Abstract
Purpose
To test an intervention bundle for thirst intensity, thirst distress, and dry mouth, which are among the most pervasive, intense, distressful, unrecognized, and undertreated symptoms in ICU patients, but for which data-based interventions are lacking.
Methods
This was a single-blinded randomized clinical trial in three ICUs in a tertiary medical center in urban California. A total of 252 cognitively intact patients reporting thirst intensity (TI) and/or thirst distress (TD) scores ≥3 on 0–10 numeric rating scales (NRS) were randomized to intervention or usual care groups. A research team nurse (RTN#1) obtained patients’ pre-procedure TI and TD scores and reports of dry mouth. She then administered a thirst bundle to the intervention group: oral swab wipes, sterile ice-cold water sprays, and a lip moisturizer, or observed patients in the usual care group. RTN#2, blinded to group assignment, obtained post-procedure TI and TD scores. Up to six sessions per patient were conducted across 2 days.
Results
Multilevel linear regression determined that the average decreases in TI and TD scores from pre-procedure to post-procedure were significantly greater in the intervention group (2.3 and 1.8 NRS points, respectively) versus the usual care group (0.6 and 0.4 points, respectively) (p < 0.05). The usual care group was 1.9 times more likely than the intervention group to report dry mouth for each additional session on day 1.
Conclusion
This simple, inexpensive thirst bundle significantly decreased ICU patients’ thirst and dry mouth and can be considered a practice intervention for patients experiencing thirst.
Similar content being viewed by others
Introduction
Thirst is a perception that provokes the urge to drink fluids [1]. It is a multidimensional symptom that is described in terms of intensity and distress and is sometimes associated with dry mouth [2], termed xerostomia [3]. Thirst is poorly recognized in intensive care unit (ICU) practice [4, 5]. Yet, research has identified it as one of the most pervasive, intense, and undertreated symptoms in ICU patients [6, 7]. Over 70 % of ICU cancer patients reported unsatisfied thirst at the highest levels of intensity [8], and almost all chronically, critically ill patients in a hospital-based respiratory care unit reported moderate or severe thirst [9]. Of 405 symptom assessments completed by 171 ICU patients, thirst was reported in 70 % of patient assessments, and it was rated as more intense than fatigue, anxiety, restlessness, hunger, dyspnea, pain, sadness, fear, and confusion [10]. The rationale for developing and testing an effective thirst relief intervention is provided by the basic compassionate care tenet that ICU patients’ symptoms should be palliated [11].
No previous study of ICU patients provides empirical guidance on thirst relief during critical illness [6]. Protocols for mouth care in ICU patients [12, 13], including those for ventilator-associated pneumonia (VAP) prevention [14], have eliminated the use of lemon–glycerin swabs because they produce an acid pH [15], dry oral tissues [16], cause irreversible softening and erosion of tooth enamel [17], exhaust salivary mechanisms, and worsen xerostomia [18]. Artificial saliva substitutes are ineffective for relieving dry mouth [19]. There is no research basis for ice chips being effective for relief of thirst or dry mouth, and ice chips are contraindicated for many critically ill patients.
Prior research evaluating individual topical measures to relieve thirst or dry mouth in healthy subjects or non-ICU patients suggested the effectiveness of sprays of cold sterile water from squirt bottles [20–22], swabs of cold sterile water [23–26], and a menthol moisturizer [21, 27]. Cold water satiates thirst more effectively than body temperature water [28] and is preferred because it offers greater relief from mouth dryness [24, 29]. Cold water also may stimulate greater saliva production than warmer water [21, 25], which may, in turn, alleviate mouth dryness [25]. Sprays of water from plastic squirt bottles and swabs to moisten the mouth and tongue have been previously shown to be effective for heart failure patients experiencing thirst from fluid restriction [22]. Like cold water, menthol stimulates sensory cold receptors in the mouth by increasing nerve discharge from cold receptors [27]. In the present study, we tested whether combining these measures as an “intervention bundle,” focusing specifically on ICU patients, would effectively reduce thirst intensity (TI) and thirst distress (TD). The comparison group received usual care, i.e., the day-to-day care (i.e., monitoring and management) provided by patients’ clinicians as part of usual practice.
