Abstract
Objective
To assess the use of hyperventilation and the adherence to Brain Trauma Foundation-Guidelines (BTF-G) after traumatic brain injury (TBI).
Setting
Twenty-two European centers are participating in the BrainIT initiative.
Design
Retrospective analysis of monitoring data.
Patients and participants
One hundred and fifty-one patients with a known time of trauma and at least one recorded arterial blood–gas (ABG) analysis.
Measurements and results
A total number of 7,703 ABGs, representing 2,269 ventilation episodes (VE) were included in the analysis. Related minute-by-minute ICP data were taken from a 30 min time window around each ABG collection. Data are given as mean with standard deviation. (1) Patients without elevated intracranial pressure (ICP) (<20 mmHg) manifested a statistically significant higher PaCO2 (36 ± 5.7 mmHg) in comparison to patients with elevated ICP (≥20 mmHg; PaCO2: 34 ± 5.4 mmHg, P < 0.001). (2) Intensified forced hyperventilation (PaCO2 ≤ 25 mmHg) in the absence of elevated ICP was found in only 49 VE (2%). (3) Early prophylactic hyperventilation (<24 h after TBI; PaCO2 ≤ 35 mmHg, ICP < 20 mmHg) was used in 1,224 VE (54%). (4) During forced hyperventilation (PaCO2 ≤ 30 mmHg), simultaneous monitoring of brain tissue pO2 or SjvO2 was used in only 204 VE (9%).
Conclusion
While overall adherence to current BTF-G seems to be the rule, its recommendations on early prophylactic hyperventilation as well as the use of additional cerebral oxygenation monitoring during forced hyperventilation are not followed in this sample of European TBI centers.
Descriptor
Neurotrauma
Similar content being viewed by others
Introduction
Moderate (PaCO2 31–35 mmHg) and forced (PaCO2 ≤ 30 mmHg) hyperventilations have been widely used in the past for the treatment of elevated intracranial pressure (ICP) [1–5]. While cerebral vasoconstriction induced by hypocarbia can effectively lower ICP by reducing cerebral blood volume, the risk of reducing cerebral blood flow below its critical limit has always been a focus of clinical concern and scientific investigation. As a result of experimental and advanced clinical studies using multimodal cerebral monitoring technology, it was hypothesized that hyperventilation in traumatic brain injury (TBI) has potentially more deleterious than beneficial effects [2, 6–11].
Consequently, the second edition (2000) [12] of the Brain Trauma Foundation-Guidelines (BTF-G) restricted the use of hyperventilation for the treatment of TBI.Footnote 1. Hyperventilation down to a PaCO2 ≤ 25 mmHg in the absence of elevated ICP was strongly discouraged (level I evidence). Due to the already markedly reduced CBF in the first 24 h after trauma [13], moderate prophylactic hyperventilation (PaCO2 31–35 mmHg) should not be applied (level II evidence). Furthermore, if forced hyperventilation (PaCO2 ≤ 30 mmHg) is inevitable to control the ICP, careful monitoring of tissue perfusion and oxygenation is recommended to avoid induction of cerebral hypoxia or even ischemia (level III evidence). The recently published third edition (2007) of the BTF-G [14] maintains these recommendations with a reduced evidence level class and acknowledges the lack of randomized clinical trials that directly link hyperventilation to patient outcome. As a result, uncertainty remains about optimal ventilation treatment in TBI. Considering the long tradition of hyperventilation as a measure to treat elevated ICP, it is of interest to assess its current use in TBI and whether or not current ventilation treatment is in line with BTF-G.
The TBI database from the BrainIT initiative [15] is an excellent tool to investigate this topic. The BrainIT initiative (http://www.brainit.org), a collaboration of 38 European centers, has developed a core data set including intensive care minute-by-minute monitoring data [16]. It has set up a validated database of 202 TBI patients drawn from 22 data contributing centers that is open for members as a tool for retrospective analysis, hypothesis generation and the development, testing, and validation of new data analysis methodologies.
