Abstract
Background
Recently, a new technology has been introduced aiming to monitor and improve patient ventilator interaction (PVI monitor). With the PVI monitor, a signal representing an estimation of the patient’s total inspiratory muscle pressure (PmusPVI) is calculated from the equation of motion, utilizing estimated values of resistance and elastance of the respiratory system.
Objective
The aim of the study was to prospectively examine the accuracy of PmusPVI to quantify inspiratory muscle pressure.
Methods and interventions
Eleven critically ill patients mechanically ventilated on proportional assist ventilation with load-adjustable gain factors were studied at three levels of assist (30, 50 and 70%). Airway, esophageal, gastric and transdiaphragmatic (Pdi) pressures, volume and flow were measured breath by breath, whereas the total inspiratory muscle pressure (Pmus) was calculated using the Campbell diagram.
Results
For a given assist, PmusPVI throughout inspiration did not differ from the corresponding values calculated using the Pdi and Pmus signals. Inspiratory and expiratory time did not differ among the various methods of calculation. Inspiratory muscle pressure decreased with increasing assist, and the magnitude of this decrease did not differ among the various methods of pressure calculation.
Conclusions
A signal generated from flow, volume and airway pressure may be used to provide breath-by-breath quantitative information of inspiratory muscle pressure.
Similar content being viewed by others
Introduction
One of the main goals of mechanical ventilation is to unload the respiratory muscles [1]. Complete unloading of respiratory muscles may be achieved during controlled mechanical ventilation [2], which usually necessitates heavy sedation and occasionally administration of neuromuscular blocking agents. However, recent evidence in the literature indicates that active respiratory efforts during mechanical ventilation are beneficial, because they prevent respiratory muscle atrophy [3–6] and improve cardiovascular system function [7]. Moreover, switching mechanically ventilated patients to assisted modes of support reduces the complications associated with heavy sedation [8, 9] and thus is a priority in the intensive care unit [10, 11]. Nevertheless, during assisted mechanical ventilation, the patient interacts with the function of the ventilator, sometimes vigorously, and this interaction may influence the decision-making process and patient outcome [12, 13]. Patient-ventilator asynchrony largely prevents mechanical ventilation from achieving its goals and may impose significant harm to the patient [14]. It follows that assessment of respiratory output during assisted mechanical ventilation is crucial for proper titration of ventilator settings.
During mechanical ventilation, respiratory output can be monitored by the neural activity (i.e., NAVA technology) [15] and pressure output of respiratory muscles [16–18]. Notwithstanding that several factors may affect the transformation of neural activity to pressure output [19–22], the latter together with the ventilator pressure are the actual forces applied to respiratory system in order to execute the act of breathing. Thus, the respiratory muscle pressure may provide the caregiver important information regarding patient-ventilator interaction. This pressure output may be estimated either by transdiaphragmatic pressure or by calculating the instantaneous pressure output of the respiratory muscles [16, 17]. These approaches, however, necessitate the placement of esophageal and gastric catheters to record esophageal and gastric pressures, respectively. Other attempts to monitor respiratory muscle pressure are limited by the difficulties to estimate respiratory system mechanics or the dependency on the mode of support [18, 23, 24].
Recently, a new technology has been introduced aiming to monitor and improve patient ventilator interaction (PVI monitor, YRT, Winnipeg, Canada) [25]. With the PVI monitor, a signal representing an estimate of the patient’s total inspiratory muscle pressure (PmusPVI) is calculated via the equation of motion, using estimated values of resistance and elastance of the respiratory system, obtained without additional interventions in mechanically ventilated patients [25]. The waveform of PmusPVI is continuously displayed on-line on a breath-by-breath basis. The effectiveness of the PVI monitor in terms of identifying triggering delay, ineffective efforts and expiratory asynchrony has been retrospectively evaluated and recently reported by a study using pre-existing recording of flow, volume and airway pressure [25]. Since then, PVI software has been upgraded for the purpose of quantifying inspiratory muscle pressure. Thus, the aim of this study is to prospectively examine if inspiratory muscle pressure can be quantified during assisted mechanical ventilation using the method of PVI technology.
