Abstract
Purpose
The impact of quantitative parameters on the differentiation of primary colorectal tumours from normal colon tissue was assessed. Dynamic PET data (DPET) were acquired, and compartment and non-compartment modelling applied. The discriminant power of single parameters and the combination of PET parameters was assessed. All lesions were confirmed by histology.
Methods
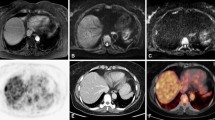
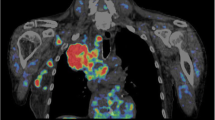
FDG DPET studies were acquired in 22 patients with colorectal tumours prior to surgery. Five of these patients also had liver metastases at the time of the PET study. The SUV 56–60 min p.i. was included in the evaluation. A two-tissue compartment model was applied and the parameters k 1–k 4 as well as the fractional blood volume (V B) were obtained. The FDG influx was calculated from the compartment data. Non-compartment modelling was used to calculate the fractal dimension (FD) of the time-activity data.
Results
FD, SUV, influx and k 3 were the most important single parameters for lesion differentiation. The highest accuracy was achieved for FD (88.78%). The overall tracer uptake was mainly dependent on k 3 and not on k 1 or V B. The support vector machines (SVM) algorithm was used to predict the classification based on the combination of individual PET parameters. The overall accuracy was 97.3%, with only one false positive case and no false negative results. The analysis of the subgroup of five patients with primary tumours and synchronous metastases revealed no significant differences for the individual PET parameters. However, V B tended to be lower while k 1 and k 2 were higher in patients with synchronous metastases. The SVM classification analysis predicted the presence of metastases based on the PET data of the primary tumour in three of five patients.
Conclusion
Quantitative FDG PET studies provide very accurate data for the differentiation of primary colorectal tumours from normal tissue. The use of quantitative data has the advantage that the detection of a colorectal tumour is not primarily dependent on the individual assessment and experience of the physician evaluating the FDG PET data only visually. The results suggest that the presence of metastatic lesions may be predicted by analysis of the dynamic PET data of the corresponding primary tumour. Further studies are needed to assess this aspect in detail.




Similar content being viewed by others
References
Gambhir SS, Czernin J, Schwimmer J, Silverman DHS, Coleman RE, Phelps ME. A tabulated summary of the FDG PET literature. J Nucl Med 2001;42:1S–93S.
Koslin DB. Update on gastrointestinal imaging. Rev Gastroenterol Disord 2002;2:3–10.
Furukawa H, Ikuma H, Seki A, Yokoe K, Yuen S, Aramaki T, et al. Positron emission tomography scanning is not superior to whole-body multi-detector helical computed tomography in the preoperative staging of colorectal cancer. Gut 2005;55:1007–11.
Strauss LG, Conti PS. The applications of PET in clinical oncology. J Nucl Med 1991;32:623–48.
Burger C, Buck A. Requirements and implementations of a flexible kinetic modeling tool. J Nucl Med 1997;38:1818–23.
Mikolajczyk K, Szabatin M, Rudnicki P, Grodzki M, Burger C. A Java environment for medical image data analysis: initial application for brain PET quantitation. Med Inform 1998;23:207–14.
Miyazawa H, Osmont A, Petit-Taboué MC, Tillet I, Travère JM, Young AR, et al. Determination of 18F-fluoro-2-deoxy-D-glucose rate constants in the anesthetized baboon brain with dynamic positron tomography. J Neurosci Methods 1993;50:263–72.
Sokoloff L, Smith CB. Basic principles underlying radioisotopic methods for assay of biochemical processes in vivo. In: Greitz T, Ingvar DH, Widén L, editors. The metabolism of the human brain studied with positron emission tomography. New York: Raven Press; 1983; p. 123–48.
Ohtake T, Kosaka N, Watanabe T, Yokoyama I, Moritan T, Masuo M, et al. Noninvasive method to obtain input function for measuring glucose utilization of thoracic and abdominal organs. J Nucl Med 1991;32:1432–8.
Peitgen HO, Juergens H, Saupe D. Length, area and dimension: measuring complexity and scaling properties. In: Peitgen HO, Juergens H, Saupe D, editors. Chaos and fractals. New York: Springer; 1992; p. 192–219.
Chen PH, Lin CJ, Schölkopf B. A tutorial on v-support vector machines. Appl Stoch Models Bus Ind 2005;21:111–36.
Chu F, Wang L. Applications of support vector machines to cancer classification with microarray data. Int J Neural Syst 2005;15:475–84.
Guyon I, Weston J, Barnhill S, Vapnik V. Gene selection for cancer classification using support vector machines. Mach Learn 2002;46:389–422.
