Abstract
Objective
Alterations in coagulation, including elevated pulmonary and systemic concentrations of urokinase, are frequent in patients with acute lung injury (ALI). Urokinase potentiates neutrophil activation and contributes to the severity of pulmonary injury in preclinical models of ALI. The objective of this study was to examine associations between polymorphisms and haplotypes of urokinase with risk for and outcomes from ALI.
Design
Prospective cohorts of healthy European-American adults and those with infection-associated ALI.
Setting
Academic medical centers participating in NIH funded studies of low tidal volume ventilation for ALI.
Patients
Controls were 175 healthy European-American subjects. Patients were 252 individuals with infection-associated ALI, prospectively followed for 60 days for mortality.
Interventions
Genetic polymorphisms and haplotypes in the urokinase gene were determined.
Measurements and main results
Six polymorphisms, rs1916341, rs2227562, rs2227564, rs2227566, rs2227571, and rs4065, defining 98% of all urokinase haplotypes, were analyzed. There were no statistically significant associations between any single urokinase polymorphism or haplotype and risk for developing ALI. In contrast, there was a statistically significant relationship between the CGCCCC haplotype and both 60-day mortality and ventilator-free days that remained present in a multivariate analysis controlling for age and sex (p = 0.033 for 60-day mortality and < 0.001 for ventilator-free days).
Conclusions
These results identify a specific urokinase haplotype as a genetic risk factor for higher mortality and more severe clinical outcome in patients with infection-associated ALI.
Similar content being viewed by others
Introduction
Acute lung injury (ALI) is clinically defined by hypoxemia and bilateral infiltrates on chest radiographs without evidence of left-sided cardiac failure [1]. Histopathologic examination of the lungs obtained from experimental models or patients with ALI demonstrates interstitial edema, microvascular thrombi, neutrophil accumulation, and alveolar fibrin formation [2, 3]. Alterations in pathways related to coagulation and fibrinolysis are present in patients with ALI and are postulated to play an important role in mediating the microvascular and inflammatory changes in the lungs that accompany ALI [3, 4].
Urokinase is a serine protease that cleaves plasminogen to generate plasmin, a potent mediator of fibrinolysis [5, 6]. In addition to its fibrinolytic properties, urokinase has recently been shown to enhance neutrophil activation and participate in the development of experimental ALI [7]. Bronchoalveolar lavage concentrations of urokinase are increased in human volunteers after local instillation of LPS into the lung [8]. In the setting of pneumonia, urokinase levels are elevated in the involved segments of the lungs [9, 10]. Both serum and bronchoalveolar lavage concentrations of urokinase are increased in patients with ALI [9, 11]. In patients with ALI or severe sepsis, levels of plasminogen activator inhibitor 1 (PAI-1), which inhibits the fibrinolytic properties of urokinase through binding to its protease domain, are usually increased to a greater degree than are those of urokinase, resulting in a procoagulant state that is present both systemically and in the lungs [12–15]. However, portions of the urokinase molecule that are not involved in fibrinolysis or interaction with PAI-1, such as its kringle sequence, also have proinflammatory effects and participate in the pathogenesis of experimental ALI [16, 17].
The urokinase gene is located in the 10q24 chromosomal region [18]. Polymorphisms in urokinase appear to be functionally significant and are associated with diseases involving altered immune regulation, including asthma, rheumatoid arthritis, type 1 diabetes, colorectal cancer, and late-onset Alzheimer's disease [19–24]. Therefore, given the importance of alterations in coagulation, neutrophil activation, and inflammation in ALI, and the ability of urokinase to participate in all of these processes, we hypothesized that genetic variants in urokinase might be associated with susceptibility to or outcome from ALI. To explore this hypothesis, we examined outcome in a well-characterized cohort of patients with infection-associated ALI, and found that a specific urokinase haplotype was associated with survival and need for prolonged ventilatory support in ALI.
