Abstract
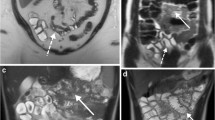
To assess the effect of the osmolarity for small bowel distension in MRI, ten volunteers ingested at two separate occasions negative oral contrast agents with different quantity and osmolarity: (1) a water solution combined with 2.0% sorbitol and 0.2% locus bean gum (LBG) with a quantity of 1500 ml and an osmolarity of 148 mOsmol/l, (2) a water solution combined with 2.0% sorbitol and 2.0% barium sulphate with a quantity of 1000 ml and an osmolarity of 194 mOsmol/l. Small bowel distension was quantified on coronal 2D-TrueFISP images by measuring the small bowel diameters. There were no statistically significant differences in mean small bowel diameter between both contrast agents. The mean small bowel distension was 19.2 mm after ingestion of 1500 ml of sorbitol-LBG solution and 19.0 mm after ingestion of 1000-ml sorbitol–barium sulphate solution. Furthermore, all volunteers found the ingestion of 1000-ml solution more pleasant than the 1500-ml solution. The ingestion of 1000 ml of sorbitol–barium sulphate solution led to a sufficient small bowel distension compared to 1500 ml of sorbitol–LBG solution. The side effect rate of both solutions was low. Based on these data, we recommend a quantity of 1000 ml of sorbitol–barium sulphate solution as an alternative for 1500-ml sorbitol–LBG solution for optimal bowel distension.






Similar content being viewed by others
References
Karlinger K, Györke T, Makö E, Mester A, Tarján Z (2000) The epidemiology and the pathogenesis of inflammatory bowel disease. Eur J Radiol 35:154–167
Gourtsoyiannis N, Papanikolaou N, Grammatikakis J, Prassopoulos P (2002) MR enteroclysis: technical considerations and clinical applications. Eur Radiol 12:2651–2658
Lauenstein TC, Schneemann H, Vogt FM, Herborn CU, Rühm SG, Debatin JF (2003) Optimization of oral contrast agents for MR imaging of the small bowel. Radiology 228:279–283
Maglinte DD, Gourtsoyiannis N, Rex D, Howard TJ, Kelvin FM (2003) Classification of small bowel Crohn’s subtypes based on multimodality imaging. Radiol Clin North Am 2:285–303
Schunk K, Kern A, Heussel CP, Kalden P, Mayer I, Orth T et al. (2000) Assessment of inflammatory activity in Crohn’s disease with hydro-MRI. RoFo Fortschr Geb Rontgenstrahlen Neuen Bildgeb Verfahr 2:153–160
Maglinte DD, Chernish SM, Kelvin FM (1992) Crohn disease of the small intestine: accuracy and relevance of enteroclysis. Radiology 184:541–545
Maglinte DD, Hall R, Miller RE, Chernish SM, Rosenak B, Elmore M et al. (1984) Detection of surgical lesions of the small bowel by enteroclysis. Am J Surg 147:225–229
Umschaden HW, Szolar D, Gasser J, Umschaden M, Haselbach H (2000) Small-bowel disease: comparison of MR enteroclysis images with conventional enteroclysis and surgical findings. Radiology 215:717–725
Antoch G, Kuehl H, Kanja J, Lauenstein TC, Schneemann H, Hauth E et al. (2004) Dual-modality PET/CT scanning with negative oral contrast agent to avoid artifacts: introduction and evaluation. Radiology 230:879–885
Ajaj W, Goehde SC, Schneemann H, Rühm SG, Debatin JF, Lauenstein TC (2003) Oral contrast agents for small bowel MRI: comparison of different additives to optimize bowel distension. Eur Radiol 14:458–464
Nakabayashi T, Mochiki E, Kamiyama Y, Haga N, Asao T, Kuwano H (2003) Erythromycin induces pyloric relaxation accompanied by a contraction of the gastric body after pylorus-preserving gastrectomy. Surgery 133:647–655
Stacher G, Peeters TL, Bergmann H, Wiesnagrotzki S, Schneider C, Granser-Vacariu GV et al. (1993) Erythromycin effects on gastric emptying, antral motility and plasma motilin and pancreatic polypeptide concentrations in anorexia nervosa. Gut 34:166–172
Shia J, Teruya-Feldstein J, Pan D, Hegde A, Klimstra DS, Chaganti RS et al. (2002) Primary follicular lymphoma of the gastrointestinal tract: a clinical and pathologic study of 26 cases. Am J Surg Pathol 26:216–224
Kettritz U, Isaacs K, Warshauer DM, Semelka RC (1995) Crohn’s disease. Pilot study comparing MRI of the abdomen with clinical evaluation. J Clin Gastroenterol 3:249–253
Madsen SM, Thomsen HS, Munkholm P, Dorph S, Schlichting P (1998) Active Crohn’s disease and ulcerative colitis evaluated by low-field magnetic resonance imaging. Scand J Gastroenterol 11:1193–1200
Lomas DJ, Graves MJ (1999) Small bowel MRI using water as a contrast medium. Br J Radiol 72:994–997
Hänsel R, Sticher O, Steinegger E Pharmakognosy and phytopharmazy. Springer Verlag, Berlin Heidelberg New York
Nau R, Dreyhaupt T, Kolenda H, Prange HW (1992) Low blood-to-cerebrospinal fluid passage of sorbitol after intravenous infusion. Stroke 23:1276–1279
Hubbell JH (1982) Photon mass attenuation and energy-absorption coefficients from 1 keV to 20 MeV. Int J Appl Radiat Isot 33:1269–1290
Reimund JM, Jung-Chaigneau E, Chamouard P, Wittersheim C, Duclos B, Baumann R (1999) Diagnostic value of high resolution sonography in Crohn’s disease and ulcerative colitis. Gastroenterol Clin Biol 7:740–746
Lim JH, Ko YT, Lee DH, Lim JW, Kim TH (1994) Sonography of inflammatory bowel disease: findings and value in differential diagnosis. AJR Am J Roentgenol 2:343–347
Lew RJ, Ginsberg GG (2002) The role of endoscopic ultrasound in inflammatory bowel disease. Gastrointest Endosc Clin N Am 3:561–571
Borthne AS, Dormagen JB, Gjesdal KI, Storaas T, Lygren I, Geitung JT (2003) Bowel MR imaging with oral gastrografin: an experimental study with healthy volunteers. Eur Radiol 13:100–106
Narin B, Ajaj W, Gohde S et al. (2004) Combined small and large bowel MR imaging in patients with Crohn’s disease: a feasibility study. Eur Radiol 14:1535–1542
Gourtsoyiannis N, Papanikolaou N, Grammatikakis J, Maris T, Prassopoulos P (2001) MR enteroclysis protocol optimization: comparison between 3D FLASH with fat saturation after intravenous gadolinium injection and true FISP sequences. Eur Radiol 11:908–913
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ajaj, W., Goyen, M., Schneemann, H. et al. Oral contrast agents for small bowel distension in MRI: influence of the osmolarity for small bowel distention. Eur Radiol 15, 1400–1406 (2005). https://doi.org/10.1007/s00330-005-2711-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-005-2711-3