Abstract
Purpose
Oral vitamin E is used in several childhood diseases, but dosage recommendations differ. Few oral products have a marketing authorization for therapeutic use in children. Preliminary data indicate differences in bioavailability among the various vitamin E compounds. Our objective was to review published data on oral vitamin E therapy in neonates and children in order to establish dosage recommendations at a local level.
Methods
A literature search was conducted, including Medline Ovid, EMBASE (1980-Feb 2008), Cochrane databases, product monographs, handbooks, and textbooks.
Results
The main vitamin E compounds being used in children are α-tocopherol, α-tocopheryl acetate, and tocofersolan. The most data are available on tocopheryl acetate, both in neonates and older children. In children with malabsorption disorders, tocofersolan appears to have an increased bioavailability compared to tocopherol or tocopheryl acetate. Published data on pharmacokinetics and dosages for clinical use are few and heterogeneous. No pharmacokinetic studies were found for tocofersolan in neonates and infants. There are few comparative studies on pharmacokinetics, therapeutic use, and adverse drug reactions (ADRs) in children. Dosages used in clinical studies and dosage recommendations in handbooks differ considerably.
Conclusions
The differences in dosing recommendations in children may be due to lack of systematic studies. Existing published data on oral vitamin E do not provide a basis for evaluation of dosage recommendations in children. Comparative clinical studies are required for scientific evaluation of pharmacokinetics, dosage regimens, and efficacy/ADR assessments in children.
Similar content being viewed by others
Introduction
Oral vitamin E is used in several childhood diseases, such as for prevention of retinopathy of prematurity (ROP), growth retardation, fat malabsorption (e.g., cystic fibrosis, cholestatic diseases), and other chronic diseases in infants and children with vitamin E deficiency. In neonates, vitamin E is administered to alter the antioxidant status in order to prevent free-radical damage in cell membranes, to inhibit inflammatory processes by modulating cellular signals, to regulate transcriptions, and to stimulate the infants’ immune system [1]. In children with fat malabsorption, vitamin E is administered to prevent neuropathy, gastrointestinal disturbances, and myopathy caused by vitamin E deficiency.
Few oral products have been approved by regulatory authorities, resulting in “off-label” or unlicensed use and extempore pharmacy compounding [2–4]. Discussions with physicians and pharmacists revealed different recommendations on doses, formulations, and drug of choice. The diversity was confirmed in a later survey [5]. Some oral vitamin E products may contain excipients, such as polyethylene glycol, propylene glycol, ethanol, or polysorbate 80, which have been associated with adverse drug reactions in children.
“Vitamin E” is a common term for eight lipid-soluble compounds: α-, β-, γ-, and δ-tocopherol, and α-, β-, γ-, and δ-tocotrienol [6]. In humans, α-tocopherol is the most abundant form in plasma [7]. Vitamin E compounds differ in stereoisomerism, esterification, and biological activity (Table 1) [6, 8].
Vitamin E undergoes passive diffusion from the small intestine [7]. The absorption rates differ considerably between individuals, ranging from 20–60%, depending on pancreatic function, bile salts, concomitant fat intake, and product properties [6, 9–11]. Preceding absorption, vitamin E and food lipids form micelles in the presence of bile and bile salts. The vitamin E compound tocofersolan has both hydrophilic and lipophilic properties and may increase the bioavailability of fat-soluble vitamin E in individuals having a low degree of absorption [12]. The strength conversion factor (Table 1) for tocofersolan is, however, based on the tocopherol content of the molecule, regardless of bioavailability. Vitamin E is not transformed and is eliminated by fecal excretion or conjugation.
Our main aim was to review data on therapeutic use of and recommendations for oral vitamin E therapy in neonates and children.
Methods
To identify published studies, case reports, and information on therapeutic use of oral vitamin E in children, a literature search was carried out. Search terms in Medline OVID and EMBASE were Vitamin e.mp, exp Vitamin E/, tocofersolan.mp, or tpgs.mp; limited to human, all child (birth to 18 years) or child.mp; administration, oral or oral.mp; publication year 1980–February 2008. Publications on other aspects than therapy, such as supplements in formulas or total parenteral nutrition (TPN), were excluded. Only articles written in English or a Scandinavian language evaluating human subjects were considered.