In this retrospective multi-center database study, we analyzed more than 7,000 arterial blood–gas analyses (ABG) to determine whether hyperventilation practice after TBI in Europe is in accordance with the BTF-G (second edition 2000) to be in effect during the time of data collection.
Materials and methods
TBI data
In this retrospective database study, demographic, physiological and clinical data from 202 patients in the current BrainIT database collected from 22 European centers were analyzed. Data were collected in a time frame between July 2003 and June 2005. Data validation was accomplished using a stepwise multi-level process [17]. For all data entered into the common database, four levels of data validation were progressively applied. After ensuring that the data conversion stage functioned correctly (validation level I), all non-numeric categorical core data were scrutinized for transcribing the errors (validation level II). Level three validation involved the conversion of units to BrainIT units, if required. Finally, level four validation was performed by human data validators who checked the accuracy of a random subset of 20% of the initial data against source documents.
Data were visualized and post-processed using a custom-made software library (BrainITLib) written in JAVA programming language. All datasets with a known time of trauma and at least one ABG were included into the final analysis. Data exchange was facilitated by a structured query language (SQL) database running on an industrial standard PC.
Analysis of PaCO2 and concomitant ICP values
Arterial blood–gas collection was performed according to local clinical practice under the modalities (analyzers and pharmaceuticals) and regulations (calibration intervals) in effect at each contributing center. For each ABG in our dataset, the time interval between trauma and probe collection was calculated. Next, to compensate for the lack of continuous PaCO2 data, a descriptive statistical analysis of minute-by-minute ICP values within a 30 min interval around the time of each ABG collection (15 min prior- and 15 min post-ABG, respectively) was performed with calculation of mean, standard deviation, and outliers for each 30 min interval. If the mean ICP during the interval was 20 mmHg or above, the ABG was classified by our software as being taken at a time of elevated ICP.
Definition of ventilation types classified by PaCO2
Normoventilation was defined as a CO2 partial pressure between 36 and 45 mmHg (4.8–6.0 kPa). To further differentiate the intensity of the hyperventilation performed, we introduced the terms "moderate, forced, and intensified forced" hyperventilation and set the ranges at 35–31, 30–26, and <26 mmHg (4.7–4.0, 3.9–3.5, and <3.5 kPa), respectively (Table 1).
Analysis of presumptive ventilation performed
Consecutive ABGs having a PaCO2 within the same predefined PaCO2 range (Table 1) were automatically consolidated into a ‘ventilation episode’ (VE) and analyzed conjointly. Consequently, by definition, a VE comprises a series of one or more serial ABGs within the same PaCO2 class. In total 2,269 VE were documented. For each VE, time, length, and ICP statistics were recorded and subsequently analyzed.
Statistical analysis
Data were analyzed using SPSS® Version 14.0.1 (SPSS Inc., Chicago, IL, USA). Interval data are given as means with standard deviation. Box-and-whiskers plots were used to represent the distribution of continuous data. In these graphs, boxes represent the interquartile range, the median is given as a solid line and the mean is shown as a dashed line. Whisker caps mark the 10th and 90th percentiles, whereas solid diamonds indicate the 5th and 95th percentiles. The normal distribution of quantitative data was tested with the Kolmogorov–Smirnov test. When comparing results between individual groups, non-parametric tests (Wilcoxon–Rank–Sum, Kruskal–Wallis H) were applied with alpha set at the 0.05 level. In case of multiple statistical testing, P values were adjusted according to the Bonferroni correction.
Results
Patient demographics
Exactly 151 out of 202 patients met the inclusion criteria of a known time of trauma and at least one recorded PaCO2 value. The final dataset contained data from 124 male and 27 female individuals treated in 17 European trauma centers. Patients aged from 1 to 83 (median 34) years. Classified by the initial Glasgow Coma Scale (GCS) score, 90 (60%) patients suffered severe (GCS 3–8), 23 (15%) moderate (GCS 9–12), and 18 (12%) mild (GCS 13–15) TBIs. Those patients with moderate or mild TBI deteriorated later on and required intubation and ventilation. For 20 patients (13%), no initial GCS was available.