Materials and methods
Volunteer selection
Healthy white volunteers, 19–89 years of age, were recruited to determine urokinase polymorphisms. The sample included 98 males (mean age 30.0 ± 6.7 years, range 19–57 years) and 77 females (mean age 32.0 ± 10.0 years, range 19–89 years). The study was approved by the institutional review board, and each volunteer signed an informed consent document.
Patients with acute lung injury
All patients included in this study had been enrolled in NIH ARDS Network studies and had received low tidal volume ventilation using previously published protocols [25]. All patients were European-American and had infection-associated ALI, as characterized by either systemic or localized pulmonary infection as the investigator-identified primary etiology for ALI. ALI was defined by standard criteria. Septic shock was defined as a systolic blood pressure of < 90 mmHg for at least 30 min despite fluid replacement or the use of inotropic support to maintain blood pressure. Exclusion criteria included age below 18 years, a neurologic condition that could impair weaning from mechanical ventilation, severe chronic respiratory disease, severe chronic liver disease (defined as a Child–Pugh score of > 10), burns covering > 30% of total body surface area, malignancy or other irreversible condition for which the mortality at 6 months was estimated to be above 50%, use of high-dose immunosuppressive therapy, and a history of lung or bone marrow transplantation. Table 2 shows characteristics of the patients. This genetic analysis study was approved by the University of Colorado Health Sciences Center and the University of Alabama at Birmingham institutional review boards. Consent was obtained from all patients or their surrogates as part of their enrollment into the NIH protocols.
Allelic discrimination
Real-time polymerase chain reaction (PCR) allelic discrimination assays were developed by the assay-by-design service offered by Applied Biosystems (Foster City, CA). Probe and primer combinations were designed for the six urokinase single nucleotide polymorphisms (SNPs), rs1916341, rs2227562, rs2227564, rs2227566, rs2227568, and rs4065, which capture all haplotypes with frequency greater than 2.2% in the European-American population as per the Seattle SNPs database (Table 1). PCR reactions were performed in a final volume of 25 μl, which consisted of 1–25 ng of DNA diluted in dH2O, 12.5 μl of 2 × TaqMan Universal PCR Master Mix, and 1.25 μl of 20 × TaqMan SNP genotyping Assay Mix. PCR was performed using an Applied Biosystems 7300 Real-Time PCR system. There were no missing genotypes. An approach similar to the one proposed by Scheet and Stephens [26] was used to check for genotyping errors. There was no statistical significant evidence for the appearance of genotyping errors in the data.
Single-marker and haplotype analysis
For single-marker analysis, two approaches were used to analyze the data. The first was based on a set of score tests for binary response, as described by Zhao et al. [27–29], without considering other covariates; the other analysis was based on a regression approach where the other covariates were included [30–32]. For haplotype analysis, two regression-based methods (for binary, continuous, and time-to-event responses) as described by Schaid et al. [33] and Lake et al. [34] and by Lin and Zeng [30–32] where the other covariates were included and excluded, were employed. For haplotype analysis, we performed both joint-effect analysis and separate-effect analysis. All significance levels reported are two-tailed.
Results
Characteristics of the patient population
A total of 252 European-American patients with infection-associated acute lung injury (ALI) were available for analysis (Table 2). The primary source of infection was the lungs, involving 55% of these patients. Men and women were equally represented in the ALI patients. An additional population of 175 healthy volunteers was recruited for comparison.
Case–control comparison of urokinase polymorphisms and haplotypes in healthy control and acute lung injury populations
Prior to analysis, Hardy–Weinberg equilibrium (HWE) was tested using the approaches described by Guo and Thompson [35] as implemented in Arlequin version 3.0a [http://anthro.unige.ch/software/arlequin/]. SNP 5 showed marginal departure from HWE (unadjusted p-value 0.046) on the pooled cases and controls. When tested on cases and controls separately, HWE held at all SNPs (unadjusted p-values > 0.092). For this analysis, all patients and controls were included.
As an initial approach, single-marker analysis of the six urokinase polymorphisms was undertaken, using the methods by Zhao et al. [28, 29], as implemented in the Nonlinear program. As shown in Table 3, there were no significant differences between the frequency of polymorphisms in the control population and patients with ALI. Analysis, with age and sex included, was also performed, using the approach described by Lin and Zeng [30–32], as implemented in the HAPSTAT program. No significant evidence of association between any polymorphism and risk for ALI was found with this approach.