Therapy recommendations and product properties were also found in handbooks, such as the British National Formulary for Children (BNF for Children) [13], Medicines for Children [14], Pediatric Dosage Handbook [11], Neonatal Drug Formulary [15], Neofax [16], product monographs, and formularies. In addition to the review of clinical studies on the use of oral vitamin E in children, data from the handbook recommendations are presented as well.
Results
As this review focused on oral vitamin E therapy in children, only studies including vitamin E doses, pharmacokinetics, and oral formulations were considered.
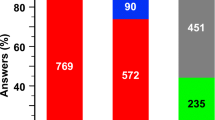
Clinical studies and case reports on oral vitamin E therapy in children are few and heterogeneous regarding the compounds being used, dosing, and indications. The majority of the studies included a small number of patients, and they rarely specified how doses were chosen, either for prophylaxis or for treatment of current deficiency. The exact name of the active substance was rarely stated. Information on the content of excipients was not always provided, and some studies did not describe the formulation at all. Consequently, overall statistical evaluations of dosing and formulation recommendations for both neonates and older children have not been feasible for this review.
Published data indicate that an esterified, synthetic racemic mixture, all-rac-α-tocopheryl acetate (formerly dl-α-tocopheryl acetate), and dl-α-tocopherol are commonly used in medicinal products (Table 2). A water-soluble form, tocofersolan, has also been used [5]. Tocofersolan contains RRR-α-tocopherol with polyethylene glycol 1000 succinate [8] and is also called “d-α-tocopheryl PEG 1000 succinate,” “d-α-tocopheryl polyethylene glycol succinate,” “TPGS,” and “vitamin E TPGS.”
Oral vitamin E in sick newborns and premature infants
In this patient category, oral vitamin E may be used for treatment or for prevention of vitamin E deficiency, anemia, or for prevention of ROP caused by oxygen therapy. However, the interpretation of data is limited by several factors, as the methodologies, choice of drugs and doses, outcomes, and ADR assessments have been less than optimal. Vitamin E was initiated as an oral formulation in only a few studies, and the doses were heterogeneous. A Cochrane review on vitamin E supplementation for prevention of morbidity and mortality in preterm infants included 26 published studies that fulfilled the Cochrane quality and entry criteria of primary and secondary outcomes analysis; infants with gestational age less than 37 weeks or birth weight less than 2,500 g were included [1]. Most studies were carried out with other administration forms, such as parenteral, intramuscular/intravenous, or parenteral in combination with oral. Eight of these studies refer to oral therapy alone and form the basis for our review in this patient category (Table 2).
No recent studies on vitamin E treatment in neonates were identified. The majority of the studies on oral vitamin E administration in neonates describe the use of α-tocopherol or α-tocopheryl acetate for prevention of anemia. Only one study addresses prevention of ROP [17]. For tocofersolan, we identified two small studies on the effect on bilirubin levels [18, 19].
It is worth noting the diversity of doses, indications, and choices of compounds in the studies. Vitamin E absorption may differ among formulations [10]. Existing studies on absorption were published several years ago, with suboptimal designs and products no longer available. Systematic, comparative dose-finding studies for any vitamin E compound within this patient group were not identified. Serum concentrations have been demonstrated to differ widely even after equal doses [20, 21].
Dosing recommendations and indications differ among handbooks (Table 3).
Oral vitamin E in children with liver or biliary tract disease
We did not identify any evidence-based review for these patient categories. The clinical studies and case reports have differing dosing approaches, choices of compound, and outcome parameters (Table 4).