Distribution of recorded PaCO2 values
The median interval between consecutive ABGs was 2.8 h with an interquartile range of 1.2–4.5 h. The mean PaCO2 value of all 7,703 ABGs was 35.8 ± 5.6 mmHg.
The histogram of all recorded blood–gas analyses (Fig. 1) demonstrated a skewed (P < 0.001) distribution of PaCO2 values with a maximum in the range between 30 and 35 mmHg. At the border between moderate and forced hyperventilation (30 mmHg), a sharp decline in PaCO2 value frequency was noted. In contrast, the transition between PaCO2 values representing moderate hyperventilation and normoventilation showed a less steep decline.
PaCO2 histogram of 7,703 blood–gas analyses; frequency bars are drawn as dotted (hypoventilation), streaked (normoventilation) or in shades of grey (moderate, forced or intensified forced hyperventilation) according to the PaCO2 ranges defined in Table 1. The distribution of PaCO2 values is skewed with a maximum in the range between 30 and 35 mmHg (moderate hyperventilation). At the border between moderate and forced hyperventilation (30 mmHg), a sharp decline in PaCO2 value frequency is noted. In contrast, the decline between PaCO2 values representing moderate hyperventilation and normoventilation is less steep
PaCO2 values and ICPs following TBI
Simultaneous ICP data were available for 4,691 out of 7,703 ABGs. The average number of minute-by-minute ICP data points available for each patient was 7,762. Patients without elevated ICP (<20 mmHg) presented a small but statistically significant higher PaCO2 (36 ± 5.7 mmHg) in comparison to patients with elevated ICP (≥20, 34 ± 5.4 mmHg; P < 0.001).
Early after TBI (<24 h), mean PaCO2 was 36 ± 5.6 mmHg and was unchanged (mean 36 ± 6.3 mmHg) after 24 h. Figure 2 demonstrates the distribution of PaCO2 (mmHg) data within and after 24 h following TBI. The data are further subdivided for ABGs taken at the time of normal (<20 mmHg) or elevated ICP (≥20 mmHg). In the first 24 h, the PaCO2 in patients without elevated ICP was 36 ± 6.2 mmHg. In patients with elevated ICP, the PaCO2 was lower at 34 ± 6.7 mmHg (P < 0.017). The mean PaCO2 within 24 h post-trauma in patients with normal ICP (ICP < 20 mmHg) was 36 ± 5.6 mmHg and higher (P < 0.001) than compared to those with elevated ICP (≥20 mmHg) 34 ± 5.2 mmHg.
PaCO2 after traumatic brain injury in 151 patients; the left half of the graph illustrates blood–gas analyses (ABG) taken within 24 h after trauma, the right half (streaked boxplots) represents ABGs taken at a later time. In episodes of elevated ICP (≥20 mmHg) PaCO2 was significantly lower compared to periods of normal ICP (<20 mmHg)
Ventilation of TBI patients by analysis of ventilation episodes
We further evaluated the use of hyperventilation by aggregating the relative time of ventilation within each ventilation type as defined in Table 1. Figure 3 visualizes the distribution of ventilation time in patients per center among the participating BrainIT centers. Individual centers contributed an unequal number of patients; the top five centers made up for 70% of the total ventilation time and for 72% of all patients. To compensate for differences in individual ventilation time per patient, the relative time shares were calculated for each patient and then averaged for each center.
