Abstract
Purpose
We assessed long-term mortality and hospitalisation in patients with severe sepsis resuscitated with hydroxyethyl starch (HES) or Ringer’s acetate.
Methods
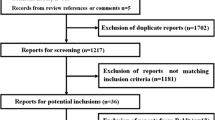
This was an investigator-initiated, parallel-grouped, blinded randomised trial using computer-generated allocation sequence and centralised allocation data that included 804 patients with severe sepsis needing fluid resuscitation in 26 general intensive care units (ICUs) in Scandinavia. Patients were allocated to fluid resuscitation using either 6 % HES 130/0.42 or Ringer’s acetate during ICU admission. We assessed mortality rates at 6 months, 1 year and at the time of longest follow-up and days alive and out of hospital at 1 year.
Results
The vital status of all patients was obtained at a median of 22 (range 13–36) months after randomisation. Mortality rates in the HES versus Ringer’s groups at 6 months were 53.3 (212/398 patients) versus 47.5 % (190/400) [relative risk 1.12; 95 % confidence interval (CI) 0.98–1.29; P = 0.10], respectively; at 1 year, 56.0 (223/398) versus 51.5 % (206/400) (1.09; 95 % CI 0.96–1.24; P = 0.20), respectively; at the time of longest follow-up, 59.8 (238/398) versus 56.3 % (225/400) (1.06; 95 % CI 0.94–1.20; P = 0.31), respectively. Percentage of days alive and out of hospital at 1 year in the HES versus Ringer’s groups was 24 (0–87 days) versus 63 % (0–90) (P = 0.07).
Conclusions
The long-term mortality rates did not differ in patients with severe sepsis assigned to HES 130/0.42 versus Ringer’s acetate, but we could not reject a 24 % relative increased or a 4 % relative decreased mortality at 1 year with HES at the 95 % confidence level.

Similar content being viewed by others
References
Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N, Moerer O, Gruendling M, Oppert M, Grond S, Olthoff D, Jaschinski U, John S, Rossaint R, Welte T, Schaefer M, Kern P, Kuhnt E, Kiehntopf M, Hartog C, Natanson C, Loeffler M, Reinhart K (2008) Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 358:125–139
Guidet B, Martinet O, Boulain T, Philippart F, Poussel JF, Maizel J, Forceville X, Feissel M, Hasselmann M, Heininger A, van Aken H (2012) Assessment of hemodynamic efficacy and safety of 6 % hydroxyethylstarch 130/0.4 vs. 0.9 % NaCl fluid replacement in patients with severe sepsis: the CRYSTMAS study. Crit Care 16:R94
Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Aneman A, Madsen KR, Moller MH, Elkjaer JM, Poulsen LM, Bendtsen A, Winding R, Steensen M, Berezowicz P, Soe-Jensen P, Bestle M, Strand K, Wiis J, White JO, Thornberg KJ, Quist L, Nielsen J, Andersen LH, Holst LB, Thormar K, Kjaeldgaard AL, Fabritius ML, Mondrup F, Pott FC, Moller TP, Winkel P, Wetterslev J (2012) Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med 367:124–134
Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, Glass P, Lipman J, Liu B, McArthur C, McGuinness S, Rajbhandari D, Taylor CB, Webb SA (2012) Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med 367:1901–1911
Haase N, Perner A, Hennings LI, Siegemund M, Lauridsen B, Wetterslev M, Wetterslev J (2013) Hydroxyethyl starch 130/0.38-0.45 versus crystalloid or albumin in patients with sepsis: systematic review with meta-analysis and trial sequential analysis. BMJ 346:f839
Patel A, Waheed U, Brett SJ (2013) Randomised trials of 6 % tetrastarch (hydroxyethyl starch 130/0.4 or 0.42) for severe sepsis reporting mortality: systematic review and meta-analysis. Intensive Care Med 39:811–822
Müller RG, Haase N, Wetterslev J, Perner A (2013) Effects of hydroxyethyl starch in subgroups of patients with severe sepsis: exploratory post hoc analyses of a randomised trial. Intensive Care Med 39:1963–1971