Neonates and children with bile duct atresia or chronic intrahepatic cholestasis have insufficient bile secretion. Vitamin E treatment is therefore indicated due to reduced ability to dissolve dietary fat and vitamins. Serum concentrations may, however, still be lower than expected [22, 23]. Some studies describe the use of tocofersolan in children with obstructive bile disease [24, 63, 65, 66], and a medicinal product was recently approved by the European Medicines Agency under exceptional circumstances [67]. The total daily dose is stated as 17 mg/kg of d-alpha-tocopherol in the form of tocofersolan. Sokol and co-workers analyzed serum concentrations in 22 children with hepatic/biliary disease who had vitamin E deficiency [24]. All patients were switched from tocopheryl acetate to tocofersolan, and all of them needed a significant dose reduction in order to maintain the target serum concentration. On average, doses were reduced by 83% (range: 64.3–93.5%). A larger study from the same authors included 60 children aged 0.5–20 years. All children needed a dose reduction when tocopherol or tocopheryl acetate 70–200 IU kg−1 day−1 was replaced with tocofersolan 20–25 IU kg−1 day−1 [65]. Dose reductions of 40–77% are also described after changing from α-tocopherol to tocofersolan in children with biliary stasis [63, 66]. Despite the paucity of data, these results indicate that patients with absorption disturbances may need considerable dose reduction when treated with tocofersolan compared to α-tocopherol or α-tocopheryl acetate.
Dosage recommendations in handbooks range from “water-miscible vitamin E” 1 IU kg−1 day−1 [11] to 100–200 mg α-tocopheryl acetate/day [13] (Table 3).
Other indications for oral vitamin E therapy
Vitamin E has also been used in children with diseases such as abetalipoproteinemia (Table 3), cystic fibrosis [25–27] , β-thalassemia, sickle cell anemia [11, 13], inborn errors of metabolism [28], epidermolysis bullosa [29], glucose-6 phosphate dehydrogenase deficiency [30], and focal segmental glomerulosclerosis [31]. Many studies do not state the rationale for the dose size, and dosing regimes are not evaluated systematically. This is demonstrated by the cystic fibrosis studies in children. Doses differed among the studies: 5.5–47.4 IU kg−1 day−1, 5–10 mg kg−1 day−1, and 50–100 IU/day. The vitamin E compounds used in the studies were described as tocopheryl acetate, tocopherol, tocofersolan, or vitamin E. Despite this, dose recommendations are listed in handbooks (Table 3).
Recently, vitamin E has been studied in children with obesity-related liver disease [32–34]. Outcome parameters included changes in laboratory findings such as aminotransferases and alkaline phosphatase (ALP). A cohort study of 11 children aged 8.3–14.3 years found a normalization of serum aminotransferase and ALP after treatment [32]. However, two other studies, including 28 and 90 children, respectively, found diet and/or exercise to be more efficient than vitamin E therapy alone [33, 34].
Dosing implications for co-administration with other drugs
Tocopherol/tocopheryl acetate and tocofersolan appear to differ in their potential for drug interactions. Tocofersolan may increase the bioavailability of other drugs, such as amprenavir [35], paclitaxel [36], vancomycin [37], and cyclosporine [38], due to its combined lipophilic and hydrophilic nature. In children with a liver transplant, tocofersolan has been found to increase cyclosporine serum concentrations significantly [39]. This may increase the risk of ADRs when tocofersolan and cyclosporine are used simultaneously [40]. Some studies suggest that vitamin E may increase the risk of hemorrhages due to reduction of prothrombin levels and may affect platelet function, particularly in patients with vitamin K deficiency, such as neonates with sepsis, or in patients treated with antithrombotic medicines such as warfarin and acetylsalicylic acid [13, 41, 42]. Decreased vitamin E plasma levels have been reported after use of phenobarbital and phenytoin [43]. Drugs that interfere with the reuptake of bile acids may reduce the uptake of fat-soluble vitamins such as vitamin E [44].
Handbook information on drug interactions with vitamin E is not consistent, and the information differs among books and other literature.
Discussion
Overall, the body of evidence was limited due to the small number of studies. The lack of supportive information on oral vitamin E dosing recommendations in children is a major concern. This review shows that oral vitamin E dosing regimens for children differ considerably, and few randomized clinical trials have been published. Information on vitamin E pharmacokinetics in children is lacking, and data regarding doses, compounds, and outcome parameters are heterogeneous. There are no existing evaluations of dose–effect relationships, therapeutic windows, safety profiles, and optimum duration of therapy for the various vitamin E compounds across age groups or disease states. Many studies incorporate various forms of vitamin E therapy in their treatment of neonates and older children, such as oral, intravenous, and intramuscular administration and as supplement in total parenteral nutrition. Consequently, there is very little documentation to support an evidence-based choice of oral therapeutic dose or compound.
