Abstract
Introduction
Papillary thyroid carcinoma (PTC) patients show a high rate of cervical lymphatic metastasis. However, there are no universal binding guidelines for the extent of lateral cervical lymph node dissection (LND) in such cases. In particular, the need for LND above the spinal accessory nerve (SAN) remains controversial. The present study examined whether level IIb lymph node (LN) dissection is always necessary in PTC patients with lateral cervical LN metastasis.
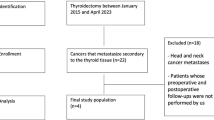
Materials and Methods
The study prospectively examined 167 PTC patients with lateral cervical LN metastasis who underwent modified radical neck dissection (MRND) in our institution from November 2005 to March 2007. The MRND was bilateral in 24 cases. All patients underwent level II, III, IV, and V LND. Levels IIa and IIb LNs were individually dissected in all cases. All LND was performed using strict leveling criteria by a single operating team. The patterns of lymphatic metastasis and potential risk factors for level IIb LN involvement were evaluated.
Results
The most common site of metastasis was level III (80.6% of cases), followed by level IV (74.9%) and II (55.5%). The metastasis rates in level IIa and IIb were 55.5% and 6.8%, respectively; all level IIb LN metastasis was accompanied by level IIa metastasis (p = 0.001). In addition, level IIb LN metastasis was found to be associated with the aggressiveness of lymphatic metastasis (i.e., the total number of metastatic LNs) (p < 0.0001).
Conclusions
A level IIb LND should be performed when there is clinical or radiological evidence of lymphatic metastasis. In the absence of such evidence, the findings suggest that level IIb LND is not necessary in N1b PTC patients when there is no level IIa LN metastasis, or when the metastasis is not aggressive.

Similar content being viewed by others
References
Kebebew E, Clark OH (2000) Differentiated thyroid cancer: “complete” rational approach. World J Surg 24:942–951
Bhattacharyya N (2003) Surgical treatment of cervical nodal metastases in patients with papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 129:1101–1104
McConahey WM, Hay ID, Woolner LB et al. (1986) Papillary thyroid cancer treated at the Mayo Clinic, 1946 through 1970: initial manifestations, pathologic finding, therapy, and outcome. Mayo Clin Proc 61:978–996
Mazzaferri EL (1987) Papillary thyroid carcinoma: factors influencing prognosis and current therapy. Semin Oncol 14:315–332
Akslen LA (1993) Prognostic importance of histologic grading in papillary thyroid carcinoma. Cancer 72:2680–2685
Moley JF, Wells SA (1999) Compartment-mediated dissection for papillary thyroid cancer. Langenbecks Arch Surg 384:9–15
Bhattacharyya N (2003) A population-based analysis of survival factors in differentiated and medullary thyroid carcinoma. Otolaryngol Head Neck Surg 128:115–123
Ozaki O, Ito K, Kobayashi K et al. (1998) Modified neck dissection for patients with nonadvanced, differentiated carcinoma of the thyroid. World J Surg 12:825–829
Noguchi M, Kumaki T, Taniya T et al. (1990) Bilateral cervical lymph node metastases in well-differentiated thyroid cancer. Arch Surg 125:804–806
Clark OH, Duh QY (1991) Thyroid cancer. Med Clin North Am 75:211–234
Lee KY, Lore JM Jr (1990) The treatment of metastatic thyroid disease. Otolaryngol Clin North Am 23:475–493
Nahum AM, Mullally W, Marmor L (1961) A syndrome resulting from radical neck dissection. Arch Otolaryngol 74:424–428
Dijkstra PU, van Wilgen PC, Buijs RP et al. (2001) Incidence of shoulder pain after neck dissection: a clinical explorative study for risk factors. Head Neck 23:947–953
Cheong PT, Hao SP, Lin YH et al. (2000) Objective comparison of shoulder dysfunction after three neck dissection techniques. Ann Otol Rhinol Laryngol 109:761–766
Patel KN, Shah JP (2005) Neck dissection: past, present, future. Surg Oncol Clin North Am 14:461–477
Chone CT, Crespo AN, Rezende AS et al. (2000) Neck lymph node metastases to the posterior triangle apex: Evaluation of clinical and histopathological risk factors. Head Neck 22:564–571
Talmi YP, Hoffman HT, Horowitz Z et al. (1998) Patterns of metastases to the upper jugular lymph nodes (the “submuscular recess”). Head Neck 20:682–686
Kupferman ME, Patterson M, Mandel SJ et al. (2004) Patterns of lateral neck metastasis in papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 130:857–860
Caron NR, Tan YY, Ogilvie JB et al. (2006) Selective modified radical neck dissection for papillary thyroid cancer–is level I, II, and V dissection always necessary? World J Surg 30:833–840
Sivanandan R, Soo KC (2001) Pattern of cervical lymph node metastases from papillary carcinoma of the thyroid. Br J Surg 88:1241–1244
Shah JP (1990) Cervical lymph node metastases—diagnostic, therapeutic and prognostic implications. Oncology (Williston Park) 4:61–69
Leon X, Quer M, Orus C et al. (2001) Selective dissection of levels II–III with intraoperative control of the upper and middle jugular nodes: a therapeutic option for the N0 neck. Head Neck 23:441–446
Corlette TH, Cole IE, Albsoul N et al. (2005) Neck dissection of level IIB: is it really necessary? Laryngoscope 115:1624–1626
Shaha AR (2004) Prognostic factors in papillary thyroid carcinoma and implications of large nodal metastasis. Surgery 135:237–239
Musacchio MJ, Kim AW, Vijungco JD et al. (2003) Greater local recurrence occurs with “berry picking” than neck dissection in thyroid cancer. Am Surg 69:191–196
Pingpank JF Jr, Sasson AR, Hanlon AL et al. (2002) Tumor above the spinal accessory nerve in papillary thyroid cancer that involves lateral neck nodes. Arch Otolaryngol Head Neck Surg 128:1275–1278
Patten C, Hillel A (1993) The 11th nerve syndrome. Accessory nerve palsy or adhesive capsulitis? Arch Otolaryngol Head Neck Surg 119:215–220
Cappiello J, Piazza C, Guidice M et al. (2005) Shoulder disability after diffenent selective neck dissections (levels II–IV versus levels II–V): a comparative study. Laryngoscope 115:259–263
Kuntz AL, Weymuller EA Jr (1999) Impact of neck dissection on quality of life. Laryngoscope 109:1334–1338
Short SO, Kaplan JN, Laramore GE et al. (1984) Shoulder pain and function after neck dissection with or without preservation of the spinal accessory nerve. Am J Surg 148:478–482
Bocca E, Pignataro O, Sasaki CT (1980) Functional neck dissection: a description of operative technique. Arch Otolaryngol 106:524–527
Shah S, Har-EI G, Rosenfeld RM (2001) Short-term and long-term quality of life after neck dissection. Head Neck 23:954–961
Sobol S, Jensen C, Sawyer W et al. (1985) Objective comparison of physical dysfunction after neck dissection. Am J Surg 150:503–509
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, J., Sung, TY., Nam, KH. et al. Is Level IIb Lymph Node Dissection Always Necessary in N1b Papillary Thyroid Carcinoma Patients?. World J Surg 32, 716–721 (2008). https://doi.org/10.1007/s00268-007-9381-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9381-z