Abstract
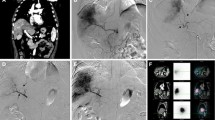
We evaluated the feasibility, safety, and efficacy of radioembolization (administered from one or two vascular points) after the redistribution of arterial blood flow in the liver in patients with hepatic neoplasms and arterial anatomic peculiarities (AAP). Twenty-four patients with liver neoplasms and AAP (graded according to Michel’s classification) were included in the study. During pretreatment angiographic planning, all extrahepatic vessels that could feed the tumor were embolized and the intrahepatic vessels occluded in order to redistribute blood flow. The distribution of microspheres was initially assessed by using technetium-99m-labeled macroaggregated albumin (99mTc-MAA) from one of two vascular points before the administration of yttrium-90 (90Y)-radiolabeled resin microspheres. Perfusion of lesions situated in the redistributed segments (L-RS) and nonredistributed segments (L-NRS) were compared by assessing the distribution of 99mTc-MAA by SPECT/CT. Perfusion was graded as normal, reduced, or absent. 90Y resin microspheres were then injected from the same arterial sites as 99mTc-MAA and the tumor response recorded 3 months later. The tumor response in L-RS was compared with that in L-NRS and graded as better, similar, or worse. Among 11 patients with type I AAP in whom mainly vessels in segments I–III or IV were occluded, perfusion of L-RS was graded as similar (n = 7) or reduced (n = 4). Among the remaining 13 patients with AAP types III (n = 3), V (n = 4), VIII (n = 3), and others (n = 3) in which aberrant arteries were occluded, perfusion of L-RS was graded as similar (n = 9), reduced (n = 3), or absent (n = 1). Overall, 99mTc-MAA was present in the L-RS of 95.8% patients and the distribution of 99mTc-MAA in L-RS and L-NRS were graded as similar in 66.6% of patients. Compared with lesions in the L-NRS, tumor response in L-RS was similar in 23 cases and worse in 1 case. No complications were recorded after the administration of 90Y resin microspheres. Redistribution of flow in L-RS is feasible and enables a safe and effective delivery of 90Y resin microspheres that are able to be distributed via intrahepatic collaterals and access the microvasculature of L-RS.



Similar content being viewed by others
References
King J, Quinn R, Glenn DM et al (2008) Radio-embolization with selective internal microspheres for neuroendocrine liver metastases. Cancer 113:921–929
Sato KT, Lewandowski RJ, Mulcahy MF et al (2008) Unresectable chemorefractory liver metastases: radio-embolization with 90Y microspheres Safety, efficacy and survival. Radiology 247:507–515
Sangro B, Bilbao JI, Boan J et al (2006) Radio-embolization using 90-Y resin microspheres for patients with advanced hepatocellular carcinoma. Int J Radiat Oncol Biol Phys 66:792–800
Ibrahim SM, Lewandowski RJ, Sato KT et al (2008) Radio-embolization for the treatment of unresectable hepatocellular carcinoma: a clinical review. World J Gastroenterol 14:1664–1669
Kennedy A, Nag S, Salem R et al (2007) Recommendations for radio-embolization of hepatic malignancies using yttrium-90 microsphere brachytherapy: a consensus panel report from the Radio-embolization Brachytherapy Oncology Consortium (REBOC). Int J Radiat Oncol Biol Phys 68:13–23
Arai Y, Yakeuchi Y, Inaba Y et al (2007) Percutaneous catheter placement for hepatic arterial infusion chemotherapy. Tech Vasc Interv Radiol 10:30–37
Ganeshan A, Upponi S, Hon LQ, Warakaulle D, Uberoi R (2008) Arterial infusion of chemotherapy: the role of diagnostic and interventional radiology. Ann Oncol 19:847–851
Tanaka T, Arai Y, Inaba Y et al (2003) Radiologic placement of side-hole catheter with tip fixation for hepatic arerial infusion chemotherapy. J Vasc Inter Radiol 14:63–68
Bledin AG, Kim EE, Chuang VP, Wallace S, Haynie TP (1984) Changes of arterial blood flow patterns during infusion chemotherapy, as monitored by intra-arterially injected technetium 99 macroaggregated albumin. Br J Radiol 57:197–203
Ikeda O, Tamura Y, Nakasone Y et al (2007) Evaluation of intrahepatic perfusion on fusion imaging using a combined CT/SPECT system: influence of anatomic variations on hemodynamic modification before installation of implantable port systems for hepatic arterial infusion chemotherapy. Cardiovasc Intervent Radiol 30:383–391
Hiatt JR, Gabbay J, Busuttil RW (1994) Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg 220:50–52