Methods (see also electronic supplementary material)
Patients
Thirteen patients admitted to the Intensive Care Unit for management of acute respiratory failure were studied. At the time of the study all patients were lightly sedated with propofol (Ramsay scale score 3), hemodynamically stable and ventilated on proportional assist ventilation (PAV) with the load-adjustable gain factors model with the ability to measure respiratory system mechanics (PAV+) semi-continuously (Nellcor Puritan Bennett LLC, Gosport, UK,). The study was approved by the hospital ethics committee, and informed consent was obtained from the patients or their families.
Measurements
Flow (V′), volume (V) and airway (Paw), esophageal (Pes) and gastric (Pga) pressures were measured as described previously [26, 27]. The proper position of the balloons was verified using standard tests [27, 28]. Transdiaphragmatic (Pdi) and transpulmonary (Ptp) pressures were derived by subtraction of Pes from Pga and Pes from Paw, respectively. Each signal was sampled at 200 Hz (WinDaq Instruments, Akron, OH) and stored on a computer disk for later analysis.
Study protocol
The patients were studied in semi-recumbent position (>45°) in order to obtain a Pes signal as accurately as possible. The patients were studied randomly at three levels of assist, 30, 50 and 70%. At each level the patients remained for 30 min.
Calculations and data analysis
Respiratory system and chest wall mechanics
Passive mechanical ventilation
At the end of the study, the patients were placed on volume-control, constant flow mode and ventilated passively with V T of 10 ml/kg. End-inspiratory respiratory system elastance (Ersp), maximum and minimum inspiratory system resistances (R max and R min), as well as chest wall elastance (Ecwp) and resistance (Rcw) were measured by the technique of rapid airway occlusion using standard formulas [28].
Assisted mechanical ventilation
Mechanics during assisted ventilation were calculated at each level of assist using the unique feature of proportional assist ventilation, which is the tight link between neural inspiration and ventilator pressure [23, 24]. Initially at each level of assist the ventilator software calculated end-inspiratory respiratory system elastance (Ersa), corrected for the presence of intrinsic PEEP [29]. Dynamic lung elastance (E L) was calculated by dividing the difference in Ptp at zero flow in the beginning and end of inflation by the corresponding V T [30]. E L was subtracted from Ersa to obtain chest wall elastance during active breathing (Ecwa). Assuming that Rcw did not differ during active and passive respiration, chest wall resistance was not calculated during active conditions.
Resistance of respiratory system during active respiration was calculated by (1) the ventilator software of PAV+ (RrsPAV+) and (2) the iso-volume technique (Rrsiso) [30]. With the latter method lung resistance (R L) was estimated, whereas Rrsiso was obtained by adding Rcw to R L [30].
Determination of inspiratory muscle pressure (PmusPVI)
PmusPVI was calculated on a breath-by-breath basis by a research prototype (PVI Monitor, YRT Limited, Winnipeg, Canada) using a method described in detail previously [25]. Briefly, the inputs required by the monitor to calculate PmusPVI were Paw and V′, whereas V was obtained by V′ integration. At least two points during expiration that satisfied passive conditions (i.e., flow was driven by the elastic recoil pressure) were automatically identified by the monitor. At these points, the equation of motion was applied, and elastance (ErsPVI) and resistance (RrsPVI) of the respiratory system were calculated. Using these values and the equation of motion, PmusPVI was calculated during each breath. Further fine-tuning of ErsPVI and RrsPVI was performed to eliminate artifacts derived from PmusPVI waveform. The monitor may calculate PmusPVI during ineffective efforts (i.e., absence of ventilator triggering) using the estimated values of ErsPVI and RrsPVI from the previous breaths and the change in V′, V and Paw caused by the ineffective effort. The proper function of the monitor requires a peak inspiratory Paw at least 3 cmH2O above PEEP. At lower Paw the calculation of respiratory system mechanics may not be reliable. However, under this circumstance the monitor continues to display the Pmus waveform, but its amplitude may not be accurate.
Pressure calculation generated by all respiratory muscles (Pmus)
Pmus was calculated from Pes taking into account the elastic and resistive properties of the chest wall. This calculation, which is based on the Campbell diagram (analysis of esophageal pressure–volume loops), has been previously described [17]. Pmus was calculated using both the values of Ecwa (Pmusa) and Ecwp (Pmusp).
