted to hospitals with catheterization facilities for differences of in-hospital mortality between patients admitted during regular working hours, at night and on weekends.
Results
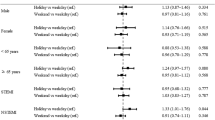
The prehospital delay and “door-to-balloon”-time were significantly longer on weekends and at nights than at regular working hours (median 196 Vs. 240 Vs. 155 min; P < 0.0001; 60 Vs. 84 min at weekends, resp. 75 min at nights; P < 0.0001). Reperfusion therapy was performed in 72.8% (8,248/11,332) patients, and there were less patients treated on weekend versus “on”-hours (69.7 Vs. 77 %, P < 0.0001). On weekends we found a significant higher in-hospital mortality (11.1 Vs. 9.4%, P = 0.01) and at night there was a trend to higher in-hospital mortality when compared with regular working hours (10.6 Vs. 9.4%, P = 0.07).
Conclusion
In patients with STEMI admitted to hospitals with catheterization facilities, admission during the “off”-hours is associated with higher in-hospital mortality. This may be due to lower rates of revascularization therapy and longer prehospital and in-hospital delays as compared to “on”-hours.
Similar content being viewed by others
References
Angeja BG, Gibson CM, Chin R, Frederick PD, Every NR, Ross AM, Stone GW, Barron HV (2002) Predictors of door-to-balloon delay in primary angioplasty. Am J Cardiol 89(10):1156–1161
Angleton P, Chandler WL, Schmer G (1989) Diurnal variation of tissue-type plasminogen activator and ist rapid inhibitor (PAI-I). Circulation 79:101–106
Assali AR, Brosh D, Vaknin-Assa H, Fuchs S, Teplitsky I, Sela O, Kornowski R (2006) The impact of circadian variation on outcomes in emergency acute anterior myocardial infarction percutaneous coronary intervention. Catheter Cardiovasc Interv 67(2):221–226
Bestehorn K (2005) Medical registries. Med Klin (Munich) 100(11):722–728
Bhalla A, Sachdev A, Lehl SS, Singh R, D’Cruz S (2006) Ageing and circadian variation in cardiovascular events. Singapore Med J 47(4):305–308
Bradley EH, Herrin J, Wang Y, Barton BA, Webster TR, Mattera JA, Roumanis SA, Curtis JP, Nallamothu BK, Magid DJ, McNamara RL, Parkosewich J, Loeb JM, Krumholz HM (2006) Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med 355:2308–2320
De Luca G, Suryapranata H, Ottervanger JP, van't Hof AW, Hoorntje JC, Gosselink AT, Dambrink JH, Zijlstra F, de Boer MJ (2005) Circadian variation in myocardial perfusion and mortality in patients with ST-segment elevation myocardial infarction treated by primary angioplasty. Am Heart J 150(6):1185–1189
D’Negri CE, Nicola-Siri L, Vigo DE, Girotti LA, Cardinali DP (2006) Circadian analysis of myocardial infarction incidence in an Argentine and Uruguayan population. BMC Cardiovasc Disord 6:1
Garot P, Juliard JM, Benamer H, Steg PG (1997) Are the results of primary PTCA for acute myocardial infarction different during the „off”hours? J Am Coll Cardiol 79:1527–1529
Giles T (2005) Relevance of blood pressure variation in the circadian onset of cardiovascular events. J Hypertens Suppl 23(1):S35–S39
Grimaudo V, Hauert J, Bachmann F, Kruithof EKO (1988) Diurnal variation of the fibrinolytic system. Thromb Haemost 59:495–499
Juliard JM, Himbert D, Golmard JL, Aubry P, Karrillon GJ, Boccara A, Benamer H, Steg PG (1997) Can we provide reperfusion therapy to all unselected patients admitted with acute myocardial infarction? J Am Coll Cardiol 30(1):157–164
Junker-Neff A, Eberle R, V Arnim T, Mehilli J, Hollweck R (2005) Is there an association between the sleep apnea syndrome and the circadian peak of myocardial infarction in the morning hours? Dtsch Med Wochenschr 130(49):2818–2822
