Abstract
Therapeutic targeting of melanoma antigens frequently focuses on the melanocyte differentiation or cancer-testis families. Antigen-loss variants can often result, as these antigens are not critical for tumor cell survival. Exploration of functionally relevant targets has been limited. The melanoma inhibitor of apoptosis protein (ML-IAP; livin) is overexpressed in melanoma, contributing to disease progression and treatment resistance. Improved understanding of the significance of ML-IAP immune responses in patients has possible therapeutic applications. We found ML-IAP frequently expressed in melanoma metastases by immunohistochemistry. To assess spontaneous immunity to ML-IAP, an overlapping peptide library representing full-length protein was utilized to screen cellular responses in stage I–IV patients and healthy controls by ELISPOT. A broad array of CD4+ and CD8+ cellular responses against ML-IAP was observed with novel class I and class II epitopes identified. Specific HLA-A*0201 epitopes were analyzed further for frequency of reactivity. The generation of specific CD4+ and cytotoxic T cells revealed potent functional capability including cytokine responsiveness to melanoma cell lines and tumor cell killing. In addition, recombinant ML-IAP protein used in an ELISA demonstrated high titer antibody responses in a subset of patients. Several melanoma patients who received CTLA-4 blockade with ipilimumab developed augmented humoral immune responses to ML-IAP as a function of treatment which was associated with beneficial clinical outcomes. High frequency immune responses in melanoma patients, associations with favorable treatment outcomes, and its essential role in melanoma pathogenesis support the development of ML-IAP as a disease marker and therapeutic target.
Similar content being viewed by others
Introduction
Many melanoma antigens have been identified that are the targets of both cellular and humoral immune responses. The melanocyte differentiation antigens expressed in both melanomas and normal melanocytes have been extensively studied as both the targets of spontaneous immune responses as well as utilized in strategies to augment immunity with therapeutic intent [1]. In addition, the cancer-testis antigens, such as MAGE [2, 3] and NY-ESO-1 [4, 5], have been evaluated in a similar manner. Cancer-testis antigens present attractive therapeutic targets as their expression is limited to a subset of melanomas and they are not expressed in normal tissues other than the germ cells of testes, placenta, and fetal ovary. Strategies to therapeutically target these classes of antigens frequently lead to antigen-loss variants [6–12] and progression of disease. An important goal in cancer therapeutics, therefore, is the identification of antigens that will less likely result in antigen-loss variants due to their essential role in melanoma pathogenesis. Some defined melanoma antigens such as β-catenin [13] have been linked to function. Further exploration of functionally relevant antigen targets for melanoma has potential clinical applications.
The inhibitor of apoptosis (IAP) family of proteins represents key regulators of apoptosis that function through the prevention of caspase activation [14] and the regulation of TNF signaling. The IAPs are frequently over expressed in a number of cancers, and their expression is increased by tumor cells in response to chemotherapy or radiation [15]. Specifically, the melanoma inhibitor of apoptosis protein (ML-IAP; livin) is strongly expressed in a variety of human cancers including melanoma [16–18], but has limited expression in normal adult tissues [19–21]. The high expression of ML-IAP in tumors has been associated with a poor prognosis. Expression of ML-IAP has been shown to provide apoptosis resistance in non-small cell lung cancer cells [21] and melanoma.
ML-IAP binds caspases 3, 7, and 9, and may function as a SMAC sink, resulting in the blockade of the death receptor and mitochondria based apoptotic pathways [22, 23]. The BIR domain of ML-IAP contains an evolutionary conserved sequence that is required for its anti-apoptotic activity. In this way, ML-IAP offers melanoma cells a distinct survival advantage during tumor progression as well as a mechanism for resistance to chemotherapy, radiation, and hypoxic conditions [24]. The downregulation of ML-IAP in various preclinical models leads to increased apoptosis, reduced tumor cell growth, and sensitization to chemotherapy [25].
ML-IAP has previously been identified as a target of immune-mediated tumor destruction in patients receiving vaccination with autologous, irradiated melanoma cells engineered to secrete granulocyte–macrophage colony stimulating factor (GM-CSF) [26]. In addition, spontaneous cytotoxic T lymphocyte (CTL) responses to ML-IAP epitopes have been found in melanoma patients and a limited number of healthy controls [27]. In the current study, we utilized a library of overlapping peptides to screen for T cell responses by ELISPOT in stage I–IV melanoma patients as well as normal donors, thus not limiting our assessment to a particular haplotype. Humoral immune responses were assessed utilizing recombinant ML-IAP protein in an ELISA. Spontaneous immune responses to ML-IAP in melanoma patients demonstrate both specific cellular and humoral activity as well as correlations with favorable clinical outcomes.
Materials and methods
Tissues and sera
Tumor and peripheral blood samples were obtained from patients on Dana-Farber/Harvard Cancer Center Institutional Review Board approved protocols. Tumor cell lines were established from harvested fresh tissues that underwent mechanical and enzymatic digestion and in vitro expansion. Cell cultures were maintained in Dulbecco’s modified Eagle medium containing 10% (vol/vol) fetal calf serum (FCS) and penicillin/streptomycin. Peripheral blood was collected in heparinized tubes from normal donors and patients diagnosed with stages I–IV melanoma. Peripheral blood mononuclear cells (PBMC) were isolated by gradient centrifugation using Ficoll-Paque Plus (GE Healthcare Bio-Sciences, Piscataway, NJ).
Immunohistochemical analysis and scoring
All specimens were standard, formalin-fixed, paraffin-embedded tissue blocks for morphological analysis. Hemotoxylin-eosin stained sections of each lesion were reviewed to verify the diagnosis and assess the presence of representative lesional material. For patients who had peripheral blood obtained for immune analyses, blocks of metastatic visceral deposits were available for immunohistochemical analysis in eight cases. This was performed utilizing a ML-IAP specific antibody as previously described [26]. Mouse IgG1 (BD biosciences, cat#: 557273) was used as a control. The extent of ML-IAP expression in tumor cells was estimated microscopically by two pathologists who were blinded to the patient’s data and graded as follows: negative (0%); + (<20%); ++ (20–60%); and +++ (>60%).
