Abstract
Objective
To explore the user-friendliness and ergonomics of seven new generation intensive care ventilators.
Design
Prospective task-performing study.
Setting
Intensive care research laboratory, university hospital.
Methods
Ten physicians experienced in mechanical ventilation, but without prior knowledge of the ventilators, were asked to perform eight specific tasks [turning the ventilator on; recognizing mode and parameters; recognizing and setting alarms; mode change; finding and activating the pre-oxygenation function; pressure support setting; stand-by; finding and activating non-invasive ventilation (NIV) mode]. The time needed for each task was compared to a reference time (by trained physiotherapist familiar with the devices). A time >180 s was considered a task failure.
Results
For each of the tests on the ventilators, all physicians’ times were significantly higher than the reference time (P < 0.001). A mean of 13 ± 8 task failures (16%) was observed by the ventilator. The most frequently failed tasks were mode and parameter recognition, starting pressure support and finding the NIV mode. Least often failed tasks were turning on the pre-oxygenation function and alarm recognition and management. Overall, there was substantial heterogeneity between machines, some exhibiting better user-friendliness than others for certain tasks, but no ventilator was clearly better that the others on all points tested.
Conclusions
The present study adds to the available literature outlining the ergonomic shortcomings of mechanical ventilators. These results suggest that closer ties between end-users and manufacturers should be promoted, at an early development phase of these machines, based on the scientific evaluation of the cognitive processes involved by users in the clinical setting.
Similar content being viewed by others
Introduction
In the technologically complex environment of a busy intensive care unit (ICU), the rapid multi-tasking required of healthcare providers is a source of incidents [1], 31–67% of them stemming from human errors [2, 3]. Respiratory care including mechanical ventilation, which accounts for approximately 25% of the daily ICU workload [4] constitutes one of the main activities associated with human error [2, 4, 5]. A lack of experience and training in the proper use of mechanical ventilators seem to be major contributing factors to these incidents [5, 6]. The absence of standardized user interface and poor ergonomics of some machines are likely to increase the risk of incidents, especially when caregivers must interact with them under stressful conditions [7, 8]. Indeed, ergonomics have been shown to play a major role in the safety with which a medical device can be used [7, 9, 10]. Two recent studies have outlined the lack of user-friendliness of turbine-based pressure-generating home care ventilators (so-called bilevel ventilators) [11] and ICU ventilators [12]. The purpose of the present study is to explore the user-friendliness and ergonomics of seven ICU ventilators when physicians experienced in mechanical ventilation were asked to perform eight specific tasks without prior knowledge of the machines. The rationale was to reproduce the fairly common situation of a physician called at the bedside to perform an urgent task on an unfamiliar ventilator, such as might occur during a night shift.
Materials and methods
The study was performed in the ICU research laboratory of a university hospital. ICU ventilators commonly used in Europe and available for testing were used: Elysée (Saime-Resmed, North Ryde, Australia), EngstromCarestation (GE Healthcare, Fairfield, Conn., USA), Evita XL (Draeger, Lubeck, Germany), Servo I (Maquet, Solna, Sweden), G5 (Hamilton, Rhäzüns, Switzerland), Avea (Viasys, Palm Springs, CA, USA), PB 840 (Puritan-Bennett, Covidien, Boulder, CO, USA).
Ten physicians (5 pulmonologists, 5 anesthesiologists) participated in the study, all with prior knowledge of mechanical ventilation (pulmonologists: home care and ICU ventilators; anesthesiologists: anesthesiology and ICU ventilators) but unfamiliar with the tested machines.
Test procedure
The methodology was based on that of a previous study on home-care ventilators [11].
Each ventilator was equipped with a standard double limb circuit and connected to a test lung model (Pneu View AI 2601I TTL, Michigan Instruments, Grand Rapids, MI, USA) described in previous studies [13, 14].