Data analysis
The last 2 min of each 30-min period was analyzed and averaged to give the breath variables corresponding to each experimental condition. Patient mechanical inspiratory time was measured using the Pdi, Pmusa, Pmusp and PmusPVI signals as the interval between the beginning of the signal increase and the point at which these signals started to decline rapidly (TIPdi, TIPmusa, TIPmusp and TIPmusPVI, respectively). Patient mechanical expiratory time was measured as the remainder of the respiratory cycle, determined from the corresponding waveforms (TEPdi, TEPmusa, TEPmusp and TEPmusPVI, respectively). The rate of rise of these signals (dp/dt) was calculated as the difference between the signal peak and the value at the onset of signal increase divided by the corresponding time. Pressure time product (PTP) of these signals was also calculated as the area under the curve during the corresponding inspiratory time (PTPPdi, PTPPmusa, PTPPmusp and PTPPmusPVI). The level of PEEPi during the different experimental conditions was measured as the positive deflection of Pdi from the onset of neural inspiration to the point of zero flow [29].
Statistical analysis
Data were analyzed by multi-factor analysis of variance for repeated measurements (ANOVA), followed by Tukey’s test for multiple comparison if the F value was significant. A p less than 0.05 was considered statistically significant. All values are expressed as mean ± SD.
Results (see also ESM)
Patients’ characteristics are shown in Table 1. Two patients were excluded from the analysis (no. 12 and 13) for technical reasons (see ESM). In one patient (no. 3) Pes and Pga data were accidentally lost after Pdi calculation and thus only comparison between Pdi and PmusPVI was made for this patient. Excluding this patient, the results did not change (see below). In one patient (no. 4) the PVI monitor did not estimate PmusPVI at 30% of assist due to low peak Paw (<3 cmH2O above PEEP) at this level of support.
Peak Paw increased significantly with increasing the level of assist, averaging 12.1 ± 2.1, 16.1 ± 3.6 and 19.8 ± 5.1 cmH2O at 30, 50 and 70% of assist, respectively. V T and breathing frequency (Fr) did not differ as a function of assist (V T 0.40 ± 0.1, 0.43 ± 0.12, 0.43 ± 0.1 l; Fr 24.0 ± 6.3, 22.6 ± 6.8, 20.7 ± 5.5 br/min, at 30, 50 and 70%, respectively). Ineffective efforts were not identified during the study period.
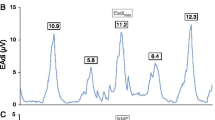
Representative waveforms of Paw, flow, volume, Pdi and PmusPVI are shown in Fig. 1. Independent of the method, all indices of inspiratory effort increased significantly with decreasing assist. For a given assist, peak PmusPVI, dPmusPVI/dt and PTPPmusPVI per breath did not differ from the corresponding values calculated using the Pdi, Pmusp and Pmusa signals (Table 2 and Figure S1). Although indices of inspiratory effort calculated from Pdi were lower than those from the other three signals, the difference was not significant. Inspiratory and expiratory time did not differ among the various methods of calculation (Table 2). The onset of inspiratory effort identified by PVI monitor was delayed from that in Pdi signal by 0.06 ± 0.05, 0.05 ± 0.04 and 0.05 ± 0.03 s at 30, 50 and 70% assist, respectively.