Ventilation types in patients among 17 centers; centers are represented by the number of contributed patients (x-axis). Averaged proportions of time of the distinct ventilation types (hyper-, normo- or hypoventilation) for each center are given on the y-axis. All centers hyperventilated their patients approximately half of the total ventilation time. Individual differences between centers existed, but the trend toward liberal use of hyperventilation was noted for all centers. One center, marked with an X, did not apply normoventilation at all
In summary, all centers hyperventilated their patients (PaCO2 ≤ 35 mmHg) approximately half of the total ventilation time (mean 55 ± 22.6%). Forced and intensified forced hyperventilations (PaCO2 ≤ 30 mmHg) were used in 18 ± 17.8% of the time. During VE without elevated ICP, prophylactic moderate hyperventilation was performed in some 40% of VE, with no significant difference in respect to time since trauma. Forced or intensified forced hyperventilation was used for the time period early after trauma (≤24 h) in 15% and later on (>24 h) in 20% of VE. During episodes of elevated ICP (ICP ≥ 20 mmHg), hyperventilation was found in 83% of VE early (≤24 h) and in 67% of VE late after trauma (>24 h).
Concomitant ICP therapy and cerebral monitoring during (intensified) forced hyperventilation
During forced hyperventilation (331 VE), mannitol was the most widely utilized concomitant ICP therapy (25% of 331 VE). Barbiturates and CSF drainage were employed in only 4% (13 VE). Additional cerebral monitoring during forced hyperventilation (PaCO2 ≤ 30 mmHg), as suggested by the BTF-G, was applied only rarely, e.g., monitoring of brain tissue pO2 in 5% (17 VE) and jugular vein oxygen saturation measurement in 4% (13 VE).
Discussion
This study attempted to elucidate the adherence to BTF-G concerning hyperventilation [12] (second edition 2000) in European trauma centers. We retrospectively analyzed the BrainIT database containing the clinical data of 202 TBI patients.
The BTF-G advise that prophylactic hyperventilation must not be used within the first 24 h after trauma. This class II recommendation is based on clinical data demonstrating an already markedly decreased CBF within the first 24 h after trauma [13] which could be aggravated by applying hyperventilation. Although statistically significant differences in PaCO2 with regard to ICP and time since trauma (within 24 h or later) were found in our study, these differences were very small and of limited clinical relevance.
When analyzing the pooled data, the PaCO2 was distributed predominantly in the ranges of normoventilation and moderate hyperventilation (Fig. 1). The sharp decline in PaCO2 frequency at the threshold of forced hyperventilation (30 mmHg) points to the fact that avoiding hyperventilation below this value seems to be an issue of major concern for treating physicians. Whether this threshold represents the amount of hyperventilation that is still considered "safe" by physicians cannot be answered. Additional studies to explore physicians’ attitude toward hyperventilation and the BTF-G are needed. Furthermore, individual differences between centers existed, but the trend towards liberal use of hyperventilation was noted for all centers. One center, did not apply normoventilation at all. Due to the blinding policy used by the BrainIT initiative, identification of this specific center to elucidate the reason for this practice is not applicable. Additionally, there was considerable variation between centers in the number of patients contributed to the study. Five out of 17 centers contributed 70% of the total data points. Due to general BrainIT policy, each center was allowed to contribute an arbitrary number of patients to the database. Varying intervals between BGA collections and differences in total ventilation time caused an inevitable heterogeneity in the number of data points provided by each patient. An attempt to attenuate this problem was done by analyzing the ventilation episodes and not single BGAs and by calculating ‘relative ventilation times’ for each PaCO2 class and patient. The rationale for this approach was the fact that the VE acts as a compensation for possible biases due to changing intervals between individual ABG collections. These factors as well as local differences in hyperventilation practice may have had a non-negligible influence on our results and constitute an inherent limitation in the design of the study.
Nonetheless, in our subsequent analysis of VE, hyperventilation treatment (PaCO2 ≤ 35 mmHg) has been confirmed as a common therapy regimen accounting for more than half of the total VE. As seen from our analysis, moderate and even forced hyperventilation was often applied in the absence of elevated ICP. This ‘prophylactic’ use of hyperventilation clearly deviates from the BTF-G. In summary, it has to be concluded that hyperventilation is still a common practice in the treatment of TBI patients in Europe.