Vitamin E compounds may differ in biological activity and bioavailability. Most clinical data in children are available for α-tocopherol or tocopherol esters, such as α-tocopheryl acetate. While a tocofersolan product recently received a marketing authorization in the EU for use in children with cholestasis, this product is contraindicated in premature infants. In newborns, most evaluations on efficacy and safety are based on studies with intravenous or intramuscular tocopheryl acetate. Assessment on the risk/benefit profile has not yet been done for oral vitamin E in neonates and children.
Tocofersolan may have increased bioavailability compared to other vitamin E compounds. This has resulted in therapeutic serum levels despite considerable dose reductions when switching from tocopheryl acetate in children with malabsorption diseases [24, 65]. Conversely, absorption of tocopheryl acetate in healthy adults may be similar or even superior to tocofersolan [45]. A change of therapy from α-tocopheryl acetate to tocofersolan may have consequences for dosing recommendations and the ADR profile, but it is not known whether this is the case for all patient groups or whether differences in intestinal absorption are less pronounced in infants without malabsorption disorders. The pharmacokinetic properties of tocofersolan indicate that therapeutic monitoring may be advisable in children to avoid adverse reactions.
The relative biological activities of vitamin E compounds have been determined by a rat model, founded on the fact that vitamin E depletion after conception causes death and embryo resorption [6]. However, the rat model cannot be used to detect differences in biological activity or bioavailability in immature, human intestines, such as in premature babies, sick neonates, or in patients with gastrointestinal disturbances. To our knowledge, the mg/IU ratio for tocofersolan is based on a calculation of the tocopherol content of the molecule and not the bioavailability of the molecule.
Toxicity and ADRs, such as sepsis, NEC, and hemorrhages have been reported after vitamin E therapy [1]. The risk of such events appears to be associated with low birth weight and serum levels above 3.5 mg/dL. No follow-up studies in neonates or older children have been found.
Some oral vitamin E products may contain excipients, such as polyethylene glycol, propylene glycol, ethanol, or polysorbate 80, which have been associated with ADRs in children. Few vitamin E products have a marketing authorization for oral administration in children. Therefore, extempore pharmacy compounding may be the only option. There are, however, few product specifications. In the 1980s, reports of deaths and serious ADRs, including thrombocytopenia and kidney and liver failure, were linked to the use of an intravenous vitamin E product [46] and may have been caused by dose-related toxicity of α-tocopherol, the emulsifier polysorbate or both. Oral administration of vitamin E has been associated with an increased risk of NEC, possibly related to dose, polysorbate content, or hyperosmolar products [47]. The polyethylene glycol component of tocofersolan may put children at risk as it accumulates in patients with immature kidneys [65]. In Norway, an extempore formulation containing 20% alcohol, originally intended for veterinary use, has been widely used “off-label” in neonates and older children [5]. The alcohol content of 60 mg 96% ethanol per 15 mg tocopheryl acetate in a 1,000-g premature baby is equivalent to 10 mL 45% ethanol in a 70-kg adult. While data on pediatric alcohol exposure due to excipients are limited, there is a potential risk of adverse effects, especially in neonates and premature infants [48].
Several handbooks carry a warning for hyperosmolar products. However, information on the osmolality of the various pharmacy-compounded products is not provided.
The choice of formulation should be based on the principle of suitability for the most vulnerable patients (premature neonates), degree of documentation for pediatric patients, pharmacokinetic predictability/reliability, and suitable strengths for the intended patient groups. The most obvious factor for achieving a suitable formulation would be to keep the content of alcohol and other excipients to a minimum and to make a critical appraisal of the need for each ingredient.
Regarding the active ingredient, both tocopheryl acetate and tocofersolan have advantages and disadvantages. Using tocofersolan eliminates the need for ethanol. In some patients, the bioavailability may be more predictable. The disadvantages of tocofersolan are the lack of documentation, unclarified dosage equivalency, and presence of polyethylene glycol.