Airway pressure (Paw 2 cmH2O/division), flow (V′ 0.2 l/s/division), volume (V 0.1 l/division), transdiaphragmatic pressure (Pdi 5 cmH2O/divison) and inspiratory pressure calculated by the PVI monitor (PmusPVI 5 cmH2O/divison) in a representative patient ventilated with 30% of assist. Arrow indicates the breath in which occlusion at the end of inspiration was performed by the PAV+ software to calculate respiratory system mechanics. The dashed vertical lines indicate the beginning of patient’s inspiration as defined by the Pdi waveform (rapid increase in Pdi from the value at the end of expiration). The continuous vertical line of the third breath indicates the point of zero flow. Notice that in all breaths PmusPVI waveform tracks closely that of Pdi in terms of timing (see the dashed lines), amplitude (see the breath variability) and shape, even in the presence of dynamic hyperinflation [see the third breath in which intrinsic PEEP (measured as the change in Pdi to reverse flow from expiratory to inspiratory) was 3.12 cmH2O]
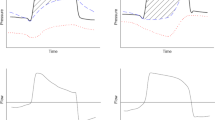
Figure 2 shows mean Pdi, PmusPVI, Pmusp and Pmusa at 20, 40, 60, 80 and 100% of the corresponding inspiratory time, respectively. At any given % of inspiratory time PmusPVI, Pmusp and Pmusa were similar. At any given % of inspiratory time Pdi was slightly but non-significantly lower than PmusPVI, Pmusp and Pmusa. In all patients PmusPVI, as a function of % of inspiratory time, was linearly related to Pdi, Pmusp and Pmusa. The slope of the Pdi-PmusPVI relationship was significantly higher than that of Pmusp-PmusPVI and Pmusa-PmusPVI (Table 3).
Figure S3 shows the mean increase in Pdi, PmusPVI, Pmusa and Pmusp as the level of assist decreased from 70 to 30%. For a given % of inspiratory time, the increase did not differ among the various methods of respiratory motor output calculation.
Respiratory system mechanics calculated during active respiration by the PVI monitor as well as by the PAV+ mode did not differ as a function of assist, and thus they were averaged for the simplicity of comparison. Although Ersp (24.5 ± 8.2 cmH2O/l) was higher than ErsPAV+ (20.3 ± 5.1) and ErsPVI (22.3 ± 6.8), the difference was not significant. RrsPVI (9.9 ± 5.0 cmH2O/l/s), RrsPAV+ (8.5 ± 3.4) and Rrsiso (10.6 ± 5.6) were significantly higher than Rmin (4.8 ± 3.2). Rmax, RrsPVI, RrsPAV+ and Rrsiso did not differ significantly. Figures S7 and S8 show the relation and Bland-Altman analysis between ErsPVI and RrsPVI and the corresponding respiratory system mechanics obtained during active (ErsPAV+, RrsPAV+, Rrsiso) and passive (Ersp, Rmin, Rmax) conditions. There was a significant correlation in all cases, but there was considerable scatter. PVI mechanics were better correlated with those obtained during active breathing than those during passive mechanical ventilation.
Discussion
The main finding of this study is that a signal generated from flow, volume, and airway pressure can be used to provide breath-by-breath quantitative information of inspiratory muscle pressure in mechanically ventilated critically ill patients.
In our study inspiratory muscle pressure was assessed by (1) Pdi and (2) calculation of the pressure developed by all respiratory muscles (Pmus) using the Campbell diagram and chest wall mechanics during active (Pmusa) and passive respiration (Pmusp). We did not rely only on transdiaphragmatic pressure to estimate inspiratory muscle pressure because critically ill patients usually use other inspiratory muscles in addition to the diaphragm because of diaphragmatic dysfunction and increased workload [31, 32]. For this reason, Pmus waveform is a better reflection of respiratory muscle activity than transdiaphragmatic pressure. Indeed, Pdi-derived indices of inspiratory effort tended to be slightly lower, although not significantly, than those derived using Pmusa and Pmusp, indicating that in these patients the diaphragm was not the only inspiratory muscle that determined total inspiratory muscle pressure.
We chose to study patients ventilated with PAV+ mode because with this modality it was possible to calculate chest wall elastance during active breathing and thus to eliminate the errors, if any, in calculation of Pmus using Pes waveform during active breathing and chest wall mechanics measured during passive mechanical ventilation (control mode) at different times. It is well known that both the type of breathing (active vs. passive) and time may affect, sometimes substantially, respiratory system mechanics [23, 24]. Nevertheless, there is no reason to believe that our results may not be applied in patients ventilated with other modes of assisted mechanical ventilation. The inputs required by the monitor to generate inspiratory muscle pressure waveform are airway pressure, flow and volume independent of their shape. Indeed, it has been shown that the PVI monitor can generate a reliable, at least in terms of timing, Pmus signal during pressure support ventilation, even at the absence of ventilator triggering (ineffective triggering) because of dynamic hyperinflation [25]. This is because the monitor calculates PmusPVI based on a change of flow, volume and airway pressure caused by the application of inspiratory muscle pressure on the respiratory system. Thus, provided that peak airway pressure during inspiration is at least 3 cmH2O above PEEP, the monitor can calculate inspiratory muscle pressure on a breath-by-breath basis independent of the mode of support. Nevertheless, the quantification of inspiratory muscle pressure during other than PAV+ assisted modes remains to be studied.