Six haplotypes with frequencies larger than 0.01 for urokinase were identified (Table 4). Haplotype analyses were conducted using both a joint-effects model [30–34], in which all haplotypes except the most frequent one are compared to the most frequent haplotype simultaneously, and a separate-effect model [30–32] in which each haplotype is compared to all of the other haplotypes (i.e., all other haplotypes pooled together as baseline), one at a time, after controlling for age and sex. The HAPSTAT [27–29] and HAPLO.STATS [33, 34] programs were used for haplotype analysis. Neither analysis found significant association between any haplotype and risk for ALI.
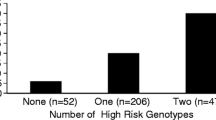
Associations of urokinase polymorphisms and haplotypes with outcome from acute lung injury
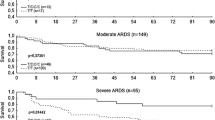
In order to test the association of genetic markers with outcome from ALI, an analysis of the patients with infection-induced ALI was undertaken. Of note, SNPs 1 (rs1916341) and 4 (rs2227566) were found to be in complete linkage disequilibrium (LD), and were in very strong LD with SNP 5 (rs2227571). Therefore, the results for SNPs 1 and 4 are identical in all single-marker analyses (Table 5). Unlike age, which was significantly associated with 60-day survival among patients with ALI, as well as ventilator-free days and the presence of fluid-unresponsive shock, there was no statistically significant association between any of the six single polymorphisms examined and 60-day survival from ALI, using either 60-day mortality as a binary response or as a time-to-event survival response. This lack of association was present with or without the inclusion of other covariates in the analysis. In contrast, when haplotype analyses were performed using a dominant-effect model, the haplotype CGCCCC was found to be significantly associated with 60-day mortality, either compared to the most frequent haplotype (AGCTTT) in a joint-effect model (p = 0.033) (Table 6), or when compared to all other haplotypes in a separate-effect model (p = 0.021), after controlling for age and sex. The association between the CGCCCC haplotype and mortality at 60 days was also weakly supported by data from a survival analysis (p = 0.077).
Measurement of ventilator-free days is a clinically relevant parameter in patients with ALI, providing an assessment of the duration of requirement for mechanical ventilation. As was the case for 60-day mortality, no individual urokinase polymorphism was significantly associated with ventilator-free days. In contrast, there was a statistically significant relationship between the CGCCCC haplotype and ventilator-free days, either compared to the most frequent haplotype (AGCTTT) in the joint-effect model (p < 0.001), or compared to all other haplotypes in the separate-effect model (p = 0.047), after controlling for age and sex.
Days of shock were assessed both by sequential daily measurement of vital signs, with a systolic blood pressure of less than 90 despite adequate fluid administration, being considered as shock, or by the Brussels system, with requirement for vasopressor support to maintain normotension being required for scoring as shock. However, using either of these criteria, there were no statistically significant relationships between shock and any single polymorphism or haplotype. In particular, for the CGCCCC haplotype, which was significantly associated with 60-day mortality and ventilator-free days, the p-values for association with shock were > 0.11 using the Brussels scoring system and > 0.26 using vital signs, in all the analyses performed, even after controlling for the covariates of sex and age.
In our haplotype analyses, we used the joint-effect model as our primary analysis and the separate-effect model as confirmation. Since SNP 5 showed marginal departure from HWE in the pooled data, to be prudent, we also conducted analyses with SNP5 excluded. The results were similar to these presented above (data not shown).
Discussion
In this study, a significant relationship was demonstrated between a specific urokinase haplotype, CGCCCC, and increased 60-day mortality as well as requirement for prolonged mechanical ventilation among patients with ALI. This association between the CGCCCC haplotype and worse outcome from ALI was present both when the haplotype was considered alone and also in multivariate analysis, when both age and sex were included as covariates. While the CGCCCC urokinase haplotype was associated with outcome from ALI, there was no apparent relationship between this haplotype and susceptibility to ALI, with no significant differences in the frequencies of the haplotype in healthy controls and patients with ALI. Such findings indicate that while genetic alterations in urokinase contribute to outcome in ALI, urokinase haplotypes do not constitute a risk factor for this life-threatening condition.