ELISPOT assay
For T cell stimulation, 1 × 106 PBMC were initially cultured with 1 μg/ml of each peptide in overlapping peptide pools or 10 μg/ml single peptide in the presence of 10 U/ml IL-2 (BD Biosciences) for 1 week. For ELISPOT analyses, 5 × 104 cells/well were placed on a 96-well plate (Millipore, Bedford, MA) pre-coated with anti-γ-IFN Ab (Mabtech, Cincinnati, OH). These cells were restimulated with the same peptides at 10 μg/ml and autologous PBMC overnight. The plates were washed and probed with biotinylated anti-γ-IFN Ab and streptovidin-ALP (Mabtech). γ-IFN spots were developed with NBT and BCIP (Promega, Madison, WI), and counted using an Immunospot reader (C.T.L. Cellular Technololgy Ltd, Shaker Heights, Ohio). Samples were performed in duplicate. The HIV peptide L11 (LLFGYPVYV) was utilized as a control. For determination of CD4+ and CD8+ T cell responses to individual peptides (>90% purity), peptide-pretreated PBMC were incubated with either CD4 or CD8 microbeads (MiltenyiBiotech, Auburn, CA). Cells were depleted of either CD4+ or CD8+ T cells through MACS separation columns (MiltenyiBiotech) and were then stimulated with the same peptides for ELISPOT analysis. To analyze HLA-A*0201 reactivity in melanoma patients and normal donors, ML-IAP peptides I280, JS90, and I237 were used. HLA-A*0201 peptides for flu(GILGFVFTL) and MART-1(EAAGIGILTV) were utilized for comparisons.
Generation of antigen-specific CTL
To determine the HLA status from donor blood, PBMC were first stained with fluorescence conjugated anti-HLA-A2 Ab (BB7.2) (AbD serotec, Oxford, UK), and analyzed by flow cytometry. Genotyping for HLA-A2 and DR alleles were performed by the American Red Cross by PCR amplification with sequence-specific primers and sequence-based typing. For HLA-A*0201 peptide reactivity, T2 cells were grown in RPMI 1640 supplemented with 10% FCS and utilized in ELISPOT.
Generation of autologous activated B cells for peptide presentation was performed as previously described [28]. Briefly, NIH 3T3-CD40L cells are stably transfected with CD40 ligand expression vector to express CD40 ligand and were maintained in F12/DMEM supplemented with 10% FCS and 400 μg/ml G418. PBMC were cocultured with irradiated (96 Gy) NIH 3T3-CD40L cells in the presence of 10 ng/ml IL-4 (R&D Systems, Minneapolis, MN) and 0.55 μM cyclosporine A (Sigma, St. Louis, MO) for 3–5 days. Activated B cells were maintained by coculture with NIH 3T3 CD40L cells in Iscove’s Modified Dulbecco’s Medium (IMDM) supplemented with 10% FCS and 10 ng/ml IL-4. CD8+ T cells were isolated by positive selection using microbeads (MiltenyiBiotech). Epitope-specific T cells were stimulated in the presence of 10 U/ml IL-2 with autologous activated B cells that have been pulsed with relevant peptide (New England Peptide, Gardner, MA) and irradiated (32 Gy). Manufactured T cells were cultured in RPMI 1,640 supplemented with 10% human AB sera (Mediatech, Herndon, VA) and 100 U/ml IL-2. After two to four rounds of stimulation, phenotypic and functional analyses of the CD8+ T cells were performed. For generation of peptide-specific CD4 T cells, patient PBMCs were treated with 10 μg/ml peptide in the presence of 10 U/ml of IL2 for 1 week. Isolated CD4+ T cells were restimulated with irradiated autologous PBMCs in the presence of 10 μg/ml. The CD4+ or CD8+ T cell cultures were further enriched by IFN-γ selection (MiltenyiBiotech), expanded and maintained with irradiated PBMC (32 Gy), 1% PHA (Invitrogen, Carlsbad, CA), and 100 U/ml IL-2.
Proliferation assay
1 × 104 cells/well T cells were cocultured with 2 × 104 irradiated melanoma lines for 2 days, and further pulsed with [3H]thymidine (0.5 μCi H3/well) overnight. The incorporated radioactivity was measured in a liquid scintillation counter.
Cytotoxic activity assay
Functional activities of antigen-specific cytotoxic T lymphocytes (CTL) were further analyzed with a DELFIA® cell cytotoxicity kit (PerkinElmer, Waltham, MA) according to manufacturer’s instructions. Briefly, 1 × 106 T2 cells or melanoma cell lines as target cells were labeled with 5 μl DATDA for 30 min at 37°C. After washing, 5 × 103/well labeled cells were mixed with antigen-specific CTLs at the indicated ratio. Supernatants were counted in a Vector™ fluorescence plate reader (PerkinElmer). All assays were performed in duplicate. Percent cytotoxicity was defined as (sample-spontaneous release)/(total release-spontaneous release) × 100.
ELISA
Full-length MLIAP was cloned in frame into the pET-41b vector (Novagen, Gibbstown, NJ) and integrity of the construct verified by sequencing (molecular biology core facilities, Dana-Farber Cancer Institute). His-tagged ML-IAP protein was expressed in E. coli rosetta 2 (DE3) (Novagen, Gibbstown, NJ) with 0.1 mM IPTG for 2 h at 30°C and purified by affinity chromatography using HisTrap™ FF nickel columns (GE Healthcare Bio-Sciences, Piscataway, NJ), and further desalted using desalt columns (GE Healthcare Bio-Sciences). Purity of recombinant ML-IAP protein was confirmed by acrylamide electrophoresis, Coomassie blue staining, and Western blot as previously described [26]. Seventy-seven pmol recombinant his-tagged ML-IAP protein and LEHHHHHHHH peptide as a control were adsorbed in coating buffer (15 mM Na2CO3, 30 mM NaHCO3, pH 9.6) to Nunc-Immno-plates overnight at 4°C. Plates were then washed with PBS and blocked with 2% nonfat milk in PBS. The plates were again washed with PBS and 100 μl per well of sera (diluted 1:500 in 2% nonfat milk) were added and incubated overnight at 4°C. Plates were then extensively washed with PBS/Tween-20, and incubated with 100 μl per well of HRP conjugated goat anti-human IgG (H+L) Ab (Zymed, Carlsbad, CA) diluted 1:2000 in 2% nonfat milk for 1 h at room temperature. The plates were again extensively washed in PBS/Tween-20 and developed with the addition of 70 μl substrate (DAKO, Carpinteria, CA). The reactions were stopped with the addition of 35 μl of 1 N HCl. Plates were read at an optical density (O.D.) of 450 nm. All samples were performed in duplicate. Values were reported as the mean O.D. of the sample wells minus the mean O.D. from wells coated with tag peptide alone.