At all levels of assist inspiratory muscle pressure estimated with PVI was similar to that obtained using the Campbell diagram. The slope of Pmusa-PmusPVI and Pmusp-PmusPVI approaches unity, and is significantly lower than that of Pdi–PmusPVI, indicating that indeed Pdi in these patients underestimates inspiratory muscle pressure. Furthermore, PmusPVI tracked with accuracy the load-induced changes in inspiratory muscle pressure; for a given % of inspiratory time, the increase in inspiratory muscle pressure when the assist decreased from 70 to 30% did not differ among the various methods of inspiratory muscle pressure calculation. It follows that, in critically ill patients, it is feasible to quantify the inspiratory muscle pressure without any intervention, using flow, volume and airway pressure, signals that may be easily obtained by the ventilator.
Our study showed that respiratory system mechanics estimated using PVI technology were similar to those estimated during active respiration using the ventilator software with PAV+ mode [23, 24] and the iso-volume technique of resistance measurement [30]. A good correlation was found for both elastance and resistance between PVI and PAV+ and iso-volume methods. Although good correlation was also observed between PVI-estimated and passive mechanics, resistance was higher and elastance lower when measured with PVI than when measured during passive mechanical ventilation. The difference between PVI and passive mechanics might not be entirely related to the methods of measurements for several reasons. Firstly, the measurements by the two methods were performed at least 1.5 h apart, and respiratory system mechanics may have changed in the interval [23, 24]. Secondly, mechanics during passive mechanical ventilation may differ from those during active breathing [23, 24]. Thirdly, the deepening of sedation and the use of muscle relaxants in some patients to achieve passive conditions may have affected the mechanical properties of the respiratory system [33]. Fourthly, PVI estimates expiratory elastance and an average of inspiratory and expiratory resistances, whereas elastance and resistance measured during passive ventilation are inspiratory. Inspiratory resistance in critically ill patients may be several fold lower than expiratory [26, 34].
Younes et al. [25] showed that the PVI signal is able to identify ineffective efforts as well as the onsets and ends of patient mechanical inspiratory efforts with reasonable accuracy. Our results confirmed these findings. We demonstrated that inspiratory time, identified by the PVI signal, did not differ from that obtained using standard methods (Pdi or Pmus waveforms). In agreement with Younes et al. [25] the onset of inspiratory effort in PVI signal was very close to that in Pdi, the time delay between the events in the two signals averaging approximately 50 ms. Furthermore, our study showed that PVI technology may be used to estimate the respiratory system mechanics and thus quantify the inspiratory muscle pressure. Indeed, inspiratory muscle pressure waveform estimated by the PVI monitor did not differ from that calculated using Pes and Pga.
A final point worth mentioning is that the PVI monitor may not be able to calculate a reliable Pmus signal in patients with very severe flow limitation in whom inspiratory efforts fail to distort airway pressure and/or flow [25]. Therefore, in these patients phenomena recorded at ventilator line (pressure and flow) are dissociated from that produced by respiratory efforts and located at alveoli. However, in our study we did not observe such a dissociation, probably because only three patients had obstructive lung disease, and at the time of the study, none of them exhibited severe flow limitation as indicated by the low levels of PEEPi (range 0.2–1.9 cmH2O).
The results of this study have important clinical implications. By identifying the onset and end of patient mechanical inspiratory time, the PVI signal may facilitate adjustments in ventilator settings to improve the triggering process and patient-ventilator synchrony [35, 36]. In addition, the current study showed that the PVI monitor can quantify inspiratory effort breath by breath and thus provide information about the degree of unloading of inspiratory muscles. Nevertheless, the optimal degree of unloading in mechanically ventilated patients is currently unknown, and thus setting the assist level based on various thresholds of inspiratory efforts [37, 38] may not be appropriate for an individual patient.