Two different formulations may be necessary, due to the differences in doses between premature neonates and school-age hepatobiliary patients/post-liver transplant children. Increasing doses with age may necessitate increasing strengths and corresponding increases in alcohol content to increase the solubility. This would represent a lesser problem in older children than in the smallest ones. Sick neonates having septicemia and other concurrent diseases have several battles to fight. The metabolic pathways for drugs are under development (transition from intrauterine to extrauterine life), they have reduced capacity for drug metabolism, and ultimately the degree of the disease may affect drug metabolism to a greater extent at this time than for older children.
In summary, the evidence regarding the use of oral vitamin E in children is limited and largely of poor methodological quality. Several types of studies are needed. A survey study would increase our knowledge of current therapeutic practice. The objective should be to discover to what extent vitamin E is being used for neonates and older children in European countries, the U.S.A., and Japan, for which patient groups, and which products and doses are the most commonly used. In addition, indications for prescribing the particular drug, existing guidelines in hospitals, and the basis for existing practice could be examined. Furthermore, there is a need for well-designed pharmacokinetic studies including different formulations of tocopherol, tocopheryl acetate, and tocofersolan. The studies should include relevant patient groups such as premature neonates, patients with congenital bile atresia before and after surgical therapy, and children after liver transplantation.
At present, most clinical data refer to tocopheryl acetate. Randomized, controlled trials should be done to examine the optimum doses and therapeutic equivalency of tocopherol/tocopheryl acetate and tocofersolan. There are, however, certain methodological challenges regarding choice of treatment and control groups. When treatment is regarded as essential, placebo controls would be unethical. To our knowledge some hospitals in Europe do not include oral vitamin E treatment in, e.g., neonates on respirators or those on oxygen therapy. Consequently, it would be possible to do comparative studies. Comparison of different therapy regimens with the various forms of vitamin E might be a possible option in children already on therapy. Other options include case series from hospitals or cohort studies, depending on the information desired. Comparisons of patients from two hospitals with different treatment regimens would have to be examined carefully due to possible confounding factors. Data collection from patients who currently receive an oral vitamin E product, including therapeutic monitoring, would be the most readily available method to gather readily accessible material. When a clinical, comparative study is feasible, we would suggest monitoring outcome parameters as analyzed in the Cochrane metaanalysis with primary outcomes being mortality/survival and long-term morbidity, and secondary outcomes being bronchopulmonary dysplasia, patent ductus arteriosus, sepsis, ROP, NEC, hemoglobin, bilirubin, platelets, and coagulation parameters. Visual assessments at 3 and 6 months should be included.
Conclusions
Oral vitamin E compounds have been used for decades to treat a number of conditions in children. There are few data to suggest solid guidelines on oral vitamin E therapy. The present data do not provide sufficient evidence of dosing and products to make recommendations for oral vitamin E use in children. Most data are available on therapeutic use of α-tocopherol or tocopherol esters, such as α-tocopheryl acetate.
There are no systematic safety data or documentation on long-term effects. Extensive use of oral vitamin E in premature infants and neonates solely for prophylactic purposes needs to be evaluated. Systematic evaluations based on clinical trials would be a better foundation for therapeutic use in premature infants and neonates, regarding both indication for therapy and prevention. Further research, including comparative, dose-finding studies, is required to ensure evidence-based dosing recommendations for neonates and older children.