Statistical analysis
All ELISPOT samples and their negative controls were run in duplicate. The spots/well were counted using ImmunoSpot software Version 3 (Cellular Technology Ltd., Shaker Heights, Ohio, USA). To screen for cellular immune responses in stage I–IV melanoma patients, the mean number of spots in sets of overlapping peptides were compared with the mean number of spots in the negative controls using a two-sample T test. A minimum of 10 or more spots per well was required for the peptides and at least 3 times more spots in the peptides than in the controls. A set of peptides was considered for further study if the probability was less than 10% that the average number of spots in the peptide group was equal to the average number in the control. Individual peptides were compared with controls using similar methodology.
Antibody titers of ML-IAP by ELISA were compared for melanoma patients and controls. Normality of the antibody data was assessed using Shapiro-Wilks test. Comparisons of antibody levels in controls with melanoma, or pair-wise comparisons of controls with stage I–II, or stage III–IV melanoma were performed using Wilcoxon rank-sum tests due to non-normality of the data. Statistical significance was defined as a P value of <0.05. A Bonferroni correction was used to adjust for multiple, pair-wise comparisons.
Results
ML-IAP expression in patient tumors
Visceral metastatic tumors from eight-stage IV patients who had paraffin blocks available and consented to having their peripheral blood analyzed for immune responses were analyzed for ML-IAP expression by immunohistochemistry (Fig. 1a). Levels of ML-IAP expression in tumors were scored (+, ++, +++). One patient tumor had 3+ staining, 3 patient tumors had 2+ staining, 3 patient tumors had 1+ staining, and one tumor had no detectable expression. Due to the limited size of primary melanomas and tumor specimens involving lymph nodes (stage III), these samples were not available for analyses.
ML-IAP is frequently expressed in metastatic melanoma deposits. a Example of patient tumor staining positive for ML-IAP by immunohistochemistry of paraffin tissues (right) and isotype control (left). b Peptide sequence for isoforms α and β of the ML-IAP protein with corresponding overlapping peptides generated. Highlighted are sequences representing the previously recognized HLA-A2 peptides JS34, JS90, and IAP280. c Examples of T cell responses to overlapping peptides. Patient 29 responding to peptide pool IAP25-32 and patient 71 responding to peptide pool IAP33-39. d ELISPOT T cell responses to overlapping peptide pools in stage I–IV melanoma patients. PBMC were cultured with overlapping peptide pools of MLIAP for 1 week in the presence of 10 U/ml IL-2, and further restimulated with either L11 peptide (negative control) or the same peptide pools. Reported is the number of patients with positive responses to the depicted peptide pool by stage as well as for healthy donors (HD). The total refers to the number of patients in each stage that underwent peptide pool screening
T cell responses to ML-IAP overlapping peptide library
To gauge the incidence of cellular immune responses to ML-IAP in melanoma patients, a series of 15–18 mer peptides were generated to cover the full-length protein sequence with 10 mer overlap between each individual peptide (Fig. 1b). A total of 45 peptides were divided into 6 peptide pools. PBMC for stage I–IV melanoma patients were stimulated with the peptide pools for 1 week, and then stimulated a second time with the same peptide pools for readout of the ELISPOT assay. Multiple peptide pools of ML-IAP-induced T cell responses (Fig. 1c, d, and supplemental Figure 1A). The highest frequency of T cell responses in stage I/II patients occurred with IAP 25–32 and IAP 40–45, whereas in stage III/IV patients the highest frequencies of responses were found in IAP25-32 and IAP40-45. Cellular responses were also observed in some healthy donors (HD).
To confirm specific T cell immunity, purified (>90%) individual peptides from the ML-IAP peptide pools were further assessed by ELISPOT. If sufficient PBMCs were available, the relevant contribution of CD4+ or CD8+ T cell responses induced was examined by CD4/CD8 depletion (Fig. 2a). CD4+ responses dominated individual ML-IAP peptide reactivity. The frequency of T cell responses to identified peptides was also examined. As shown in supplemental Figure 1B, IAP15, IAP31, and IAP35 induced T cell response in stage I patients. T cell response to IAP21, 26, 39, and 44 were observed in stage III and IV patients.
T cell responses of melanoma patient PBMC to ML-IAP individual peptides. a CD4+ responses dominate cellular responses to ML-IAP peptides. T cell responses induced by individual ML-IAP peptides were further investigated for CD4+ and CD8+ responses. PBMC from patients were cultured with the individual peptide for 1 week. CD4+ or CD8+ T cells were isolated from the peptide-pretreated patient PBMC by relevant depletion, and these cells were restimulated with either L11 or the individual peptide for ELISPOT analysis. Responses for non-depleted, CD4 depleted, and CD8 depleted are presented. b and c Generation of IAP35 and IAP44-specific CD4+ T cells. CD4+ T cells were multi-stimulated with IAP35 or IAP44-pulsed autologous PBMC cells. The response of IAP35 or IAP44-specific CD4+ T cells is inhibited by a HLA DR blocking antibody (L243). The proliferative response of IAP35 or IAP44-specific CD4+ T cells to melanoma lines were further assessed by H3 uptake assay
CD4+ T cells for IAP26, IAP35, and IAP44 were generated from patient PBMCs. Antibody blocking experiments indicated that a HLA DQ antibody inhibited IAP26-induced CD4+ T cell responses (supplemental Figure C), whereas a HLA DR antibody abrogated IAP35 and IAP44-induced CD4+ T cell responses (Fig. 2b, c upper panels). Genotyping of these patients revealed that they were DQA1*05, DRB1*03/04, and DRB1*13/15. The responses of IAP35 and IAP44-specific CD4+ T cells to melanoma lines were further examined. As depicted in lower panels of Fig. 2b and c, IAP35 and IAP44 CD4+ cells had substantial proliferation to the HLA DRB1*04 melanoma cell line K028, and HLA DRB1*13 melanoma cell line COO2, respectively. In contrast, melanoma lines with alternate HLA DRB1 haplotypes did not result in significant proliferation.