Two hypotheses were tested:
-
Hypothesis 1
Thirst intensity and thirst distress will decrease significantly more from pre-procedure to post-procedure in ICU patients who receive a thirst intervention compared to those who receive usual care.
-
Hypothesis 2
Dry mouth will decrease significantly in ICU patients who receive a thirst intervention bundle compared to those who receive usual care.
Materials and methods
Site and sample
This study was conducted as a single-blinded, longitudinal randomized clinical trial. We tested the intervention in each patient for up to six times to determine the effect at each of several time periods. We report our findings guided by the Consolidated Standards Of Reporting Trials (CONSORT) statement for randomized trials of nonpharmacological treatment [30]. Patients were recruited from medical-surgical, neurological, and cardiovascular ICUs in a tertiary medical center in urban California (77 adult beds.) Although each ICU serves different populations, they follow uniform practice standards. Inclusion criteria were age ≥18 years; ICU stay ≥24 h; English proficient; oriented to name, date of birth, and location; a Richmond Agitation Sedation Scale (RASS) [31] score of −1 to +1 (i.e., not sedated or agitated); and either a TI or TD score of ≥3 on a 0–10 numeric rating scale (NRS), which was assessed at the time of screening. Exclusion criteria were open sores or desquamation on the mouth or lips, a history of dementia, or a medical condition that contraindicated the intervention (e.g., oral surgery). Since thirst could occur in patients unrelated to nil per os (NPO) status, patients were enrolled in the study regardless of whether they were allowed fluids by mouth. All research team members were trained extensively on the procedures and systematically observed for protocol compliance.
Pre-screening for thirst
A research team nurse (RTN) used NRSs (0–10) to obtain patient thirst ratings at baseline and during subsequent assessments. The NRS has been widely used to assess pain intensity and other symptoms; has face, construct, and concurrent validity [32]; and is feasible for use in ICUs. To measure TI, the RTN asked the patient, “how intense is your thirst, on this scale, where 0 = no thirst and 10 = worst possible thirst?” To measure TD, the RTN asked, “how distressing [or bothersome] is your thirst, on this scale, where 0 = no distress and 10 = very distressing?” For patients unable to communicate orally owing to endotracheal intubation, the RTN held up a laminated sheet showing the NRS and/or asked the patient to nod affirmatively when she pointed to the number that corresponded to their TI or TD. Independent scoring by two RTNs for 50 assessments was initially compared to assure inter-rater reliability. Patients who met eligibility criteria were invited to participate in the study. Approval was obtained from the institutional review board at the study institution, and informed consent was obtained for all participants, either directly or through an appropriate surrogate.
Study protocol
Patients received either the intervention or usual care according to randomization by the RTN enrolling the patient (RTN#1) by a code drawn from an envelope. The study procedure occurred during three 15-min sessions per day for 2 days, conducted between 10 a.m. and 6 p.m. up to 7 days per week. There was a minimum of 30 min between each of the three sessions; the maximum time between sessions varied as a factor of other patient care activities. RTN#1 and a second RTN who was blinded to group assignment, RTN#2, worked together to implement the study procedure.
The detailed study protocol is in Supplemental Table 1. In brief, pre-procedure TI and TD scores were obtained at the beginning of each session, and patients were asked whether their mouth felt dry. Assessment was done to determine if the patient had stickiness or dryness in the mouth or around lips; had split skin at the corners of the mouth; or cracked lips. Intervention group patients then received the thirst bundle: oral swabs and water sprays, and menthol moisturizer applied to the patient’s lips. The full intervention was delivered in 15 min. Patients in the usual care group were observed for a 15-min period. RTN#1 did not interfere with the patients’ normal nursing activities. Immediately after each 15-min session, RTN#2, blinded to the patient’s pre-procedure thirst scores and group allocation (intervention materials were removed from the room), was called to the patient’s bedside by RTN#1. RTN#2 obtained the patients’ post-procedure TI and TD scores. After a minimum of 30 min, this procedure was repeated twice on day 1 and up to three sessions on day 2, if the patient remained in ICU. Patient participation ended when they were transferred from the unit or when two RTNs were not available on day 2. All enrolled patients contributed data to the analyses. Data collection began in April 2010 and ended in June 2012.