Mutter TC, Ruth CA, Dart AB (2013) Hydroxyethyl starch (HES) versus other fluid therapies: effects on kidney function. Cochrane Database Syst Rev 7: CD007594
Citerio G, Bakker J, Bassetti M, Benoit D, Cecconi M, Curtis JR, Hernandez G, Herridge M, Jaber S, Joannidis M, Papazian L, Peters M, Singer P, Smith M, Soares M, Torres A, Vieillard-Baron A, Timsit JF, Azoulay E (2014) Year in review in Intensive Care Medicine 2013: I. acute kidney injury, ultrasound, hemodynamics, cardiac arrest, transfusion, neurocritical care, and nutrition. Intensive Care Med 40:147–159
Gattas DJ, Dan A, Myburgh J, Billot L, Lo S, Finfer S (2013) Fluid resuscitation with 6 % hydroxyethyl starch (130/0.4 and 130/0.42) in acutely ill patients: systematic review of effects on mortality and treatment with renal replacement therapy. Intensive Care Med 39:558–568
Zarychanski R, Bou-Setta AM, Turgeon AF, Houston BL, McIntyre L, Marshall JC, Fergusson DA (2013) Association of hydroxyethyl starch administration with mortality and acute kidney injury in critically ill patients requiring volume resuscitation: a systematic review and meta-analysis. JAMA 309:678–688
Wiedermann CJ, Joannidis M (2014) Accumulation of hydroxyethyl starch in human and animal tissues: a systematic review. Intensive Care Med 40:160–170
Hartog CS, Reuter D, Loesche W, Hofmann M, Reinhart K (2011) Influence of hydroxyethyl starch (HES) 130/0.4 on hemostasis as measured by viscoelastic device analysis: a systematic review. Intensive Care Med 37:1725–1737
Haase N, Wetterslev J, Winkel P, Perner A (2013) Bleeding and risk of death with hydroxyethyl starch in severe sepsis: post hoc analyses of a randomized clinical trial. Intensive Care Med 39:2126–2134
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39:165–228
Meybohm P, van Aken H, Gasperi AD, Hert SD, Rocca GD, Girbes AR, Gombotz H, Guidet B, Hasibeder W, Hollmann MW, Ince C, Jacob M, Kranke P, Kozek-Langenecker S, Loer SA, Martin C, Siegemund M, Wunder C, Zacharowski K (2013) Re-evaluating currently available data and suggestions for planning randomised controlled studies regarding the use of hydroxyethyl starch in critically ill patients—a multidisciplinary statement. Crit Care 17:R166
Annane D, Siami S, Jaber S, Martin C, Elatrous S, Declere AD, Preiser JC, Outin H, Troche G, Charpentier C, Trouillet JL, Kimmoun A, Forceville X, Darmon M, Lesur O, Regnier J, Abroug F, Berger P, Clec’h C, Cousson J, Thibault L, Chevret S (2013) Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock: the CRISTAL randomized trial. JAMA 310:1809–1817
Perner A, Haase N, Wetterslev J, Aneman A, Tenhunen J, Guttormsen AB, Klemenzson G, Pott F, Bodker KD, Badstolokken PM, Bendtsen A, Soe-Jensen P, Tousi H, Bestle M, Pawlowicz M, Winding R, Bulow HH, Kancir C, Steensen M, Nielsen J, Fogh B, Madsen KR, Larsen NH, Carlsson M, Wiis J, Petersen JA, Iversen S, Schoidt O, Leivdal S, Berezowicz P, Pettila V, Ruokonen E, Klepstad P, Karlsson S, Kaukonen M, Rutanen J, Karason S, Kjaeldgaard AL, Holst LB, Wernerman J (2011) Comparing the effect of hydroxyethyl starch 130/0.4 with balanced crystalloid solution on mortality and kidney failure in patients with severe sepsis (6S—Scandinavian Starch for Severe Sepsis/Septic Shock trial): study protocol, design and rationale for a double-blinded, randomised clinical trial. Trials 12:24
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le G Jr, Payen D (2006) Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 34:344–353