Our findings are in line with prior studies. In a 1997 survey among North American neurosurgeons, more than one-third of the participants stated that they still use prophylactic hyperventilation in the management of their patients [18]. Although Wilkins et al. [19] reported an increasing awareness of the potentially negative consequences of hyperventilation in a survey among neurosurgical centers in the UK and Ireland, Thomas et al. [20] found inappropriately high assisted-ventilation rates and low end-tidal CO2 (etCO2) below 30 mmHg in 60–70% of thirty-seven patients transferred by helicopter to an US urban level I trauma center. Furthermore, Warner et al. [21] reported a distribution of PaCO2 values of 492 intubated TBI patients referred to an US level I trauma center similar to our histogram (Fig. 1). Approximately 16% of these patients revealed PaCO2 levels below 30 mmHg, while in 30% PaCO2 stretched from 30 to 35 mmHg.
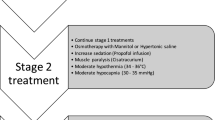
The use of forced hyperventilation has been accepted as second tier therapy in the year 2000 BTF-G as a treatment option if conventional therapy (sedation, paralysis, osmotherapy, CSF drainage, and moderate hyperventilation) has failed. Our analysis of concomitant ICP therapy revealed that forced hyperventilation is often used without prior mannitol therapy and thus against the year 2000 BTF-G ICP treatment algorithm.
The lack of concomitant standard ICP therapy and the high incidence of prophylactic hyperventilation have to raise questions whether the induction of hypocarbia may have been non-intentional in some cases. In our study, all patients were ventilated according to individual institution policy. Mechanical as well as metabolic factors necessitate a constant adjustment of ventilation parameters to the current physiologic demand of the patient. Long intervals between BGA collections give rise to the possibility of ‘accidental’ hyperventilation. Although etCO2 monitoring can provide continuous data, it has its own problems and pitfalls [22]. Elevated alveolar dead space can lead to a significant gradient between PaCO2 and etCO2. Reliance on etCO2 monitoring without frequent calibration by ABG may thus lead to inadvertent hypoventilation. Only 63 out of 151 patients in the study received continuous recording of etCO2 and merely 34 of these within the first 24 h post-trauma. Speculating that ventilator settings often aim at the lower threshold of normoventilation points to another possible cause of ‘accidental’ hyperventilation.
In summary, we conclude that hyperventilation is used extensively, intentionally or otherwise, in the treatment of severe TBI in Europe, while the overall adherence to current BTF-G seems to be the rule, their recommendations on early prophylactic hyperventilation (PaCO2 ≤ 35 mmHg) and additional cerebral oxygenation monitoring during forced hyperventilation are not followed in the majority of European TBI centers.
No conclusions can be drawn on the question whether hyperventilation has benefited or harmed the patients included in our study. This would require a separate investigation in a dedicated clinical trial which has not yet been performed.
In a more recent animal study using a multimodal cerebral monitoring setup, Clausen et al. found very variable individual response to hyperventilation with a marked effect on cerebral blood flow and metabolism. They conclude that any degree of hyperventilation without advanced neuromonitoring cannot be considered as a safe practice and should either be avoided or used with extreme caution [11]. In a recent prospective interventional study Coles et al. [8] showed that levels of hypocarbia of 30 mmHg may result in significant regional ischemia within 10 days of head injury. Therefore, without a proven benefit of hyperventilation on outcome and serious doubts about the safety of this procedure, we advocate that, in the absence of elevated ICP, the principle of ‘primum nil nocere’ should be obeyed. Thus, on current evidence and acknowledging the lack of sufficient prospective randomized clinical trials, PaCO2 should probably not be intentionally reduced below 35 mmHg. In contrast, our study conversely demonstrates that hyperventilation is widespread in European neurointensive care units.