T cell responses of melanoma patients to HLA-A*0201 binding epitopes of ML-IAP
As a result of the overlapping peptide screening, individual peptides IAP26 and IAP35 revealed CD8+ responses in addition to CD4+ responses in patient 29 and patient 71, respectively. Since patients 29 and 71 were class I genotyped to be HLA-A*0201, we examined whether HLA-A*0201 binding epitopes existed for peptides IAP26 and IAP35 by peptide prediction programs, HLA peptide binding predictions (http://www-bimas.cit.nih.gov/molbio/hla_bind/) and MHC class I binding peptide prediction server (http://bioinformatics.uams.edu/mirror/propred1/). The results of this analysis revealed potential HLA-A*0201 affinity peptide in IAP35 peptide identified as IAP237 (CLDRAVSIV, binding score: 26). In contrast, the binding scores of HLA-A*0201 peptides in IAP26 were very low.
Given the frequency of the HLA-A*0201 haplotype within the melanoma population, we next examined responses in HLA-A*0201 patient PBMC to IAP237. To gain additional context for these responses, we also examined the frequency of T cell responses to previously identified HLA-A*0201 ML-IAP peptides IAP280, JS34, and JS90 [26, 27] as well as peptides representing flu and the melanosomal differentiation antigen MART-1 (Fig. 3a). PBMC from normal HLA-A*0201 donors were also assessed for comparisons. IAP280, IAP237, and JS90 peptides induced detectable T cell responses in stage I–IV melanoma patients (Fig. 3b). As expected patients demonstrated reactivity to flu peptide. No reactivity was noted for the JS34 peptide in our tested patient population.
T cell responses to ML-IAP HLA-A*0201 epitopes. a Representative patient responses. Patient PBMC were pretreated with I280, JS90, and I237 peptides for 1 week and restimulated with either L11 or the same peptide for ELISPOT analysis. Flu and MART-1 HLA-A*0201 peptides were utilized for comparison. b Summary of responses to predicted HLA-A*0201 epitopes from normal donors and stage I–IV melanoma patients (responders/number tested)
Finally, we investigated additional predicted HLA-A*0201 peptides that were represented but relatively low CD8+ responses in our overlapping peptides screening since longer peptides possess lower binding affinities. Individual peptide IAP21 (CQFLLRSKGRDFVHSV) contained predicted HLA-A*0201 peptide IAP154 (LLRSKGRDFV, binding score: 24.2) and IAP158 (KGRDFVHSV, binding score: 4.328). Individual peptide IAP26 (AAPVAPSVPASGYPEL) contained IAP192 (SVPASGYPEL, binding score 2.8). IAP154 and IAP192 did demonstrate low frequency of reactivity in stage I–IV melanoma patients (Fig. 3b). There was no detectable reactivity for IAP158.
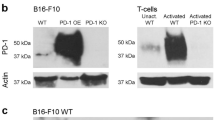
Generation and functional characterization of IAP237-specific CTL
To determine the functional significance of identified epitope-specific CTL, IAP237 CTL were generated using CD40L activated B cells as antigen presenting cells from normal HLA-A*0201 donors (Fig. 4). T2 cells in the presence of 10 μg/ml peptide revealed functional and specific activities including target killing (Fig. 4a). In contrast, IAP237 CTLs exhibited different abilities to lyse HLA-A*0201 positive melanoma cell lines that express ML-IAP (Fig. 4b). The killing activities against K029 and K028 were enhanced in the presence of 10 μg/ml I237 peptide. K008 and K028 melanoma cell lines have low expression of ML-IAP by immunoblotting, while K029 has strong ML-IAP expression. All cell lines have evidence for ML-IAP expression by RT-PCR (data not shown). The K008 melanoma cell line is genotypically HLA-A*0201, but fails to express HLA A2 molecules on its surface as determined by flow cytometry. As a result, the K008 cell line experienced less cytotoxic killing as compared to other cell lines tested. I280 and JS90-specific CTL also demonstrated similar patterns of activity against tumor lines (data not shown).
Generation of CTL to ML-IAP HLA-A*0201 epitopes. PBMC from HLA-A*0201 donors underwent multiple rounds of stimulation with CD40L-activated B cells pulsed with IAP237 peptide. CD8+ cells were further enriched by IFN-γ selection and the cells expanded in the presence of irradiated PBMC, PHA, and IL-2. a ELISPOT assay for γ-IFN production proved specific IAP237 CD8+ CTL (left upper panel). Specificity to HLA-A*0201 activity was further demonstrated by the ability to block activity with the addition of the anti-class I antibody W6/32 (left lower panel). Functional cytotoxicity of manufactured cells was further revealed by CTL assay utilizing T2 cells in the presence of 10 μg/ml IAP237 peptide (right panel). The effector to target ratio (E/T) is represented on the x-axis and percent cytotoxicity is represented on the y-axis. b The cytolytic activity of IAP237 CTL were further analyzed against HLA-A2 expressing melanoma cell lines in the absence (left panel) or presence of 10 μg/ml IAP237 peptide (right panel). Melanoma cell line K029 expresses ML-IAP while cell lines K008 and K028 have very low level of ML-IAP expression. Cell line K008 has lost surface HLA-A2 expression as determined by flow cytometry
Humoral immune responses of melanoma patients to ML-IAP
To further characterize these immune responses to ML-IAP, we evaluated the antibody responses to ML-IAP in our melanoma patient population. Recombinant ML-IAP protein was generated and purity confirmed by Coomassie staining (Fig. 5a, left panel) and immunoblot analysis utilizing a ML-IAP-specific monoclonal antibody [26] (Fig. 5a, middle panel). Patients whose sera revealed significant titers of antibodies to ML-IAP by ELISA were confirmed for specificity by immunoblotting (Fig. 5a, right panel). Sera from normal donors and patients with stage I–IV melanoma were analyzed by ELISA (Fig. 5b). Several melanoma patients had higher titers of antibody responses to ML-IAP in comparison to normal donors. However, the distributions of antibody values between melanoma patients and controls were not statistically significant (Wilcoxon rank-sum P = 0.09), nor were there differences in antibody values for stages I–II melanoma compared with stages III–IV (Wilcoxon rank-sum P = 0.94).