Reinikainen M, Karlsson S, Varpula T, Parviainen I, Ruokonen E, Varpula M, Ala-Kokko T, Pettila V (2010) Are small hospitals with small intensive care units able to treat patients with severe sepsis? Intensive Care Med 36:673–679
(1992) American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20: 864–74
ICH Steering Committee (1998) International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. ICH harmonised tripartite guideline for good clinical practice, 3rd edn. Brookwood Medical Publications Ltd, Richmond
Fergusson D, Aaron SD, Guyatt G, Hebert P (2002) Post-randomisation exclusions: the intention to treat principle and excluding patients from analysis. BMJ 325:652–654
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
Angus DC, Laterre PF, Helterbrand J, Ely EW, Ball DE, Garg R, Weissfeld LA, Bernard GR (2004) The effect of drotrecogin alfa (activated) on long-term survival after severe sepsis. Crit Care Med 32:2199–2206
Clermont G, Angus DC, Linde-Zwirble WT, Griffin MF, Fine MJ, Pinsky MR (2002) Does acute organ dysfunction predict patient-centered outcomes? Chest 121:1963–1971
Bion J, Bellomo R, Myburgh J, Perner A, Reinhart K, Finfer S (2014) Hydroxyethyl starch: putting patient safety first. Intensive Care Med 40:256–259
Perner A, Haase N, Wetterslev J (2014) Mortality in patients with hypovolemic shock treated with colloids or crystalloids. JAMA 311:1067
Wittbrodt P, Haase N, Butowska D, Winding R, Poulsen JB, Perner A (2013) Quality of life and pruritus in patients with severe sepsis resuscitated with hydroxyethyl starch long-term follow-up of a randomised trial. Crit Care 17:R58
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions Version 5.1.0. The Cochrane Collaboration. Available at: http://www.cochrane.org/handbook. Accessed 25 April 2014
Conflicts of interest
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: The 6S trial was funded by the Danish Medical Research Council (271-08-0691 and 09-066938) and supported by Rigshospitalets Research Council and the Scandinavian Society of Anaesthesiology and Intensive Care Medicine (the ACTA foundation) and endorsed by the European Clinical Research Infrastructures Network (ECRIN). B Braun AG delivered trial fluids to all trial sites free of charges. Neither the funding organisations nor B Braun had any influence on (1) the design and conduct of the study; (2) the collection, management, analysis and interpretation of the data; (3) the preparation, review or approval of the manuscript; (4) the decision to submit the manuscript for publication. AP is head of research in his ICU, which receives research funds from CSL Behring, Switzerland, Fresenius Kabi, Germany, COSMED, Italy and Bioporto Diagnostics A/S, Denmark and has received a speaker’s fee from LFP SA, France. B Braun AG has covered his travel expenses for presenting 6S-data at the German Anaesthetic Congress 2012.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message:
The long-term mortality rates did not differ in patients with severe sepsis assigned to HES 130/0.42 versus Ringer’s acetate, but the trial was not powered to show this. As 90-day mortality differed, the data indicate that the harmful effects of HES occurred within the first months after randomisation.
On behalf of the 6S trial group, and the Scandinavian Critical Care Trials Group.
Members of the Scandinavian Starch for Severe Sepsis/Septic Shock (6S) trial group are listed in the Appendix.
Trial registration: clinicaltrials.gov NCT00962156.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
The 6S trial investigators
Steering Committee: Anders Perner (Chair), Nicolai Haase, Anne B. Guttormsen, Jyrki Tenhunen, Gudmundur Klemenzson, Anders Åneman and Jørn Wetterslev.