Demographic and clinical characteristics of patients such as age, gender, laboratory values, medications, and first 24 h APACHE II score [33] were abstracted from the medical record on the study day. Safety monitoring of the intervention was performed to ensure that the intervention had no adverse effect on patients. An interim analysis showed no increase in thirst, so the study protocol was continued.
Statistical analyses
Statistical results are expressed as numerical values and percentages for categorical variables and as means, standard deviations (SD), medians, and first and third quartiles [Q1; Q3] for continuous variables. Comparisons were based on the χ 2 test for categorical data and on the t test for continuous data. Multilevel linear regression (MLR) with random intercepts was used to test hypothesis 1, that TI and TD will decrease significantly more from pre-procedure to post-procedure in ICU patients who receive a thirst intervention compared to those who receive usual care [34, 35]. This approach, unlike ANOVA, allows for missing data on the dependent variable (i.e., when patients did not complete all six sessions) as well as unbiased estimates of both fixed and random effects. MLR is also an appropriate analytical method when observations are non-independent. In a two-level linear mixed models design (multilevel regression model), repeated measures are at level one, and individuals (“clusters”) are at level two.
Group assignment (intervention or usual care) was the between-subjects factor. Our hypothesis 1 tested the difference between groups in average TI and TD scores from pre- to post-procedure. However, in preliminary analyses of the full factorial model, we tested three within-subjects factors: (1) the difference between groups for the pre- to post-procedure TI and TD scores, (2) the difference between groups due to session order, and (3) the difference between groups for day 1 compared to day 2. The “sessions” and “days” factors were of secondary interest but were examined to determine whether the pre- to post-procedure effect of the intervention was influenced by multiple interventions (i.e., three per day), and/or whether the effect of the intervention differed if it was given on two sequential days. Supplementary Table 2 provides a detailed explanation of statistical methods used in this study as well as their rationale. A power analysis determined that at least 69 patients should remain in each group at the end of the treatment period, for a total of 138. Anticipating attrition due to patient transfers and other clinical reasons, we chose to enroll 252.
For hypothesis 2, multilevel logistic regression was used to determine if there was a change in the odds that patients would experience dry mouth across sessions and, if so, whether the change differed according to the presence of the thirst intervention. This analysis focused on day 1 because there were more assessments on day 1 than day 2. The difference between groups in dry mouth was analyzed by multilevel logistic regression using Stata/SE for Windows® release 12 because of the superiority of this estimation method compared to the SPSS method.
Additional statistical analyses (χ 2, t tests, and multilevel logistic regression) were performed post hoc to further explore the meaning of results. Specifically, differences between groups were analyzed for fluid consumption, NPO orders, oral care practices, and the specific ICU (medical-surgical, neurovascular, cardiovascular) in which patients were located. All data were de-identified and double entered into IBM Statistical Package for the Social Sciences (SPSS) for Windows® version 20 (Armonk, NY, 2011).
Results
A total of 1,417 patients were screened for TI and TD, 950 patients met eligibility criteria, and 252 provided informed consent (see Fig. 1 for CONSORT diagram). Patients were randomized to the intervention group (n = 127) and the usual care group (n = 125). There were few statistically significant differences in demographic, clinical, and biological characteristics between the two groups (Table 1).
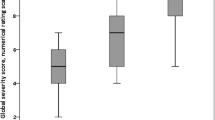
Results from the preliminary analysis of the full factorial MLR model showed that the potentially confounding influences of session order and day were not significant; i.e., they did not influence the individual differences between the intervention and the usual care groups’ thirst scores from pre-procedure to post-procedure (the between-subjects effect.) Therefore, for parsimony, these nonsignificant effects were removed, and the model was rerun in order to focus on hypothesis 1, i.e., the mean change in pre- to post-procedure thirst scores for the two groups. Decreases in pre- to post-procedure TI and TD scores were significantly greater in the intervention group than in the usual care group (p < 0.01), in both the full factorial model and in the more parsimonious model, from which the results are reported. Specifically, TI scores in the intervention group decreased 2.3 points, on average, while scores in the usual care group decreased 0.6 points, on average. TD scores in the intervention group decreased 1.8 points, on average, while scores in the usual care group decreased 0.4 points, on average. Differences in TI and TD, based on the multilevel regression analyses, are shown in Table 2. Table 3 shows the pre- and post-procedure mean thirst scores in both groups across the 2 days, and Supplemental Figs. 2 and 3 show scores at each session.