Humoral immunity of melanoma patients and healthy donors to recombinant ML-IAP protein. a Purified recombinant ML-IAP protein was confirmed by Coomassie blue staining (left panel) and immunoblotting with ML-IAP-specific monoclonal antibody [26] (middle panel). Specificities of patient humoral responses to ML-IAP by ELISA were confirmed by immunoblotting using patient sera and recombinant protein (right panel). b Antibody titers to recombinant ML-IAP from stage I/II and III/IV melanoma patients and healthy donor sera as determined by ELISA. Sera from fifteen healthy donors and sera from fifteen patients representing each stage of disease (60 melanoma patients total) were assayed. Humoral responses of melanoma patients to recombinant ML-IAP protein after ipilimumab plus bevacizumab treatment. c Antibody titers to recombinant ML-IAP from two different patients sera as determined by ELISA. Pretreatment and treatment time courses are represented. Arrows represent treatment times. d Specificities of the patient humoral responses to ML-IAP by ELISA were confirmed by immunoblotting using patient sera and ML-IAP recombinant protein
Overall ML-IAP immunity in melanoma patients
Table 1 summarizes the immune responses to ML-IAP in stage I–IV melanoma patients and healthy donors (HD). T cell immunity is reported as responding to one-peptide pool, two-peptide pools, or three-peptide pools per patient. Most patients responded to only one-peptide pool, several responded to two-peptide pools, and only one stage IV patient responded to three-peptide pools. No individual responded to more than three-peptide pools. In comparison, two healthy donors responded to a single peptide pool and one healthy donor responded to two-peptide pools. The percentage of patients for each group who had detectable T cell responses, detectable serologic responses, or either a T cell or serologic response to ML-IAP are also presented. For stage I/II patients, 31% had either a cellular or humoral response, and 5% had both a cellular and humoral response to ML-IAP, whereas for stage III/IV patients 57 and 14% were observed, respectively. In comparison, none of the healthy donors examined had a serologic response to ML-IAP, and 20% had detectable T cell responses. Taken together, our data indicate the existence of spontaneous immune response against ML-IAP in melanoma patients.
Significance of immune responses to ML-IAP in melanoma patients receiving CTLA-4 blockade-based therapy
To further investigate the significance of immunity to ML-IAP, we examined the serologic responses of 10 patients who received ipilimumab (10 mg/kg) plus bevacizumab (15 mg/kg) in a phase I clinical trial. Treatment dramatically augmented antibody responses against ML-IAP in two patients as shown by ELISA time course and immunoblotting (Fig. 5c, d). Moreover, there are no responses to another IAP family member, survivin (data not shown). One of these patients had preexisting humoral immunity to ML-IAP. Both patients experienced significant clinical benefit from treatment with stable disease or partial response for greater than 6 months.
Discussion
ML-IAP is well established as a critical component for melanoma propagation and survival. The microphthalmia-associated transcription factor MITF, a known melanoma-associated oncogene [29] and central regulator in melanoma, has been found to regulate ML-IAP transcription in melanoma cells [30]. Furthermore, there is an increased expression of ML-IAP in primary as well as metastatic melanomas as compared to melanocytic nevi [16]. The significance of ML-IAP to tumor cell survival is further evidenced by the induction of apoptosis through silencing RNA targeting of ML-IAP [31].
Since most cancers rely on anti-apoptotic mechanisms to propagate tumor cell growth as well as provide treatment resistance, the members of the inhibitor of apoptosis family are highly attractive to fulfill this role as functionally significant antigens. Spontaneous immune responses to anti-apoptotic proteins such as Bcl-xL in a variety of cancers suggest that such immunity may be a generalized event [32]. The most studied member of the IAP family from an immune perspective is survivin, found to be the target of CD4+, CD8+, and humoral immune responses in a variety of cancers [33–40] as well as a tumor rejection antigen in patients [41]. In comparison, humoral and cellular immune responses to ML-IAP have sporadically been reported [27, 40]. Aberrant expression of ML-IAP in lung cancer, for example, has been associated with the detection of ML-IAP-specific CTL in the peripheral blood of patients [38]. Significant antibody titers to ML-IAP have also been detected in lung cancer, gastrointestinal cancer, and breast cancer patients [39, 40, 42]. These reports strongly suggest the broad antigenic potential of ML-IAP in cancer.
The current report reveals spontaneous immune responses in melanoma patients to an array of ML-IAP epitopes spanning the protein’s entire sequence. The overlapping peptide library was most sensitive for detecting CD4+ T cell responses. It is possible that CD4+ T cell responses are present at higher precursor frequency in these patients. Additionally, MHC class II epitopes have significantly greater promiscuity for binding than class I peptides, likely contributing to this phenomenon when utilizing 18 mer peptides in our screening. This approach was nonetheless able to identify several class I epitopes including the novel HLA-A*0201 IAP237 peptide. Importantly, the broad cellular immunogenicity of ML-IAP in melanoma patients is evidenced by the significant rate of reactivity revealed in this screening involving both CD4+ and CD8+ responses. The importance of ML-IAP to melanoma is highlighted by the fact that half of all melanoma patients have developed spontaneous immunity to this antigen. The presence of both cellular and humoral immune responses in individual patients suggests potential for coordination of multiple immune effector mechanisms targeting ML-IAP.