Notes
Standard, class I evidence: no hyperventilation (PaCO2 ≤ 25 mmHg) when ICP is not increased; Guideline, class II evidence: no prophylactic hyperventilation with a PaCO2 ≤ 35 mmHg within the first 24 h post trauma; Option, class III evidence: hyperventilation may be necessary for short periods with acute neurologic deterioration or for longer periods as second tier therapy, Pt iO2 or SjvO2 monitoring is necessary at PaCO2 ≤ 30 mmHg [11]
References
Heffner JE, Sahn SA (1983) Controlled hyperventilation in patients with intracranial hypertension. Application and management. Arch Intern Med 143:765–769
Stringer WA, Hasso AN, Thompson JR, Hinshaw DB, Jordan KG (1993) Hyperventilation-induced cerebral ischemia in patients with acute brain lesions: demonstration by xenon-enhanced CT. AJNR Am J Neuroradiol 14:475–484
Lundberg N, Kjallquist A, Bien C (1959) Reduction of increased intracranial pressure by hyperventilation. A therapeutic aid in neurological surgery. Acta Psychiatr Scand 34:1–64
Oertel M, Kelly DF, Lee JH, Glenn TC, Vespa PM, Martin NA (2002) Can hyperventilation improve cerebral microcirculation in patients with high ICP? Acta Neurochir Suppl 81:71–72
Oertel M, Kelly DF, Lee JH, McArthur DL, Glenn TC, Vespa P, Boscardin WJ, Hovda DA, Martin NA (2002) Efficacy of hyperventilation, blood pressure elevation, and metabolic suppression therapy in controlling intracranial pressure after head injury. J Neurosurg 97:1045–1053
Muizelaar JP, Marmarou A, Ward JD, Kontos HA, Choi SC, Becker DP, Gruemer H, Young HF (1991) Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg 75:731–739
Marion DW, Puccio A, Wisniewski SR, Kochanek P, Dixon CE, Bullian L, Carlier P (2002) Effect of hyperventilation on extracellular concentrations of glutamate, lactate, pyruvate, and local cerebral blood flow in patients with severe traumatic brain injury. Crit Care Med 30:2619–2625
Coles JP, Fryer TD, Coleman MR, Smielewski P, Gupta AK, Minhas PS, Aigbirhio F, Chatfield DA, Williams GB, Boniface S, Carpenter TA, Clark JC, Pickard JD, Menon DK (2007) Hyperventilation following head injury: effect on ischemic burden and cerebral oxidative metabolism. Crit Care Med 35:568–578
Coles JP, Minhas PS, Fryer TD, Smielewski P, Aigbirihio F, Donovan T, Downey SP, Williams G, Chatfield D, Matthews JC, Gupta AK, Carpenter TA, Clark JC, Pickard JD, Menon DK (2002) Effect of hyperventilation on cerebral blood flow in traumatic head injury: clinical relevance and monitoring correlates. Crit Care Med 30:1950–1959
Manley GT, Hemphill JC, Morabito D, Derugin N, Erickson V, Pitts LH, Knudson MM (2000) Cerebral oxygenation during hemorrhagic shock: perils of hyperventilation and the therapeutic potential of hypoventilation. J Trauma 48:1025–1032
Clausen T, Scharf A, Menzel M, Soukup J, Holz C, Rieger A, Hanisch F, Brath E, Nemeth N, Miko I, Vajkoczy P, Radke J, Henze D (2004) Influence of moderate and profound hyperventilation on cerebral blood flow, oxygenation and metabolism. Brain Res 1019:113–123
Bullock MR, Chesnut RM, Clifton GL, Ghajar J, Marion DW, Narayan RK, Newell DW, Pitts LH, Rosner MJ, Walters BC, Wilberger JE (2000) Management and prognosis of severe traumatic brain injury. Part I: guidelines for the management of severe traumatic brain injury. J Neurotrauma 17:513–520
Bouma GJ, Muizelaar JP, Choi SC, Newlon PG, Young HF (1991) Cerebral circulation and metabolism after severe traumatic brain injury: the elusive role of ischemia. J Neurosurg 75:685–693