The physicians had to consecutively accomplish eight different tasks on each ventilator in a random order. The time to perform each task was measured with a precision stopwatch by the tester and recorded. An arbitrary upper limit of 3 min was set, at and above which task failure was declared. The tester’s time to accomplish each task was used as the reference [11]. Tasks to accomplish (for details see ESM): (1) turning the ventilator on, (2) recognizing mode and parameters (3) recognizing and setting alarms, (4) mode change, (5) finding and activating the pre-oxygenation function, (6) pressure support setting, (7) stand by, (8) finding and activating the non-invasive ventilation (NIV) mode.
Physicians were asked to grade their subjective impression of overall difficulty of interaction with each device on a scale of 0 (very easy) to 10 (very difficult) [11]. Finally, a difficulty index (DI) was computed for each ventilator: DI = (total time for 8 tasks (s) × n failures)/1,000.
Statistics
Time values are expressed as median (interquartile range). Other values are expressed as mean (SD). Details in ESM.
Results
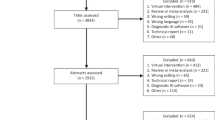
Overall results
For each of the tests, all physicians’ times were significantly higher than the reference time (P < 0.001). A mean of 13 (8) task failures was observed by ventilator (16%), one machine (Avea) exhibiting 28 failures (Table 1). Most often failed tasks: recognizing the mode and parameters (15), pressure support setting (19) and finding and activating the NIV mode (22).
Table 2 shows the mean values for the difficulty score for each ventilator.
Figure 1 in the ESM shows the box-plot of total time needed to complete the eight tasks for each machine.
Box-plot presentation of time needed per ventilator for the execution of the eight tasks. Upper series of graphs Tasks 1 (turning the ventilator on) and 2 (recognizing mode and parameters). Filled triangle Reference time; *P < 0.001 versus all other ventilators except Evita XL. # P < 0.001 versus all other ventilators except EngstromCarestation. Tasks 3 (recognizing and setting alarms) and 4 (mode change). Filled triangle Reference time; *P < 0.01 versus all other ventilators. § P < 0.05 versus all other ventilators; # P < 0.05 versus all other ventilators except PB 840; † P < 0.05 versus all other ventilators except Avea. Lower series of graphs Tasks 5 (finding and activating the pre-oxygenation function) and 6 (pressure support setting). No data are shown for the Avea, because all physicians failed the task on this machine. Filled triangle Reference time Tasks 7 (stand-by) and 8 (Finding and activating the NIV mode). Filled triangle Reference time; *P < 0.001 versus all other ventilators
Specific tasks
Times needed for task completion are shown in Fig. 1, and details of results indicated in the ESM.
(1) Turning the ventilator on: the shortest time was obtained with the Elysée (P < 0.0001). Failure to turn on the Servo i occured with 50% of physicians; (2) recognizing mode and parameters: the times of the Engström Carestation and Evita XL were significantly shorter (P < 0.001); (3) recognizing and setting alarms: very few failures were observed for this task (Table 1); (4) mode change: the shortest time was documented with the EngströmCarestation, the longest with the Avea and PB840 (P < 0.01); (5) finding and activating the pre-oxygenation function: only one failure was observed (Table 1). The median time was the closest to the reference time. No significant difference between ventilators was found; (6) pressure support setting: no significant difference was observed between ventilators. All physicians failed to set pressure support on the Avea; (7) stand by: significantly lower times were measured for the Servo i and G5 (P < 0.001). Six physicians failed the task with the Elysée; (8) finding and activating the NIV mode: significantly lower times were measured for the Servo i and G5 (P < 0.001).
There was a strong correlation between the rating by physicians and the DI (P < 0.001).
Discussion
Some limitations of the study sould be pointed out (details discussed in the ESM). First, our study population was made up of pulmonologists and anesthesiologists who do not use ICU ventilators in their daily practice. Second, the tasks we chose were arbitrarily defined, given the absence of a validated protocol for such tests. Third, the DI has not been formally validated. Fourth, failure was defined as the need for ≥3 min to complete the task, which might seem arbitrary. Finally, not all ventilators available in Europe could be tested due to availability and feasibility issues.