Management Committee: Anders Perner (Chair), Nicolai Haase and Jørn Wetterslev.
Scientific Committee: Simon Finfer, Andre Vercueil, Lars S. Rasmussen and Frank Brunkhorst.
Data Monitoring and Safety Committee: Daniel De Backer (Chair), Peter Dalgaard and Kathy Rowan.
Writing Committee: Anders Perner (Chair), Nicolai Haase and Jørn Wetterslev.
Trial site investigators (in Denmark unless otherwise specified): Rigshospitalet: A. Perner, N. Haase, M.N. Kjær, K.R. Uhre, V. Knudsen, V. Christiansen, A. Schulze, J. Wiis, J.O. White, K. Thornberg, L.Quist, F. Sjøvall, N. Wesche, N. Reiter, I.L. Jarnvig; Næstved Hospital: K.R. Madsen, A. L. Kjældgaard, M. L. Fabritius, F. Mondrup, K.F. Sommer, L. F. Pedersen; Bispebjerg Hospital: M.H. Møller, F.C. Pott, J.A. Petersen, A. Lindhardt, K. Møller, A. Haraldson, C. Pedersen; Holbæk Hospital: H.H. Bülow, J.M. Elkjær, T. P. Møller, L.H. Andersen, L.B. Holst, J.F. Schmidt, S.T. Nielsen, F.P. Treschow, M. Overgaard, H. Ahlstrøm, S. Grangaard, J.H. Bruun, S. Larsen; Køge Hospital: L.M. Poulsen, M.V. Madsen, B. Bang; Glostrup Hospital: A. Bendtsen, Herning Hospital R. Winding, K.V. Jepsen, S. Haubjerg, N. Dey, J. Hjørringsgaard; Hvidovre Hospital: M. Steensen, J. Nielsen, C. Albek, S. Petersen, A. Christensen, A. Kristensen; Vejle Hospital: P.Berezowicz; Herlev Hospital: P. Søe-Jensen, H. Tousi; Hillerød Hospital: M. Bestle, K. Nielsen, T. Kold, K. Grundahl; Stavanger University Hospital, Norway: K. Strand, O. Larsen; Slagelse Hospital: S. Iversen, O. Schøidt; Hjørring Hospital: M. Pawlowicz, M. Kruse, H.S. Rasmussen, L.O. Nielsen; Haukeland University Hospital, Bergen, Norway: A.B. Guttormsen, B. Sjøbø; Sønderborg Hospital: S. Leivdal; Tromsø University Hospital, Norway: L.M. Ytrebø; Tampere University Hospital, Finland: J. Tenhunen, S. Karlsson, A. Kukkurainen, S. Kortelainen, M.L. Peltola, S. Varila; Gentofte Hospital: K. Thormar, P.M. Bådstøløkken; Landspitali, Reykjavik, Iceland: G. Klemenzson, S. Karason; Helsinki University Hospital, Finland: V. Pettilä, M. Kaukonen, L. Pettilä, S. Sutinen; Odense University Hospital: M. Carlson, N.H. Lassen, U.L. Larsen, K.D. Jung; Holstebro Hospital: C. Kancir; Kuopio University Hospital, Finland: J. Rutanen, E. Ruokonen, S. Rissanen, K. Kontra; Trondheim University Hospital, Norway: P. Klepstad; Esbjerg Hospital: R.E. Berthelsen, K.D. Bødker, B. Dilling.
Rights and permissions
About this article
Cite this article
Perner, A., Haase, N., Winkel, P. et al. Long-term outcomes in patients with severe sepsis randomised to resuscitation with hydroxyethyl starch 130/0.42 or Ringer’s acetate. Intensive Care Med 40, 927–934 (2014). https://doi.org/10.1007/s00134-014-3311-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3311-y