Abbreviations
- ADR(s):
-
Adverse drug reaction(s)
- ALP:
-
Alkaline phosphatase
- BPD:
-
Bronchopulmonary dysplasia
- NEC:
-
Necrotizing enterocolitis
- PEG:
-
Polyethylene glycol
- ROP:
-
Retinopathy of prematurity
- TPGS:
-
Tocopheryl polyethylene glycol succinate
- TPN:
-
Total parenteral nutrition
- BNF:
-
British National Formulary
References
Brion LP, Bell EF, Raghuveer TS (2003) Vitamin E supplementation for prevention of morbidity and mortality in preterm infants. Cochrane Database Syst Rev 4:CD003665. doi:10.1002/14651858.CD003665
Conroy S, Choonara I, Impicciatore P et al (2000) Survey of unlicensed and off label drug use in paediatric wards in European countries. European Network for Drug Investigation in Children. Br Med J 320:79–82
Brion F, Nunn AJ, Rieutord A (2003) Extemporaneous (magistral) preparation of oral medicines for children in European hospitals. Acta Paediatr 92:486–490
Conroy S (2003) Extemporaneous (magistral) preparation of oral medicines for children in European hospitals. Acta Paediatr 92:408–410
Westergren T, Kalikstad B (2006) Liquid vitamin E for children: treatment with a blindfold? Tidsskr Nor Laegeforen 126:902–904
Eitenmiller R, Lee J (2004) Vitamin E: chemistry and biochemistry. In: Vitamin E Food chemistry, composition and analysis. Marcel Dekker, New York, pp 2–5
Roxborough HE, Burton GW, Kelly FJ (2000) Inter- and intra-individual variation in plasma and red blood cell vitamin E after supplementation. Free Radic Res 33:437–445
Eastman (2008) Eastman vitamin E TPGS, food grade. http://www.eastman.com Accessed May 20, 2008
Jeanes YM, Hall WL, Ellard S et al (2004) The absorption of vitamin E is influenced by the amount of fat in a meal and the food matrix. Br J Nutr 92:575–579
Jansson L, Lindroth M, Työppönen J (1984) Intestinal absorption of vitamin E in low birth weight infants. Acta Paediatr Scand 73:329–332
Taketomo CK, Hodding JH, Kraus DM (2007) Pediatric dosage handbook, 14th ed. Lexi-Comp, Hudson, OH, pp 1620–1622
Brigelius-Flohé R, Kelly FJ, Salonen JT et al (2002) The European perspective on vitamin E: current knowledge and future research. Am J Clin Nutr 76:703–716
BMJ Publishing Group (2007) BNF for children. London, p 549
RCPCH Publications (2003) Medicines for children. London, pp 670–671
Bhatt D, Reber DJ, Wirtschafter DD et al (1997) Neonatal drug formulary. Fontana, CA, pp 432–433
Young TE, Mangum B (2008) NeoFax. Thomson Reuters, Montvale, NJ, p 286
Hittner HM, Godio LB, Rudolph AJ et al (1981) Retrolental fibroplasia: efficacy of vitamin E in a double-blind clinical study of preterm infants. N Engl J Med 305:1365–1371
Fischer AF, Inguillo D, Martin DM et al (1987) Carboxyhemoglobin concentration as an index of bilirubin production in neonates with birth weight less than 1,500 grams: a randomized double-blind comparison of supplemental oral vitamin E and placebo. J Pediatr Gastroenterol Nutr 6:748–751
Smith DW, Cohen RS, Vreman HJ et al (1985) Bilirubin production after supplemental oral vitamin E therapy in preterm infants. J Pediatr Gastroenterol Nutr 4:38–44
Friedman CA, Wender DF, Temple DM et al (1988) Serum alpha-tocopherol concentrations in preterm infants receiving less than 25 mg/kg/day alpha-tocopherol acetate supplements. Dev Pharmacol Ther 11:273–280
Neal PR, Erickson P, Baenziger JC et al (1986) Serum vitamin E levels in the very low birth weight infant during oral supplementation. Pediatrics 77:636–640
Issa S, Rotthauwe HW, Burmeister W (1989) 25 hydroxyvitamin D and vitamin E absorption in healthy children and children with chronic intrahepatic cholestasis. Eur J Pediatr 148:605–609
Guggenheim MA, Ringel SP, Silverman A et al (1982) Progressive neuromuscular disease in children with chronic cholestasis and vitamin E deficiency: diagnosis and treatment with alpha tocopherol. J Pediatr 100:51–58