Kentsch M, Rodemerk U, Ittel TH, Muller-Esch G, Mitusch R (2002) Day-night variability of the prehospital phase of acute myocardial infarct. Z Kardiol 91(8):637–641
Kostis WJ, Demissie K, Marcella SW, Shao Y-H, Wilson AC, Moreyra AE (2007) Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med 356(11):1099–1109
Morrow et al. (2000) TIMI risk score for ST-elevation myocardial infarction: a convenient, bedside, clinical score for risk assessment at presentation. An intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation 102:2031–2037
Schuster S, Koch A, Burczyk U, Schiele R, Wagner S, Zahn R, Glunz HG, Heinrich F, Stuby K, Berg G, et al. (1997) [Early treatment of acute myocardial infarction: implementation of therapy guidelines in routine clinical practice, MITRA pilot phase] Frühbehandlung des akuten Myokardinfarktes: Umsetzung von Therapierichtlinien in den klinischen Alltag, MITRA-Pilotphase. Z Kardiol 86:273–283
Silbergleit R, Kronick SL, Philpott S, Lowell MJ, Wagner C (2006) Quality of emergency care on the night shift. Acad Emerg Med 13(3):325–330
Wagner S, Schneider S, Schiele R, Fischer F, Dehn H, Grube R, Becker G, Baumgärtel B, Altmann E, Senges J (1999) Akuter Myokardinfarkt in Deutschland im Zeitraum zwischen 1996–1998: Therapie und hospitaler Verlauf. Ergebnisse des Myokardinfarktregisters (MIR) in Deutschland. [Acute myocardial infarction in Germany between 1996 and 1998: therapy and intrahospital course. Results of the myocardial infarction registry (MIR) in Germany]. Z Kardiol 88:857–867
Zahn R, Vogt A, Zeymer U, Gitt AK, Seidl K, Gottwik M, Weber MA, Niederer W, Modl B, Engel HJ, Tebbe U, Senges J (2005) In-hospital time to treatment of patients with acute ST elevation myocardial infarction treated with primary angioplasty determinants and outcome. Results from the registry of percutaneous coronary interventions in acute myocardial infarction of the Arbeitsgemeinschaft Leitender Kardiologischer Krankenhausärzte. Heart 91(8):1041–1046
Zahn R, Koch A, Rustige J, Schiele R, Wirtzfeld A, Neuhaus KL, Kuhn H, Gulker H, Senges J (1997) Primary angioplasty versus thrombolysis in the treatment of acute myocardial infarction. ALKK study group. Am J Cardiol 79(3):264–269
Zahn R, Schiele R, Schneider S, Gitt AK, Wienbergen H, Seidl K, Bossaller C, Buttner HJ, Gottwik M, Altmann E, Rosahl W, Senges J (2000) Decreasing hospital mortality between 1994 and 1998 in patients with acute myocardial infarction treated with primary angioplasty but not in patients treated with intravenous thrombolysis. Results from the pooled data of the maximal individual therapy in acute myocardial infarction (MITRA) registry and the myocardial infarction registry (MIR). J Am Coll Cardiol 36(7):2067–2071
Zahn R, Schweppe F, Zeymer U, Schiele R, Mark B, Frilling F, Gitt AK, Fraiture B, Gottwik M (2006) Einsatz der invasiven Diagnostik und Therapie bei konsekutiven unselektionierten NSTEMI- und STEMI-Patienten an einem Interventionszentrum. Herzmedizin 23:suppl 1 2
Zahn R, Schiele R, Seidl K, Bergmeier C, Schuster S, Hauptmann KE, Voigtlander T, Gottwik M, Glunz HG, Senges J, MITRA Study Group (1999) Primary angioplasty in acute myocardial infarction: differences between referred patients and those treated in hodpitals with on-site facilities? J Invasive Cardiol 11(4):213–219
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krüth, P., Zeymer, U., Gitt, A. et al. Influence of presentation at the weekend on treatment and outcome in ST-elevation myocardial infarction in hospitals with catheterization laboratories. Clin Res Cardiol 97, 742–747 (2008). https://doi.org/10.1007/s00392-008-0671-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-008-0671-8