Patients were able to differentiate thirst from dry mouth. Table 4 presents the odds of patients in the intervention and usual care groups reporting dry mouth across sessions. MLR showed that the usual care group was 1.9 times more likely to report dry mouth compared to the intervention group for each additional assessment (p < 0.04).
No group differences were found regarding oral care practices and ICU assignment. Nor was there a significant difference between groups in total amount of fluids received during the 24-h period (Table 1). However, significantly more patients in the intervention group had an NPO order (35 versus 22 %, respectively, p = 0.02). Furthermore, significantly fewer patients in the intervention group received oral fluids during the 24-h period and study sessions (65 versus 77 %, respectively, p = 0.03).
Discussion
Amelioration of thirst has not previously been a research focus in ICU patients despite documentation that thirst is a prevalent and intense symptom. In this study, we tested a safe, simple, and inexpensive three-part intervention bundle for ICU patients experiencing thirst. Measured on a 0–10 NRS, the intervention decreased TI by 2.3 points and TD by 1.8 points from pre- to post-procedure regardless of the number of sessions or days in which patients participated. That is, the intervention was effective at each of the six sessions. While not previously examined in thirst research, this degree of difference exceeds the “minimally clinically significant” criterion of 1.7 points on an NRS determined in pain research [36]. Thus, these decreases in thirst can be considered both statistically and clinically significant. Furthermore, using criteria developed for pain responses [37], TI and TD scores decreased from “moderate” (NRS scores from 5 to 6) to “minimal” levels (i.e., NRS scores from 1 to 4).
Lower TI and TD scores occurred in the intervention group in spite of the fact that fewer received oral fluids; however, the total amount of fluids received in a 24-h period was not significantly different between groups. Also, more thirst intervention patients had a decrease in dry mouth than usual care patients.
The three-part thirst intervention was developed from individual, research-based treatments found to be effective in healthy subjects or patients outside of ICUs. To our knowledge, these treatments had not been tested in ICU patients or evaluated as a bundle, either in ICU patients or any other patient group. Data from the present study showed that combining the individual thirst treatments in our bundled intervention helped relieve thirst and dry mouth, which cause distress for many ICU patients.
The positive effect of the intervention that we tested is consistent with physiologic data showing that thirst relief is independent of swallowing and gastric distention but, rather, appears to be mediated by inhibition of vasopressin secretion through cold-sensitive oropharyngeal receptors [23]. This process of thirst relief has been termed “preabsorptive satiety” [21, p. 30] or inhibition of thirst by actions in the oropharynx itself [24]. While oropharyngeal stimulation/satiety from sprays of cold water may help explain the reduction in thirst found in intervention patients, symptom relief through oropharyngeal stimulation was not independently investigated. Still, this thirst intervention, which does not require swallowing fluids that reach the stomach, seems suitable for many ICU patients who are not permitted to or unable to swallow oral fluids. Preabsorptive satiety may also be influenced by menthol owing to the menthol’s cooling sensation, and the peppermint odor of menthol may be perceived as pleasant [21].
This study has limitations. Our recruitment rate was modest, perhaps owing the patients’ extreme tiredness or stress caused by their illness and/or multiple ICU events. However, a heterogeneous sample of over 250 patients was enrolled. Second, the proportion of mechanically ventilated (MV) patients was small, primarily because of sedation levels which limited patient ability to report thirst scores. Yet, MV patients, whose mouths are open and who are not usually allowed to drink or take ice chips, are often thirsty [8] and might benefit from our intervention. Future research is required with MV patients who are cognitively clear enough to self-report to demonstrate benefit to them and extend generalizability of results.