Sokol RJ, Heubi JE, Butler-Simon N et al (1987) Treatment of vitamin E deficiency during chronic childhood cholestasis with oral d-α-tocopheryl polyethylene glycol-1000 succinate. Gastroenterology 93:975–985
Feranchak AP, Sontag MK, Wagener JS et al (1999) Prospective, long-term study of fat-soluble vitamin status in children with cystic fibrosis identified by newborn screen. J Pediatr 135:601–610
Winklhofer-Roob BM, van’t Hof MA, Shmerling DH (1996) Long-term oral vitamin E supplementation in cystic fibrosis patients: RRR-α-tocopherol compared with all-rac-α-tocopheryl acetate preparations. Am J Clin Nutr 63:722–728
Wilfond BS, Farrell PM, Laxova A et al (1994) Severe hemolytic anemia associated with vitamin E deficiency in infants with cystic fibrosis. Clin Pediatr (Phila) 33:2–7
Moyano D, Vilaseca MA, Pineda M et al (1997) Tocopherol in inborn errors of intermediary metabolism. Clin Chim Acta 263:147–155
Shirakata Y, Shiraishi S, Sayama K et al (1993) High-dose tocopherol acetate therapy in epidermolysis bullosa siblings of the Cockayne-Touraine type. J Dermatol 20:723–725
Eldamhoughy S, Elhelw Z, Yamamah G et al (1988) The vitamin E status among glucose-6 phosphate dehydrogenase deficient patients and effectiveness of oral vitamin E. Int J Vitam Nutr Res 58:184–188
Tahzib M, Frank R, Gauthier B et al (1999) Vitamin E treatment of focal segmental glomerulosclerosis: results of an open-label study. Pediatr Nephrol 13:649–652
Lavine JE (2000) Vitamin E treatment of nonalcoholic steatohepatitis in children: a pilot study. J Pediatr 136:734–738
Vajro P, Mandato C, Franzese A et al (2004) Vitamin E treatment in pediatric obesity-related liver disease: a randomized study. J Pediatr Gastroenterol Nutr 38:48–55
Nobili V, Manco M, Devito R et al (2006) Effect of vitamin E on aminotransferase levels and insulin resistance in children with non-alcoholic fatty liver disease. Aliment Pharmacol Ther 24:1553–1561
Yu L, Bridgers A, Polli J et al (1999) Vitamin E-TPGS increases absorption flux of an HIV protease inhibitor by enhancing its solubility and permeability. Pharm Res 16:1812–1817
Mu L, Feng SS (2003) A novel controlled release formulation for the anticancer drug paclitaxel (Taxol). J Control Release 86:33–48
Prasad YVR, Puthli SP, Eaimtrakarn S et al (2003) Enhanced intestinal absorption of vancomycin with Labrasol and D-α-tocopheryl PEG 1000 succinate in rats. Int J Pharm 250:181–190
Chang T, Benet LZ, Hebert MF (1996) The effect of water-soluble vitamin E on cyclosporine pharmacokinetics in healthy volunteers. Clin Pharmacol Ther 59:297–303
Sokol RJ, Johnson KE, Karrer FM et al (1991) Improvement of cyclosporine absorption in children after liver transplantation by means of water-soluble vitamin E. Lancet 338:212–214
Holt DW, Johnston A (1991) Cyclosporine and vitamin E. Lancet 338:697
Helsing E (2000) Vitamins. In: Dukes MNG, Aronson JK (eds) Meyler’s side effects of drugs, 14th ed. Elsevier, Amsterdam, pp 1354–1356
Liede KE, Haukka JK, Saxen LM et al (1998) Increased tendency towards gingival bleeding caused by joint effect of alpha-tocopherol supplementation and acetylsalicylic acid. Ann Med 30:542–546
Higashi A, Ikeda T, Matsukura M et al (1982) Serum zinc and vitamin E concentrations in handicapped children treated with anticonvulsants. Dev Pharm Ther 5(3–4):109–113
Gold Standard (2009) Vitamin E. http://www.clinicalpharmacology.com. Accessed May 28, 2009
Dimitrov NV, Meyer-Leece C, McMillan J et al (1996) Plasma α-tocopherol concentrations after supplementation with water- and fat-soluble vitamin E. Am J Clin Nutr 64:329–335
Balistreri WF, Farrell MK, Bove KE (1986) Lessons from the E-Ferol tragedy. Pediatrics 78:503–506
Mino M (1989) Use and safety of elevated dosages of vitamin E in infants and children. Int J Vitam Nutr Res 30:69–80
Inoue N (2004) Iatrogenic alcohol in medication. Clin Pediatr (Phila) 43:399–400
