Abstract
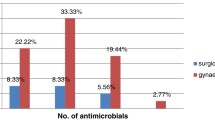
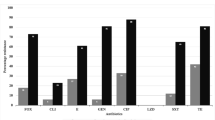
Over the past decade, methicillin-resistant Staphylococcus aureus (MRSA) has emerged as a global problem, prompting extensive surveillance efforts. A previous study of S. aureus isolates at our institution revealed alarming increases in the prevalence of MRSA with no sign of plateau. However, evidence of MRSA in pediatric surgical patients remains largely anecdotal, as there are no published reports of institutional MRSA surveillance in the pediatric surgical literature. We conducted a retrospective review of incision and drainage (I and D) procedures at our institution from 1998 through 2004. All I and D procedures performed at the University of Chicago Children’s Hospital were identified and the patients’ charts reviewed for pertinent information. A total of 99 I and D procedures were performed during the study period, ranging from 5 in 1998 to 32 in 2004. Among cultures with positive growth, 52 (65.8%) were MRSA, 14 (17.7%) were methicillin-sensitive S. aureus, and 13 (16.5%) were miscellaneous species. The number of MRSA isolates increases from 2 in 1998 to 20 in 2004, the largest increase occurring during the last 3 years of the study. A large proportion of MRSA isolates were resistant to antimicrobials from other classes, with over 70% being resistant to both erythromycin and cefazolin. A majority of MRSA isolates (71.4%) were obtained from patients with no record of prior hospitalization. Our analysis confirms a high prevalence of MRSA among soft-tissue infections requiring surgical drainage. In addition, a majority of MRSA isolates were resistant to multiple antimicrobials and were isolated from children without a previous documented exposure to the hospital milieu. Thus, pediatric surgeons should be aware of MRSA prevalence and resistance patterns in the local communities.




Similar content being viewed by others
References
Fluit AC, Wielders CL, Verhoef J, Schmitz FJ (2001) Epidemiology and susceptibility of 3,051 Staphylococcus aureus isolates from 25 university hospitals participating in the European SENTRY study. J Clin Microbiol 39:3727–3732
Madani TA, Al-Abdullah NA, Al-Sanousi AA, Ghabrah TM, Afandi SZ, Bajunid HA (2001) Methicillin-resistant Staphylococcus aureus in two tertiary-care centers in Jeddah, Saudi Arabia. Infect Control Hosp Epidemiol 22:211–216
Riley TV, Rouse IL (1995) Methicillin-resistant Staphylococcus aureus in Western Australia, 1983–1992. J Hosp Infect 29:177–188
Petinaki E, Miriagou V, Tzouvelekis LS, Pournaras S, Hatzi F, Kontos F, Maniati M, Maniatis AN (2001) Methicillin-resistant Staphylococcus aureus in the hospitals of central Greece. Int J Antimicrob Agents 18:61–65
Simor AE, Ofner-Agostini M, Bryce E, Green K, McGeer A, Mulvey M, Paton S (2001) The evolution of methicillin-resistant Staphylococcus aureus in Canadian hospitals: 5 years of national surveillance. CMAJ 165:21–26
Witte W, Braulke C, Cuny C, Heuck D, Kresken M (2001) Changing pattern of antibiotic resistance in methicillin-resistant Staphylococcus aureus from German hospitals. Infect Control Hosp Epidemiol 22:683–686
Seal JB, Moreira B, Bethel CD, Daum RS (2003) Antimicrobial resistance in Staphylococcus aureus at the University of Chicago Hospitals: a 15-year longitudinal assessment in a large university-based hospital. Infect Control Hosp Epidemiol 24:403–408
Herold BC, Immergluck LC, Maranan MC, Lauderdale DS, Gaskin RE, Boyle-Vavra S, Leitch CD, Daum RS (1998) Community-acquired methicillin-resistant Staphylococcus aureus in children with no identified predisposing risk. JAMA 279:593–598
Fridkin SK, Hageman JC, Morrison M, Sanza LT, Como-Sabetti K, Jernigan JA, Harriman K, Harrison LH, Lynfield R, Farley MM (2005) Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med 352:1436–1444
Orrett FA (1999) Methicillin resistance among Trinidadian isolates of community and hospital strains of Staphylococcus aureus and their patterns of resistance to non-beta-lactam antibiotics. Jpn J Infect Dis 52:238–241
Morgan M, Evans-Williams D, Salmon R, Hosein I, Looker DN, Howard A (2000) The population impact of MRSA in a country: the national survey of MRSA in Wales, 1997. J Hosp Infect 44:227–239
Prevention CfDCa (2002) Staphylococcus aureus resistant to vancomycin: United States, 2002. MMWR 51:565–567
Prevention CfDCa (2002) Vancomycin-resistant Staphylococcus aureus: Pennsylvania, 2002. MMWR 51:902
Tsiodras S, Gold HS, Sakoulas G, Eliopoulos GM, Wennersten C, Venkataraman L, Moellering RC, Ferraro MJ (2001) Linezolid resistance in a clinical isolate of Staphylococcus aureus. Lancet 358:207–208
Daum RS, Seal JB (2001) Evolving antimicrobial chemotherapy for Staphylococcus aureus infections: our backs to the wall. Crit Care Med 29:N92–N96
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seal, J., Glynn, L., Statter, M. et al. A high prevalence of methicillin-resistant Staphylococcus aureus among surgically drained soft-tissue infections in pediatric patients. Pediatr Surg Int 22, 683–687 (2006). https://doi.org/10.1007/s00383-006-1684-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-006-1684-x