While the frequency of immune responses to ML-IAP appears higher in melanoma patients, there were detectable responses in healthy individuals. While not statistically significant, there is a trend toward greater frequency of cellular and humoral immune responses in advanced melanoma patients as compared to earlier stage or healthy individuals. In addition, spontaneous CTL responses to ML-IAP have been reported in melanoma patients as well as some healthy individuals. There may exist a hierarchy of antigens with respect to their ability to induce spontaneous immune responses in healthy individuals versus the tumor bearing host.
The ability to generate functional ML-IAP CTL that lyse targets confirms the significance of identified epitopes and relevance to the pursuit of targeting ML-IAP for therapeutic development. This ability is dependent on the presentation of naturally processed epitope on the target surface. Immunodominant HLA-A2 restricted MART-1 epitope has frequently been reported to not be presented on the surface of melanoma cells [43]. Since immunodominant epitopes can fail to be presented in some tumors, dysfunctional regulation of epitope expression in cancer cells remains a significant potential mechanism of tumor immune evasion. Inadequate epitope presentation on melanoma cell lines utilized in the current study would limit target killing by CTL, and proliferation of antigen-specific CD4+ T cells. Our detection of broad spontaneous immune responses to ML-IAP via overlapping peptides suggests that some of these epitopes can naturally be presented. One limitation in such investigation is the technical difficulty to detect ML-IAP peptides on the surface of melanoma cells. Development of such methods for peptide detection, for example mass spectrometry to identify MHC associated peptides, will likely prove insightful.
The broad immunogenicity of ML-IAP in melanoma patients further supports its importance as an immune target for therapeutic development and as a marker of disease. Three of three patients who had detectable immune responses to ML-IAP and five of six who did not have detectable immune responses exhibited significant expression of ML-IAP in their tumors (1+ or greater by immunohistochemistry). From available patient tumor samples, only one lacked expression of ML-IAP in a patient that did not exhibit detectable cellular or humoral immune responses. The degree of ML-IAP expression by immunohistochemistry and development of immune responses were not able to be directly correlated due to the small number of pathology samples available in patients whose PBMC and sera were utilized.
Ipilimumab is a fully human CTLA4 blocking antibody that is able to augment immune response against melanoma [44] and has recently been demonstrated to offer a survival advantage for patients [45]. The improvement in ML-IAP humoral immunity as a function of treatment not only validates ML-IAP as an antigen target, but also provides insight to the mechanism of effective antitumor immunity of CTLA-4 blockade.
Despite the high incidence of spontaneous immunity witnessed against ML-IAP in melanoma patients, these nascent responses were not sufficient to prevent the development of melanoma or its progression. One possibility for this is the concurrent induction of immune regulatory pathways that limit the antitumor efficacy of ML-IAP-specific immunity. For such cases, intervention with checkpoint blockade may provide improvement of ML-IAP effector responses. In addition, there are overlapping functions of the anti-apoptotic family members such that it may be necessary to target other critical proteins, such as survivin, XIAP, and BCL-2.
CTL from the peripheral blood of healthy donors were manufactured and functional in targeting ML-IAP. This provides the basis for vaccination and whole cell therapeutic approaches. Given its broad expression, its functional importance in tumor propagation, and high incidence of immune responses in melanoma patients, clinical investigation targeting ML-IAP is worthy of pursuit.
References
Slingluff CL Jr, Petroni GR, Yamshchikov GV, Barnd DL, Eastham S, Galavotti H, Patterson JW, Deacon DH, Hibbitts S, Teates D, Neese PY, Grosh WW, Chianese-Bullock KA, Woodson EM, Wiernasz CJ, Merrill P, Gibson J, Ross M, Engelhard VH (2003) Clinical and immunologic results of a randomized phase II trial of vaccination using four melanoma peptides either administered in granulocyte-macrophage colony-stimulating factor in adjuvant or pulsed on dendritic cells. J Clin Oncol 21:4016–4026
Gaugler B, Van den Eynde B, van der Bruggen P, Romero P, Gaforio JJ, De Plaen E, Lethe B, Brasseur F, Boon T (1994) Human gene MAGE-3 codes for an antigen recognized on a melanoma by autologous cytolytic T lymphocytes. J Exp Med 179:921–930
van der Bruggen P, Traversari C, Chomez P, Lurquin C, De Plaen E, Van den Eynde B, Knuth A, Boon T (1991) A gene encoding an antigen recognized by cytolytic T lymphocytes on a human melanoma. Science 254:1643–1647
Jager E, Chen YT, Drijfhout JW, Karbach J, Ringhoffer M, Jager D, Arand M, Wada H, Noguchi Y, Stockert E, Old LJ, Knuth A (1998) Simultaneous humoral and cellular immune response against cancer-testis antigen NY-ESO-1: definition of human histocompatibility leukocyte antigen (HLA)-A2-binding peptide epitopes. J Exp Med 187:265–270