Our results illustrate that many new generation ventilators present poor ergonomics, leading to delayed or impossible user–machine interactions, which could prove critical in an emergency when, for instance, the ventilator cannot be turned on. Likewise several long delays observed could be unacceptable in clinical use, as illustrated by two examples. First, turning on the ventilator. The Elysee can be turned on very quickly: as soon as it is powered, an on-screen message appears, reading “to switch on press the button”, and an arrow showing its location. At the other end of the spectrum, tortuous paths must be followed, such as performing several actions in different panels (Avea, EngströmCarestation), double validation (on-screen and on the side of the ventilator, PB840) or finding the switch concealed behind a small sliding cover (Servo i). There is, of course, a logical safety goal here which is avoiding the accidental switching off of the machine. However, in the interest of safety, one might devise an asymetric procedure, i.e. difficult to switch off and easy and quick to switch on. While it is difficult to pinpoint the optimal time to switch on a ventilator, it is intuitive that shortest is best. In the study by Gonzalez-Bermejo et al. [11], most domiciliary ventilators could be switched on within 40 s, more quickly than most of the machines tested in this study. On the other hand, in the study performed on four ICU ventilators by Uzawa et al. [12], 60–70% of the times spent to switch on the ventilator were above 2 min, higher than in our study. The difference may be due to the lower level of experience of the physicians in that study [12].
Second, the high error rate (30–40%) and long delay (60–150 s) to correctly identify the ventilatory mode and set/measured parameters constitue another ergonomic shortcoming. By comparison, in their study on home ventilators, Gonzalez-Bermejo et al. [11] found a 49% rate of erroneous assessment of mode and settings, median times ranging from 47 to 71 s, while this specific task was not reported by Uzawa et al. [12] with ICU machines. Clear display and ease of ventilator mode recognition should be a priority in ventilator design and selection, given the safety issues involved [15], and there is obviously room for improvement.
The ergonomic aspects of medical devices [9, 10, 16], and the potential contribution of their shortcomings to incidents have been outlined in the literature [7, 17]. In particular, the often confusing aspects of the human–computer interface, designed by engineers with insufficient input from end-users as to the realities of their working environment, can lead to solutions which, while making sense in the development laboratory, prove inadequate in the clinical setting [7, 17, 18]. On the other hand, by studying how end-users commit mistakes [8] and cope with ergonomic shortcomings [18], and using this data during the development phase of medical devices [10], valuable information can be provided to manufacturers leading to improved user–device interaction [19, 20]. A good example of this approach has been provided by work done on infusion pumps, known for the key role of ergonomic factors in their safe use in patients [19, 20].
At present, ventilator manufacturers include clinicians in the process of ventilator design and development, an approach for which they are to be commended. However, based on the above discussion and on the results of the present study and the two other trials on this topic [11, 12], it seems reasonable to recommend that ties between manufacturers and end-users be strengthened, care being taken to ensure that this tight cooperation occurs at a very early stage of development, when major interface changes are still possible. Ideally, this type of cooperation should integrate modern concepts of cognitive psychology in analyzing the user–machine interaction [8, 16].
One important point is, of course, that adequate training of all caregivers in the proper use of a ventilator should be a prerequisite in any ICU, which machine user-friendliness cannot be expected to replace. Proper ergonomics are, in our view, complementary to basic training.
In conclusion, the present study adds to the available literature outlining the ergonomic shortcomings of mechanical ventilators. These results suggest that closer ties between end-users and manufacturers should be promoted, at an early development phase of these machines, based on the scientific evaluation of the cognitive processes involved by users in the clinical setting. This approach would likely contribute to an overall improvement in ventilator ergonomics and the avoidance of some of the pitfalls highlighted by our results and those of others, in turn leading to enhanced safety.