Bullock MR, Povlishock JT (2007) Guidelines for the management of severe traumatic brain injury. J Neurotrauma 24(Suppl 1):S87–S90
Piper I, Citerio G, Chambers I, Contant C, Enblad P, Fiddes H, Howells T, Kiening K, Nilsson P, Yau YH (2003) The BrainIT group: concept and core dataset definition. Acta Neurochir (Wien) 145:615–628
Chambers IR, Barnes J, Piper I, Citerio G, Enblad P, Howells T, Kiening K, Matterns J, Nilsson P, Ragauskas A, Sahuquillo J, Yau YH (2006) BrainIT: a trans-national head injury monitoring research network. Acta Neurochir Suppl 96:7–10
Barnes J, Chambers I, Piper I, Citerio G, Contant C, Enblad P, Fiddes H, Howells T, Kiening K, Nilsson P, Yau YH (2005) Accurate data collection for head injury monitoring studies: a data validation methodology. Acta Neurochir Suppl 95:39–41
Marion DW, Spiegel TP (2000) Changes in the management of severe traumatic brain injury: 1991–1997. Crit Care Med 28:16–18
Wilkins IA, Menon DK, Matta BF (2001) Management of comatose head-injured patients: are we getting any better? Anaesthesia 56:350–352
Thomas SH, Orf J, Wedel SK, Conn AK (2002) Hyperventilation in traumatic brain injury patients: inconsistency between consensus guidelines and clinical practice. J Trauma 52:47–52
Warner KJ, Cuschieri J, Copass MK, Jurkovich GJ, Bulger EM (2007) The impact of prehospital ventilation on outcome after severe traumatic brain injury. J Trauma 62:1330–1336
Kerr ME, Zempsky J, Sereika S, Orndoff P, Rudy EB (1996) Relationship between arterial carbon dioxide and end-tidal carbon dioxide in mechanically ventilated adults with severe head trauma. Crit Care Med 24:785–790
Acknowledgments
We would like to thank all the staff of the BrainIT centers for the time and help in collecting the data. This work was supported by European Community, Frame Work Five Programme, Quality of Life and Management of Living Resources—brain-monitoring with information technology; an open, internet based trans-national collaborative infrastructure for supporting assessment of health care technologies in brain-injured patients, developing and testing an improved coordination structure/grant no. QLRT-2001-01160.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendix
Appendix
Investigators and participating centers
Barcelona, Spain: Prof. Sahuquillo; Cambridge, UK: Prof. Pickard; Edinburgh, UK: Prof. Whittle; Glasgow, UK: Mr. Dunn; Gothenburg, Sweden: Dr. Rydenhag; Heidelberg, Germany: Dr. Kiening; Iasi, Romania: Dr. Iencean; Kaunas, Lithuania: Prof. Pavalkis; Leipzig, Germany: Prof. Meixensberger; Leuven, Belgium: Prof. Goffin; Mannheim, Germany: Prof. Vajkoczy; Milano, Italy: Prof. Stocchetti; Monza, Italy: Dr. Citerio; Newcastle upon Tyne, UK: Dr. Chambers; Novara, Italy: Prof. Della Corte; Southampton, UK: Dr. Hell; Uppsala, Sweden: Prof. Enblad; Torino, Italy: Dr. Mascia; Vilnius, Lithuania: Prof. Jarzemaskas; Zürich, Switzerland: Prof. Stocker.
BrainIT Steering Group members
IR Chambers, Newcastle upon Tyne; G Citerio, Monza; P Enblad, Uppsala; BA Gregson, Newcastle upon Tyne; T Howells, Uppsala; K Kiening, Heidelberg; J Mattern, Heidelberg; P Nilsson, Uppsala; I Piper, Glasgow; A Ragauskas, Kaunas; J Sahuquillo, Barcelona; YH Yau, Edinburgh.
Rights and permissions
About this article
Cite this article
Neumann, JO., Chambers, I.R., Citerio, G. et al. The use of hyperventilation therapy after traumatic brain injury in Europe: an analysis of the BrainIT database. Intensive Care Med 34, 1676–1682 (2008). https://doi.org/10.1007/s00134-008-1123-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1123-7