In conclusion, our study showed that in mechanically ventilated critically ill patients a signal generated from flow, volume and airway pressure may be used to provide breath-by-breath quantitative information of inspiratory muscle pressure.
References
Slutsky AS (1994) Consensus conference on mechanical ventilation—January 28–30, 1993 at Northbrook, Illinois, USA. Part I. European Society of Intensive Care Medicine, the ACCP and the SCCM. Intensive Care Med 20:64–79
Fitting JW (1994) Respiratory muscles during ventilatory support. Eur Respir J 7:2223–2225
Levine S, Nguyen T, Taylor N, Friscia ME, Budak MT, Rothenberg P, Zhu J, Sachdeva R, Sonnad S, Kaiser LR, Rubinstein NA, Powers SK, Shrager JB (2008) Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N Engl J Med 358:1327–1335
Shanely RA, Zergeroglu MA, Lennon SL, Sugiura T, Yimlamai T, Enns D, Belcastro A, Powers SK (2002) Mechanical ventilation-induced diaphragmatic atrophy is associated with oxidative injury and increased proteolytic activity. Am J Respir Crit Care Med 166:1369–1374
Sassoon CS, Zhu E, Caiozzo VJ (2004) Assist-control mechanical ventilation attenuates ventilator-induced diaphragmatic dysfunction. Am J Respir Crit Care Med 170:626–632
Futier E, Constantin JM, Combaret L, Mosoni L, Roszyk L, Sapin V, Attaix D, Jung B, Jaber S, Bazin JE (2008) Pressure support ventilation attenuates ventilator-induced protein modifications in the diaphragm. Crit Care 12:R116
Putensen C, Zech S, Wrigge H, Zinserling J, Stuber F, Von Spiegel T, Mutz N (2001) Long-term effects of spontaneous breathing during ventilatory support in patients with acute lung injury. Am J Respir Crit Care Med 164:43–49
Kress JP, Pohlman AS, O’Connor MF, Hall JB (2000) Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 342:1471–1477
Hooper MH, Girard TD (2009) Sedation and weaning from mechanical ventilation: linking spontaneous awakening trials and spontaneous breathing trials to improve patient outcomes. Crit Care Clin 25:515–525 viii
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut JF, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent JL (2008) Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 36:296–327
MacIntyre NR, Cook DJ, Ely EW Jr, Epstein SK, Fink JB, Heffner JE, Hess D, Hubmayer RD, Scheinhorn DJ (2001) Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest 120:375S–395S
Chao DC, Scheinhorn DJ, Stearn-Hassenpflug M (1997) Patient-ventilator trigger asynchrony in prolonged mechanical ventilation. Chest 112:1592–1599
Willatts SM, Drummond G (2000) Brainstem death and ventilator trigger settings. Anesthesia 55:676–677
Thille AW, Rodriguez P, Cabello B, Lellouche F, Brochard L (2006) Patient–ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med 32:1515–1522
Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, Gottfried SB, Lindstrom L (1999) Neural control of mechanical ventilation in respiratory failure. Nat Med 5:1433–1436
Laghi F (2005) Assessment of respiratory output in mechanically ventilated patients. Respir Care Clin N Am 11:173–199
Georgopoulos D, Mitrouska I, Webster K, Bshouty Z, Younes M (1997) Effects of inspiratory muscle unloading on the response of respiratory motor output to CO2. Am J Respir Crit Care Med 155:2000–2009
Yamada Y, Shigeta M, Suwa K, Hanaoka K (1994) Respiratory muscle pressure analysis in pressure-support ventilation. J Appl Physiol 77:2237–2243
Parthasarathy S, Jubran A, Tobin MJ (2000) Assessment of neural inspiratory time in ventilator-supported patients. Am J Respir Crit Care Med 162:546–552
Beck J, Sinderby C, Lindstrom L, Grassino A (1998) Effects of lung volume on diaphragm EMG signal strength during voluntary contractions. J Appl Physiol 85:1123–1134
Sinderby C, Beck J, Spahija J, de Marchie M, Lacroix J, Navalesi P, Slutsky AS (2007) Inspiratory muscle unloading by neurally adjusted ventilatory assist during maximal inspiratory efforts in healthy subjects. Chest 131:711–717