Jager E, Gnjatic S, Nagata Y, Stockert E, Jager D, Karbach J, Neumann A, Rieckenberg J, Chen YT, Ritter G, Hoffman E, Arand M, Old LJ, Knuth A (2000) Induction of primary NY-ESO-1 immunity: CD8+ T lymphocyte and antibody responses in peptide-vaccinated patients with NY-ESO-1+ cancers. Proc Natl Acad Sci USA 97:12198–12203
Jager E, Ringhoffer M, Arand M, Karbach J, Jager D, Ilsemann C, Hagedorn M, Oesch F, Knuth A (1996) Cytolytic T cell reactivity against melanoma-associated differentiation antigens in peripheral blood of melanoma patients and healthy individuals. Melanoma Res 6:419–425
Sanchez-Perez L, Kottke T, Diaz RM, Ahmed A, Thompson J, Chong H, Melcher A, Holmen S, Daniels G, Vile RG (2005) Potent selection of antigen loss variants of B16 melanoma following inflammatory killing of melanocytes in vivo. Cancer Res 65:2009–2017
Lozupone F, Rivoltini L, Luciani F, Venditti M, Lugini L, Cova A, Squarcina P, Parmiani G, Belardelli F, Fais S (2003) Adoptive transfer of an anti-MART-1(27–35)-specific CD8+ T cell clone leads to immunoselection of human melanoma antigen-loss variants in SCID mice. Eur J Immunol 33:556–566
Riker A, Cormier J, Panelli M, Kammula U, Wang E, Abati A, Fetsch P, Lee KH, Steinberg S, Rosenberg S, Marincola F (1999) Immune selection after antigen-specific immunotherapy of melanoma. Surgery 126:112–120
Khong HT, Wang QJ, Rosenberg SA (2004) Identification of multiple antigens recognized by tumor-infiltrating lymphocytes from a single patient: tumor escape by antigen loss and loss of MHC expression. J Immunother 27:184–190
Yamshchikov GV, Mullins DW, Chang CC, Ogino T, Thompson L, Presley J, Galavotti H, Aquila W, Deacon D, Ross W, Patterson JW, Engelhard VH, Ferrone S, Slingluff CL Jr (2005) Sequential immune escape and shifting of T cell responses in a long-term survivor of melanoma. J Immunol 174:6863–6871
Hersey P (1997) Melanoma vaccines: prospects for the treatment of melanoma. Expert Opin Investig Drugs 6:267–277
Robbins PF, El-Gamil M, Li YF, Kawakami Y, Loftus D, Appella E, Rosenberg SA (1996) A mutated beta-catenin gene encodes a melanoma-specific antigen recognized by tumor infiltrating lymphocytes. J Exp Med 183:1185–1192
Schimmer AD (2004) Inhibitor of apoptosis proteins: translating basic knowledge into clinical practice. Cancer Res 64:7183–7190
Kato J, Kuwabara Y, Mitani M, Shinoda N, Sato A, Toyama T, Mitsui A, Nishiwaki T, Moriyama S, Kudo J, Fujii Y (2001) Expression of survivin in esophageal cancer: correlation with the prognosis and response to chemotherapy. Int J Cancer 95:92–95
Gong J, Chen N, Zhou Q, Yang B, Wang Y, Wang X (2005) Melanoma inhibitor of apoptosis protein is expressed differentially in melanoma and melanocytic naevus, but similarly in primary and metastatic melanomas. J Clin Pathol 58:1081–1085
Augello C, Caruso L, Maggioni M, Donadon M, Montorsi M, Santambrogio R, Torzilli G, Vaira V, Pellegrini C, Roncalli M, Coggi G, Bosari S (2009) Inhibitors of apoptosis proteins (IAPs) expression and their prognostic significance in hepatocellular carcinoma. BMC Cancer 9:125
Wagener N, Crnkovic-Mertens I, Vetter C, Macher-Goppinger S, Bedke J, Grone EF, Zentgraf H, Pritsch M, Hoppe-Seyler K, Buse S, Haferkamp A, Autschbach F, Hohenfellner M, Hoppe-Seyler F (2007) Expression of inhibitor of apoptosis protein livin in renal cell carcinoma and non-tumorous adult kidney. Br J Cancer 97:1271–1276
Lin JH, Deng G, Huang Q, Morser J (2000) KIAP, a novel member of the inhibitor of apoptosis protein family. Biochem Biophys Res Commun 279:820–831
Ashhab Y, Alian A, Polliack A, Panet A, Ben Yehuda D (2001) Two splicing variants of a new inhibitor of apoptosis gene with different biological properties and tissue distribution pattern. FEBS Lett 495:56–60
Crnkovic-Mertens I, Muley T, Meister M, Hartenstein B, Semzow J, Butz K, Hoppe-Seyler F (2006) The anti-apoptotic livin gene is an important determinant for the apoptotic resistance of non-small cell lung cancer cells. Lung Cancer 54:135–142
Vucic D, Deshayes K, Ackerly H, Pisabarro MT, Kadkhodayan S, Fairbrother WJ, Dixit VM (2002) SMAC negatively regulates the anti-apoptotic activity of melanoma inhibitor of apoptosis (ML-IAP). J Biol Chem 277:12275–12279
Vucic D, Fairbrother WJ (2007) The inhibitor of apoptosis proteins as therapeutic targets in cancer. Clin Cancer Res 13:5995–6000
Nachmias B, Ashhab Y, Bucholtz V, Drize O, Kadouri L, Lotem M, Peretz T, Mandelboim O, Ben-Yehuda D (2003) Caspase-mediated cleavage converts livin from an antiapoptotic to a proapoptotic factor: implications for drug-resistant melanoma. Cancer Res 63:6340–6349
Liu B, Han M, Wen JK, Wang L (2007) Livin/ML-IAP as a new target for cancer treatment. Cancer Lett 250:168–176
Schmollinger JC, Vonderheide RH, Hoar KM, Maecker B, Schultze JL, Hodi FS, Soiffer RJ, Jung K, Kuroda MJ, Letvin NL, Greenfield EA, Mihm M, Kutok JL, Dranoff G (2003) Melanoma inhibitor of apoptosis protein (ML-IAP) is a target for immune-mediated tumor destruction. Proc Natl Acad Sci USA 100:3398–3403
Andersen M, Reker S, Becker J, Straten PT (2004) The melanoma inhibitor of apoptosis protein: a target for spontaneous cytotoxic T cell responses. J Invest Dermatol 122:392–399
von Bergwelt-Baildon MS, Vonderheide RH, Maecker B, Hirano N, Anderson KS, Butler MO, Xia Z, Zeng WY, Wucherpfennig KW, Nadler LM, Schultze JL (2002) Human primary and memory cytotoxic T lymphocyte responses are efficiently induced by means of CD40-activated B cells as antigen-presenting cells: potential for clinical application. Blood 99:3319–3325