Some patients received small amounts of fluids during the procedure. However, since more usual care patients received fluids, the intervention effect might actually be underestimated. Thus, thirst relief measures can be given to patients regardless of their oral fluid status. Additionally, the effectiveness of the individual parts of the thirst bundle was not analyzed, so we do not know if thirst reduction requires all parts of the bundle. Finally, since there were at least 30 min between each session, we do not know the precise duration of effectiveness of the thirst bundle. In actual practice, versus research conditions, the thirst bundle could be used more frequently, as needed. The necessary materials (i.e., ice-cold water in spray bottles, swabs, and moisturizer) could be at the patient’s bedside. Either the patient’s nurse or a family member could use the materials to help with patient thirst relief [38].
Conclusions
Thirst is a prevalent, intense, and distressing symptom in ICU patients. A bundle of simple, inexpensive, and safe measures reduced TI and TD as well as xerostomia. Integrating this practice with routine thirst assessment can relieve one of the most distressing symptoms experienced by critically ill patients.
References
McKinley MJ, Cairns MJ, Denton DA, Egan G, Mathai ML, Uschakov A, Wade JD, Weisinger RS, Oldfield BJ (2004) Physiological and pathophysiological influences on thirst. Physiol Behav 81:795–803
Greenleaf JE (1992) Problem: thirst, drinking behavior, and involuntary dehydration. Med Sci Sports Exerc 24:645–656
Sreenbny LM (1996) Xerostomia: diagnosis, management and clinical complications. In: Edgar WM, O’Mullane DM (eds) Saliva and oral health. British Dental Association, London, pp 43–66
So HM, Chan DS (2004) Perception of stressors by patients and nurses of critical care units in Hong Kong. Int J Nurs Stud 41:77–84
Lombardo V, Vinatier I, Baillot ML, Franja V, Bourgeon-Ghittori I, Dray S, Jeune S, Mossadegh C, Reignier J, Souweine B, Roch A (2013) How caregivers view patient comfort and what they do to improve it: a French survey. Ann Intensive Care 3:1–8
Rose L, Nonoyama M, Rezaie S, Fraser I (2013) Psychological wellbeing, health related quality of life and memories of intensive care and a specialised weaning centre reported by survivors of prolonged mechanical ventilation. Intensive Crit Care Nurs. doi:10.1016/j.iccn.2013.11.002
Persenius MW, Hall-Lord ML, Wilde-Larsson B (2009) Grasping the nutritional situation: a grounded theory study of patients’ experiences in intensive care. Nurs Crit Care 14:166–174
Nelson JE, Meier DE, Oei EJ, Nierman DM, Senzel RS, Manfredi PL, Davis SM, Morrison RS (2001) Self-reported symptom experience of critically ill cancer patients receiving intensive care. Crit Care Med 29:277–282
Nelson JE, Meier DE, Litke A, Natale DA, Siegel RE, Morrison RS (2004) The symptom burden of chronic critical illness. Crit Care Med 32:1527–1534
Puntillo KA, Arai S, Cohen NH, Gropper MA, Neuhaus J, Paul SM, Miaskowski C (2010) Symptoms experienced by intensive care unit patients at high risk of dying. Crit Care Med 38:2155–2160
Nelson JE, Puntillo KA, Pronovost PJ, Walker AS, McAdam JL, Ilaoa D, Penrod J (2010) In their own words: patients and families define high-quality palliative care in the intensive care unit. Crit Care Med 38:808–818
Prendergast V, Jakobsson U, Renvert S, Hallberg IR (2012) Effects of a standard versus comprehensive oral care protocol among intubated neuroscience ICU patients: results of a randomized controlled trial. J Neurosci Nurs 44(3):134–146
Feider LL, Mitchell P, Bridges E (2010) Oral care practices for orally intubated critically ill adults. Am J Crit Care 9:175–183
Pear S (2007) The role of oral care in the prevention of hospital-acquired pneumonia. Infection Control Today 11(10):1–3
Wiley SB (1969) Why glycerol and lemon juice? Am J Nurs 69:342–344
Van Drimmelen J, Rollins HF (1969) Evaluation of a commonly used oral hygiene agent. Nurs Res 8:327–332
Meurman JH, Sorvari R, Pelttari A, Rytomaa I, Franssila S, Kroon L (1996) Hospital mouth-cleaning aids may cause dental erosion. Spec Care Dentist 16:247–250
Miller M, Kearney N (2001) Oral care for patients with cancer: a review of the literature. Cancer Nurs 24:241–254