Sinderby C, Spahija J, Beck J, Kaminski D, Yan S, Comtois N, Sliwinski P (2001) Diaphragm activation during exercise in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 163:1637–1641
Younes M, Webster K, Kun J, Roberts D, Masiowski B (2001) A method for measuring passive elastance during proportional assist ventilation. Am J Respir Crit Care Med 164:50–60
Younes M, Kun J, Masiowski B, Webster K, Roberts D (2001) A method for noninvasive determination of inspiratory resistance during proportional assist ventilation. Am J Respir Crit Care Med 163:829–839
Younes M, Brochard L, Grasso S, Kun J, Mancebo J, Ranieri M, Richard JC, Younes H (2007) A method for monitoring and improving patient: ventilator interaction. Intensive Care Med 33:1337–1346
Kondili E, Alexopoulou C, Prinianakis G, Xirouchaki N, Georgopoulos D (2004) Pattern of lung emptying and expiratory resistance in mechanically ventilated patients with chronic obstructive pulmonary disease. Intensive Care Med 30:1311–1318
Kondili E, Prinianakis G, Alexopoulou C, Vakouti E, Klimathianaki M, Georgopoulos D (2006) Respiratory load compensation during mechanical ventilation–proportional assist ventilation with load-adjustable gain factors versus pressure support. Intensive Care Med 32:692–699
D’Angelo E, Robatto FM, Calderini E, Tavola M, Bono D, Torri G, Milic-Emili J (1991) Pulmonary and chest wall mechanics in anesthetized paralyzed humans. J Appl Physiol 70:2602–2610
Brochard L (2002) Intrinsic (or auto-) positive end-expiratory pressure during spontaneous or assisted ventilation. Intensive Care Med 28:1552–1554
Rodarte JR, Rehder K (1986) Dynamics of respiration. In: Macklem PT, Mead J (eds) Handbook of physiology. The respiratory system, section 3. Mechanics of breathing, vol 3. The American Physiological Society, Bethesda, pp 131–144
Tobin MJ, Laghi F, Brochard LJ (2009) Role of the respiratory muscles in acute respiratory failure of COPD: lessons from weaning failure. J Appl Physiol 107:962–970
Parthasarathy S, Jubran A, Laghi F, Tobin MJ (2007) Sternomastoid, rib cage, and expiratory muscle activity during weaning failure. J Appl Physiol 103:140–147
Conti G, Dell’Utri D, Vilardi V, De Blasi RA, Pelaia P, Antonelli M, Bufi M, Rosa G, Gasparetto A (1993) Propofol induces bronchodilation in mechanically ventilated chronic obstructive pulmonary disease (COPD) patients. Acta Anaesthesiol Scand 37:105–109
Kondili E, Prinianakis G, Athanasakis H, Georgopoulos D (2002) Lung emptying in patients with acute respiratory distress syndrome: effects of positive end-expiratory pressure. Eur Respir J 19:811–819
Thille AW, Cabello B, Galia F, Lyazidi A, Brochard L (2008) Reduction of patient–ventilator asynchrony by reducing tidal volume during pressure support ventilation. Intensive Care Med 34:1477–1486
de Wit M, Miller KB, Green DA, Ostman HE, Gennings C, Epstein SK (2009) Ineffective triggering predicts increased duration of mechanical ventilation. Crit Care Med 37:2740–2745
Jubran A, Tobin MJ (1997) Pathophysiologic basis of acute respiratory distress in patients who fail a trial of weaning from mechanical ventilation. Am J Respir Crit Care Med 155:906–915
Brochard L, Pluskwa F, Lemaire F (1987) Improved efficacy of spontaneous breathing with inspiratory pressure support. Am Rev Respir Dis 136:411–415
Acknowledgments
The authors would like to thank Prof. M. Younes for providing the PVI monitor and helpful suggestions.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kondili, E., Alexopoulou, C., Xirouchaki, N. et al. Estimation of inspiratory muscle pressure in critically ill patients. Intensive Care Med 36, 648–655 (2010). https://doi.org/10.1007/s00134-010-1753-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1753-4