Ferlin MLS, Chuan LS, Jorge SM et al (1998) Early anemia of prematurity. Nutr Res 18:1161–1173
Jansson L, Holmberg L, Nilsson B et al (1978) Vitamin E requirements of preterm infants. Acta Paediatr Scand 67:659–663
Melhorn DK, Gross S, Childers G (1971) Vitamin E-dependent anemia in the premature infant. I. Effects of large doses of medicinal iron. J Pediatr 79:569–580
Pathak A, Roth P, Piscitelli J et al (2003) Role of vitamin E supplementation during erythropoietin treatment of the anemia of prematurity. Arch Dis Child Fetal Neonatal Ed 88:F324–F328
Zipursky A, Brown EJ, Watts J et al (1987) Oral vitamin E supplementation for the prevention of anemia in premature infants: a controlled trial. Pediatrics 79:61–68
Chowers I, Banin E, Merin S et al (2001) Long-term assessment of combined vitamin A and E treatment for the prevention of retinal degeneration in abetalipoproteinaemia and hypobetalipoproteinaemia patients. Eye 15:525–530
Clark JH, Nagamori KE, Ellett ML et al (1985) Vitamin E sufficiency in children with cholestasis: a comparison between erythrocyte peroxide hemolysis and serum α-tocopherol. Clin Chim Acta 153:117–124
Guggenheim MA, Ringel SP, Silverman A et al (1982) Progressive neuromuscular disease in children with chronic cholestasis and vitamin E deficiency: clinical and muscle biopsy findings and treatment with α-tocopherol. Ann N Y Acad Sci 393:84–93
Hegele RA, Angel A (1985) Arrest of neuropathy and myopathy in abetalipoproteinemia with high-dose vitamin E therapy. Can Med Assoc J 132:41–44
Lubrano R, Frediani T, Citti G et al (1989) Erythrocyte membrane lipid peroxidation before and after vitamin E supplementation in children with cholestasis. J Pediatr 115:380–384
Muller DPR, Lloyd JK, Wolff OH (1985) The role of vitamin E in the treatment of the neurological features of abetalipoproteinaemia and other disorders of fat absorption. J Inherit Metab Dis 8(Suppl.1):88–92
Nakagawa M, Tazawa Y, Kobayashi Y et al (1984) Familial intrahepatic cholestasis associated with progressive neuromuscular disease and vitamin E deficiency. J Pediatr Gastroenterol Nutr 3:385–389
Roma E, Klontza D, Kairis M et al (1984) Familial hypobetalipoproteinaemia. Helv Paediatr Acta 39:145–151
Roongpraiwan R, Suthutvoravut U, Feungpean B et al (2002) Effect of oral vitamin E supplementation in children with cholestasis. J Med Assoc Thai 8(Suppl 4):1199–1204
Socha P, Koletzko B, Pawlowska J et al (1997) Treatment of cholestatic children with water-soluble vitamin E (alpha-tocopheryl polyetylene glycol succinate): effects on serum vitamin E, lipid peroxides and polyunsaturated fatty acids. J Pediatr Gastroenterol Nutr 24:189–193
Sokol RJ, Guggenheim M, Iannacone S et al (1985) Improved neurologic function after long-term correction of vitamin E deficiency in children with chronic cholestasis. N Engl J Med 313:1580–1586
Sokol RJ, Butler-Simon N, Conner C et al (1993) Multicenter trial of d-α-tocopheryl polyethylene glycol 1000 succinate for treatment of vitamin E deficiency in children with chronic cholestasis. Gastroenterology 104:1727–1735
Traber MG, Kayden HJ, Balmer Green J et al (1986) Absorption of water miscible forms of vitamin E in a patient with cholestasis and in thoracic duct-cannulated rats. Am J Clin Nutr 44:914–923
European Medicines Agency (EMEA) (2009) Vedrop. European Public Assessment Report, 29. May 2009. http://www.emea.europa.eu
Acknowledgements
We thank professor Thor Willy Ruud Hansen at the University of Oslo, Section on Neonatology, Oslo University Hospital, Rikshospitalet, Oslo, Norway, for valuable feedback on the manuscript.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Westergren, T., Kalikstad, B. Dosage and formulation issues: oral vitamin E therapy in children. Eur J Clin Pharmacol 66, 109–118 (2010). https://doi.org/10.1007/s00228-009-0729-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-009-0729-1