References
Rothschild JM, Landrigan C, Cronin J, Kaushal R, Lockley S, Burdick E, Stone P, Lilly C, Katz J, Czeisler CA, Bates D (2005) The critical care safety study: the incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med 33(8):1694–1700
Bracco D, Favre J, Bissonnette B, Wasserfallen J, Revelly J, Ravussin P, Chiolero R (2001) Human errors in a multidisciplinary intensive care unit: a 1-year prospective study. Intensive Care Med 27(1):137–145
Giraud T, Dhainaut JF, Vaxelaire JF, Joseph T, Journois D, Bleichner G, Sollet JP, Chevret S, Monsallier JF (1993) Iatrogenic complications in adult intensive care units: a prospective two-center study. Crit Care Med 21(1):40–51
Donchin Y, Gopher D, Olin M, Badihi Y, Biesky M, Sprung C, Pizov R, Cotev S (1995) A look into the nature and causes of human errors in the intensive care unit. Crit Care Med 23(2):294–300
Wright D, Mackenzie S, Buchan I, Cairns C, Price L (1991) Critical incidents in the intensive therapy unit. Lancet 338(8768):676–678
HO JCA (2002) Preventing ventilator-related deaths and injuries. Jt Comm Perspect 22(4):14–15
Horsky J, Zhang J, Patel V (2005) To err is not entirely human: complex technaology and user cognition. J Biomed Inf 38:264–266
Zhang J, Patel V, Johnson T, Shortliffe E (2004) A cognitive taxonomy of medical errors. J Biomed Inf 37:193–204
Buckle P, Clarkson P, Coleman R, Ward J, Anderson J (2006) Patient safety, design and ergonomics. Appl Ergonomics 37:491–500
Martin J, Norris B, Murphy E, Crowe J (2008) Medical device development: the challenge for ergonomics. Appl Ergonomics 39:271–283
Gonzalez-Bermejo J, Laplanche V, Husseini F, Duguet A, Derenne J, Similowski T (2006) Evaluation of the user-friendliness of 11 home mechanical ventilators. Eur Respir J 27(6):1236–1243
Uzawa Y, Yamada Y, Suzukawa M (2008) Evaluation of the user interface simplicity in the modern generation of mechanical ventilators. Respir Care 53(3):329–337
Battisti A, Tassaux D, Janssens J, Michotte J, Jaber S, Jolliet P (2005) Performance characteristics of ten recent bilevel ventilators: a comparative bench study. Chest 127:1784–1792
Vignaux L, Tassaux D, Jolliet P (2007) Performance of noninvasive ventilation modes on ICU ventilators during pressure support: a bench model study. Intensive Care Med 33(8):1444–1451
Grace K (1998) The ventilator: selection of mechanical ventilators. Crit Care Clin 14:563–580
Wilson J (2000) Fundamentals of ergonomics in theory and practice. Appl Ergonomics 31:557–567
Zhang J, Johnson T, Patel V, Kubose T (2003) Using usability heuristics to evaluate patient safety of medical devices. J Biomed Inf 36:23–30
Obradovich J, Woods D (1996) Users as designers: how people cope with poor HCI design in computer-based medical devices. Hum Factors 38:574–592
Garmer K, Liljegren E, Osvalder A, Dahlman S (2002) Application of usability testing to the development of medical equipment. Usability testing of a frequently used infusion pump and a new user interface for an infusion pump developed with a human factors approach. Int J Ind Ergon 29:145–149
Garmer K, Ylvén J, Karlsson M (2004) User participation in requirements elicitation comparing focus group interviews and usability tests for eliciting usability requirments for medical equipment: a case study. Int J Ind Ergon 33:85–98
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: doi:10.1007/s00134-009-1581-6.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vignaux, L., Tassaux, D. & Jolliet, P. Evaluation of the user-friendliness of seven new generation intensive care ventilators. Intensive Care Med 35, 1687–1691 (2009). https://doi.org/10.1007/s00134-009-1580-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1580-7