Furness S, Worthington HV, Bryan G, Birchenough S, McMillan R (2011) Interventions for the management of dry mouth: topical therapies. Cochrane Database Syst Rev 12:CD008934
Porth CM, Erickson M (1992) Physiology of thirst and drinking: implication for nursing practice. Heart Lung 21:273–282
Eccles R (2000) Role of cold receptors and menthol in thirst, the drive to breathe and arousal. Appetite 34:29–35
Tomioko T, Inomata K, Nakaoka M, Futakami J, Yamada Y, Watanabe M, Takao S, Yokoyama Y (2006) Support for heart failure patients with thirst induced by fluid restriction: usefulness of a spray with sufficient sialogogic effect. J Kushiro City Gen Hosp 18:29–32
Phillips PA, Bretherton M, Risvanis J, Casley D, Johnston C, Gray L (1993) Effects of drinking on thirst and vasopressin in dehydrated elderly men. Am J Physiol 264:R877–R881
Brunstrom JM (2002) Effects of mouth dryness on drinking behavior and beverage acceptability. Physiol Behav 76:423–429
Brunstrom JM, Macrae AW (1997) Effects of temperature and volume on measures of mouth dryness, thirst and stomach fullness in males and females. Appetite 29:31–42
Berry AM, Davidson PM (2006) Beyond comfort: oral hygiene as a critical nursing activity in the intensive care unit. Intensive Crit Care Nurs 22:318–328
Schafer K, Braun HA, Isenberg C (1986) Effect of menthol on cold receptor activity. Analysis of receptor processes. J Gen Physiol 88:757–776
Deaux E (1973) Thirst satiation and the temperature of ingested water. Science 181:1166–1167
Szlyk PC, Sils IV, Francesconi RP, Hubbard RW, Armstrong LE (1989) Effects of water temperature and flavoring on voluntary dehydration in men. Physiol Behav 45:639–647
Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P (2008) Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med 148:295–309
Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA, Tesoro EP, Elswick RK (2002) The Richmond Agitation-Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med 166:1338–1344
Jensen MP, Karoly P, Braver S (1986) The measurement of clinical pain intensity: a comparison of six methods. Pain 27:117–126
Damiano AM, Bergner M, Draper EA, Knaus WA, Wagner DP (1992) Reliability of a measure of severity of illness: acute physiology of chronic health evaluation–II. J Clin Epidemiol 45:93–101
Hox J (2002) Multilevel analysis: techniques and applications. Lawrence Erlbaum Associates, Mahwah
Singer JD, Willett JB (2003) Applied longitudinal data analysis: modeling change and event occurrence. Oxford University Press, New York
Todd KH (1996) Clinical versus statistical significance in the assessment of pain relief. Ann Emer Med 27:439–441
Serlin RC, Mendoza TR, Nakamura Y, Edwards KR, Cleeland CS (1995) When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain 61:277–284
Hammond F (1995) Involving families in care within the intensive care environment: a descriptive survey. Intensive Crit Care Nurs 11:256–264
Acknowledgments
This study was supported by a grant from the National Institutes of Health National Institute for Nursing Research 1NR011825-03. Principal Investigator: Dr. K. Puntillo. Dr. Nelson is the recipient of a K07 Academic Career Leadership Award (AG034234) from the National Institute on Aging. The authors wish to acknowledge the nurses in the ICUs in which this study was performed and all of the patients who participated in our study.
Conflicts of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: Thirst is one of the most pervasive, intense, and undertreated symptoms in ICU patients. A thirst bundle consisting of oral swab wipes, sterile ice-cold water sprays, and a lip moisturizer significantly decreased ICU patients’ thirst and dry mouth and can be considered as a practice intervention for patients experiencing thirst. Thirst in ICU patients is relieved by a thirst bundle containing oral swab wipes, sterile ice-cold water sprays, and lip moisturizer.
Clinical trial registered with www.ClinicalTrials.gov (NCT01015755).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Puntillo, K., Arai, S.R., Cooper, B.A. et al. A randomized clinical trial of an intervention to relieve thirst and dry mouth in intensive care unit patients. Intensive Care Med 40, 1295–1302 (2014). https://doi.org/10.1007/s00134-014-3339-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3339-z