Garraway LA, Widlund HR, Rubin MA, Getz G, Berger AJ, Ramaswamy S, Beroukhim R, Milner DA, Granter SR, Du J, Lee C, Wagner SN, Li C, Golub TR, Rimm DL, Meyerson ML, Fisher DE, Sellers WR (2005) Integrative genomic analyses identify MITF as a lineage survival oncogene amplified in malignant melanoma. Nature 436:117–122
Dynek JN, Chan SM, Liu J, Zha J, Fairbrother WJ, Vucic D (2008) Microphthalmia-associated transcription factor is a critical transcriptional regulator of melanoma inhibitor of apoptosis in melanomas. Cancer Res 68:3124–3132
Crnkovic-Mertens I, Hoppe-Seyler F, Butz K (2003) Induction of apoptosis in tumor cells by siRNA-mediated silencing of the livin/ML-IAP/KIAP gene. Oncogene 22:8330–8336
Andersen MH, Becker JC, Straten P (2005) Regulators of apoptosis: suitable targets for immune therapy of cancer. Nat Rev Drug Discov 4:399–409
Andersen MH, thor SP (2002) Survivin—a universal tumor antigen. Histol Histopathol 17:669–675
Reker S, Becker JC, Svane IM, Ralfkiaer E, Straten PT, Andersen MH (2004) HLA-B35-restricted immune responses against survivin in cancer patients. Int J Cancer 108:937–941
Reker S, Meier A, Holten-Andersen L, Svane IM, Becker JC, thor Straten P, Andersen MH (2004) Identification of novel survivin-derived CTL epitopes. Cancer Biol Ther 3:173–179
Casati C, Dalerba P, Rivoltini L, Gallino G, Deho P, Rini F, Belli F, Mezzanzanica D, Costa A, Andreola S, Leo E, Parmiani G, Castelli C (2003) The apoptosis inhibitor protein survivin induces tumor-specific CD8+ and CD4+ T cells in colorectal cancer patients. Cancer Res 63:4507–4515
Andersen MH, Svane IM, Becker JC, Straten PT (2007) The universal character of the tumor-associated antigen survivin. Clin Cancer Res 13:5991–5994
Hariu H, Hirohashi Y, Torigoe T, Asanuma H, Hariu M, Tamura Y, Aketa K, Nabeta C, Nakanishi K, Kamiguchi K, Mano Y, Kitamura H, Kobayashi J, Tsukahara T, Shijubo N, Sato N (2005) Aberrant expression and potency as a cancer immunotherapy target of inhibitor of apoptosis protein family, livin/ML-IAP in lung cancer. Clin Cancer Res 11:1000–1009
Yagihashi A, Asanuma K, Kobayashi D, Tsuji N, Shijubo Y, Abe S, Hirohashi Y, Torigoe T, Sato N, Watanabe N (2005) Detection of autoantibodies to livin and survivin in Sera from lung cancer patients. Lung Cancer 48:217–221
Yagihashi A, Asanuma K, Tsuji N, Torigoe T, Sato N, Hirata K, Watanabe N (2003) Detection of anti-livin antibody in gastrointestinal cancer patients. Clin Chem 49:1206–1208
Wobser M, Keikavoussi P, Kunzmann V, Weininger M, Andersen MH, Becker JC (2006) Complete remission of liver metastasis of pancreatic cancer under vaccination with a HLA-A2 restricted peptide derived from the universal tumor antigen survivin. Cancer Immunol Immunother 55:1294–1298
Yagihashi A, Ohmura T, Asanuma K, Kobayashi D, Tsuji N, Torigoe T, Sato N, Hirata K, Watanabe N (2005) Detection of autoantibodies to survivin and livin in sera from patients with breast cancer. Clin Chim Acta 362:125–130
Sorensen RB, Junker N, Kirkin A, Voigt H, Svane IM, Becker JC, Thor Straten P, Andersen MH (2009) The immunodominant HLA-A2-restricted MART-1 epitope is not presented on the surface of many melanoma cell lines. Cancer Immunol Immunother 58:665–675
Yuan J, Gnjatic S, Li H, Powel S, Gallardo HF, Ritter E, Ku GY, Jungbluth AA, Segal NH, Rasalan TS, Manukian G, Xu Y, Roman RA, Terzulli SL, Heywood M, Pogoriler E, Ritter G, Old LJ, Allison JP, Wolchok JD (2008) CTLA-4 blockade enhances polyfunctional NY-ESO-1 specific T cell responses in metastatic melanoma patients with clinical benefit. Proc Natl Acad Sci USA 105:20410–20415
Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, Akerley W, van den Eertwegh AJ, Lutzky J, Lorigan P, Vaubel JM, Linette GP, Hogg D, Ottensmeier CH, Lebbe C, Peschel C, Quirt I, Clark JI, Wolchok JD, Weber JS, Tian J, Yellin MJ, Nichol GM, Hoos A, Urba WJ (2010) Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 363:711–723
Acknowledgments
This work was supported in part by The Ron Gelb Melanoma Research Fund and Malcolm and Emily Mac Naught Fund for Melanoma Research at Dana-Farber Cancer Institute. The authors do not have additional financial relationships with the organizations that sponsored the research.
Conflict of interest
F.S.H. has been named in a patent identifying ML-IAP as an antigen target.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
262_2011_1124_MOESM1_ESM.doc
Supplemental Figure 1. T cell responses to overlapping peptide pools in stage I-IV melanoma patients by ELISPOT. PBMC were cultured with overlapping peptide pools of ML-IAP for one week in the presence of 10 U/ml IL-2, and further stimulated with either L11 peptide (negative control) or the same peptide pools. (A) Patients with positive responses to the peptide pool are shown by stage. (B) Frequency of T cell responses to the identified peptides in stage I-IV melanoma patients. (C) Generation of IAP26-specific CD4+ T cells. CD4+ T cells were multi-stimulated with IAP26 pulsed autologous PBMC cells. The responses of IAP26-specific CD4+ T cells are inhibited by a HLA DQ blocking antibody (SPVL3). (DOC 771 kb)
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Zhou, J., Yuen, N.K., Zhan, Q. et al. Immunity to the melanoma inhibitor of apoptosis protein (ML-IAP; livin) in patients with malignant melanoma. Cancer Immunol Immunother 61, 655–665 (2012). https://doi.org/10.1007/s00262-011-1124-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-011-1124-1