Ikeda O, Kusunoki S, Nakaura T et al (2006) Evaluation of intrahepatic perfusion Comparison of fusion imaging using a combined CT/SPECT system and intra-arterial CT: assesment of drug distribution by an implantable port systems in patients undergoing hepatic arterial infusion chemotherapy. Cardiovasc Intervent Radiol 29:371–379
Redman HC, Reuter SR (1970) Arterial collaterals in the liver hilus. Radiology 94:575–579
Chuang VP, Wallace S (1980) Hepatic arterial redistribution for intraarterial infusion of hepatic neoplasms. Radiology 135:295–299
Charnsangavej C, Chuang VP, Wallace S, Soo CS, Bowers T (1982) Angiographic classification of hepatic arterial collaterals. Radiology 144:485–494
Cho A, Gunji H, Koike N et al (2007) Intersegmental arterial communication between the medial and left lateral segments of the liver. Dig Surg 24:328–330
Gunji H, Cho A, Tohma T et al (2006) The blood supply of the hilar bile duct and its relationship to the communicating arcade located between the right and left hepatic arteries. Am J Surg 192:276–280
Tohma T, Cho A, Okazumi S et al (2005) Communicating arcade between the right and left hepatic arteries: evaluation with CT and angiography during temporary balloon occlusion of the right or left hepatic artery. Radiology 237:361–365
Miyazaki M, Ito H, Nkagawa K et al (2000) Unilateral hepatic artery reconstruction is unnecessary in biliary tract carcinomas involving lobar hepatic artery: implications of interlobar hepatic artery and its preservation. Hepatogastroenterology 47:1526–1530
Onishi H, Kawarada Y, Das BC et al (2000) Surgical anatomy of the medial segment (S4) of the liver with special reference to bile ducts and vessels. Hepatogastroenterology 47:143–150
Saad WE, Davies MG, Darcy MD (2008) Management of bleeding after percutaneous transhepatic cholangiography or transhepatic biliary drain placement. Tech Vasc Interv Radiol 11:60–71
Lewandowski RJ, Sato KT, Atassi B et al (2007) Radio-embolization with 90Y microspheres: angiographic and technical considerations. Cardiovasc Intervent Radiol 30:571–592
Cosin O, Bilbao JI, Alvarez S et al (2007) Right gastric artery embolization prior to treatment with yttrium-90 microspheres. Cardiovasc Intervent Radiol 30:98–103
Sebastian AJ, Szyszko T, Al-Nahhas A, Nijran K, Tait NP (2008) Evaluation of hepatic angiography procedures and bremsstrahlung imaging in selective internal radiation therapy: a two-year single-center experience. Cardiovasc Intervent Radiol 31:643–649
Bilbao JI, Díaz-Dorronsoro L, De Luis E et al (2009) Biocompatibility, inflammatory response and recanalization characteristics of non-radioactive resin microspheres: histological findings. Cardiovasc Intervent Radiol 32:727–736
Sone M, Kato K, Hirose A et al (2008) Impact of multislice CT angiography of radiological catheter placement for hepatic arterial infusion chemotherapy. Cardiovasc Intervent Radiol 31:91–97
Wallace MJ, Murthy R, Kammat PP et al (2007) Impact of C-arm CT on hepatic arterial interventions for hepatic malignancies. J Vasc Interv Radiol 18:1500–1507
Gaba RC, Wang D, Lewandowski RJ et al (2008) Four-dimensional transcatheter intraarterial perfusion MR imaging for monitoring chemoembolization of hepatocellular carcinoma: preliminary results. J Vasc Interv Radiol 19:1589–1595
Ho S, Lau WY, Leung TW, Chan M, Chan K, Lee WY et al (1997) Tumour-to-normal uptake ratio of 90Y microspheres in hepatic cancer assessed with 99Tc macroaggregated albumin. Br J Radiol 70(836):823–828
Ho S, Lau WY, Leung TW, Chan M, Johnson PJ, Li AK (1997) Clinical evaluation of the partition model for estimating radiation doses from yttrium-90 microspheres in the treatment of hepatic cancer. Eur J Nucl Med 24(3):293–298
Koch W, Tastch K (2008) Nuclear medicine procedures for treatment evaluation. In: Bilbao JI, Reiser MF (eds) Liver radioembolization with 90Y microspheres. Springer, New York, pp 75–91
Boan JF, Valero M, Arbizu J (2008) Improving treatment design by image fusion techniques. In: Bilbao JI, Reiser MF (eds) Liver radioembolization with 90Y microspheres. Springer, New York, pp 61–73
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bilbao, J.I., Garrastachu, P., Herráiz, M.J. et al. Safety and Efficacy Assessment of Flow Redistribution by Occlusion of Intrahepatic Vessels Prior to Radioembolization in the Treatment of Liver Tumors. Cardiovasc Intervent Radiol 33, 523–531 (2010). https://doi.org/10.1007/s00270-009-9717-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-009-9717-1