Oh JH, Nandi A, Gurnai P, Knowles L, Schorge J. Diagnosis of early relapse in ovarian cancer using serum proteomic profiling. Genome Inform 2005;16:195–204.
Strauss LG, Clorius JH, Schlag P, Lehner B, Kimmig B, Engenhart R, et al. Recurrence of colorectal tumours: PET evaluation. Radiology 1989;70:329–32.
Kantorová I, Lipská L, Bělohlávek O, Visokai V, Trubač M, Schneiderová M. Routine 18F-FDG PET preoperative staging of colorectal cancer: comparison with conventional staging and its impact on treatment decision making. J Nucl Med 2003;44:1784–8.
Keogan MT, Lowe VJ, Baker ME, McDermott VG, Lyerly HK, Coleman RE. Local recurrence of rectal cancer: evaluation with F-18 fluorodeoxyglucose PET imaging. Abdom Imaging 1997;22:332–7.
Dev P. Basic principles and applications of fractal geometry in pathology: a review. Anal Quant Cytol Histol 2005;27:284–90.
Strauss LG, Dimitrakopoulou-Strauss A, Koczan D, Bernd L, Haberkorn U, Ewerbeck V, et al. 18F-FDG kinetics and gene expression in giant cell tumours. J Nucl Med 2004;45:1528–35.
Koukouraki S, Strauss, LG, Georgoulias V, Schuhmacher J, Haberkorn U, Karkavitsas N, et al. Evaluation of the pharmacokinetics of 68Ga-DOTATOC in patients with metastatic neuroendocrine tumours scheduled for 90Y-DOTATOC therapy. Eur J Nucl Med Mol Imaging 2006;33:460–6.
Dimitrakopoulou-Strauss A, Strauss LG, Schwarzbach M, Burger C, Heichel T, Willeke F, et al. Dynamic PET 18F-FDG studies in patients with primary and recurrent soft-tissue sarcomas: impact on diagnosis and correlation with grading. J Nucl Med 2001;42:713–20.
Dimitrakopoulou-Strauss A, Georgoulias V, Eisenhut M, Koukouraki S, Mäcke HR, Haberkorn U, et al. Quantitative assessment of SSTR2 expression in patients with non-small cell lung cancer using 68Ga-DOTATOC PET and comparison with 18F-FDG PET. Eur J Nucl Med Mol Imaging 2006;33:823–30.
de Geus-Oei LF, Visser EP, Krabbe PFM, van Hoorn BA, Koenders EB, Willemsen AT, et al. Comparison of image-derived and arterial input functions for estimating the rate of glucose metabolism in therapy-monitoring 18F-FDG PET studies. J Nucl Med 2006;47:945–9.
Strauss LG, DImitrakopoulou-Strauss A, Haberkorn U. Shortened PET data acquisition protocol for the quantification of 18F-FDG kinetics. J Nucl Med 2003;44:1933–9.
Wei L, Yang Y, Nishikawa RM, Wenick MN, Edwards A. Relevance vector machine for automatic detection of clustered microcalcifications. IEEE Trans Med Imaging 2005;24:1278–85.
Macheda ML, Rogers S, Best JD. Molecular and cellular regulation of glucose transporter (GLUT) proteins in cancer. J Cell Physiol 2005;202:654–62.
Sakashita M, Aoyama N, Minami R, Maekawa S, Kuroda K, Shirasaka D, et al. Glut1 expression in T1 and T2 stage colorectal carcinomas: its relationship to clinicopathological features. Eur J Cancer 2001;37:204–9.
Haber RS, Rathan A, Weiser KR, Pritsker A, Itzkowitz SH, Bodian C, et al. GLUT1 glucose transporter expression in colorectal carcinoma: a marker for poor prognosis. Cancer 1998;83:34–40.
Burt BM, Humm JL, Kooby DA, Squire OD, Mastorides S, Larson SM, et al. Using positron emission tomography with [18F]FDG to predict tumour behavior in experimental colorectal cancer. Neoplasia 2001;3:189–95.
Fanciulli M, Bruno T, Giovannelli A, Gentile FP, Di Padova M, Rubiu O, et al. Energy metabolism of human LoVo colon carcinoma cells: correlation to drug resistance and influence of lonidamine. Clin Cancer Res 2000;6:1590–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Strauss, L.G., Klippel, S., Pan, L. et al. Assessment of quantitative FDG PET data in primary colorectal tumours: which parameters are important with respect to tumour detection?. Eur J Nucl Med Mol Imaging 34, 868–877 (2007). https://doi.org/10.1007/s00259-006-0319-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-006-0319-8