There is only limited information about urokinase polymorphisms and inflammatory conditions. In the present study, we examined a series of tagged and common polymorphisms that were previously found in the Seattle SNPs database to characterize all haplotypes present in more than 2.2% of the European-American population. The six haplotypes identified in the present study encompass more than 98% of the subjects included in the control and ALI populations examined, providing a comprehensive assessment of the relationships between genetic variation in urokinase and ALI.
While there have been reports of associations between the nonsynonymous C → T polymorphism rs2227564 within intron 7 and Alzheimer's disease, type 1 diabetes, and colonic cancer, this has not been a universal finding [19, 20, 22, 23, 36]. Although previous studies have shown associations between polymorphisms in proteins related to coagulation and mortality associated with sepsis [37, 38], there are no data on the relationship between urokinase polymorphisms and outcome from critical illness. In the present study, no association was found between specific urokinase polymorphisms and either the incidence or the outcome of ALI.
In addition to its well-characterized fibrinolytic activity, urokinase has additional properties that are likely to make it a relevant mediator of acute inflammatory processes, such as ALI. In particular, the high concentrations of urokinase present in the lungs after endotoxin exposure [8, 39], during pneumonia [9, 40, 41], and with ALI [3, 12, 14, 42–45], even if lacking fibrinolytic activity because of association with PAI-1, may still contribute to the accumulation of large numbers of activated neutrophils which appear to play an important role in the pathophysiology of ALI. Urokinase, through interactions of its growth factor domain with the classic uPA receptor (uPAR), has potent chemotactic effects on neutrophils [46–49]. The kringle domain of urokinase has recently been shown to have proinflammatory activity, enhancing neutrophil release of cytokines relevant to ALI, such as TNF-α and IL-1α [17]. In murine models, antibodies to the urokinase kringle domain diminish the severity of LPS-induced ALI [16]. Even though circulating and pulmonary levels of PAI-1 are elevated in ALI, resulting in inhibition of the fibrinolytic properties of urokinase, PAI-1 binds to the urokinase protease domain, without apparent interaction with either the kringle or growth factor domains [14, 50, 51]. Therefore, interactions between PAI-1 and urokinase would not be expected to modify effects leading to neutrophil activation or accumulation in the lungs that are modulated by urokinase domains distinct from the protease domain.
To minimize confounding variables, such as racial admixture and heterogeneous etiologies for ALI, the present study focused on European-American patients whose primary etiology for ALI was infection. Management of mechanical ventilation was standardized for these patients as a result of being enrolled in studies in which protocols were used with levels of compliance exceeding 98%. In particular, all patients included in this study had been enrolled in NIH ARDS Network studies and received low tidal volume ventilation, presently considered the optimal ventilatory therapy for ALI [1]. However, because of the restricted patient population included in this analysis, it is presently unknown whether the association between the CGCCCC urokinase haplotype and outcome from ALI is present in other groups of patients with ALI or is limited only to European-Americans with infection-associated ALI. An additional limitation of the present study is that neither urokinase levels nor activities were determined, so there is no information concerning the functional significance of the urokinase haplotype identified as being associated with worse outcome from ALI.
The findings of the present study, showing that genetic alterations in urokinase are associated with higher mortality and the need for prolonged mechanical ventilation in patients with ALI, provide an additional indication of the importance of coagulation and its regulation in contributing to the pathophysiology of ALI and other organ system dysfunction resulting from severe infection. In addition, these results not only may have diagnostic utility in identifying ALI patients at increased risk of worse outcomes, but also may have additional future implications since they may facilitate the targeting of therapies specific for modulating injurious effects of urokinase or related molecules to appropriate patient populations.
References
Bernard GR (2005) Acute respiratory distress syndrome: a historical perspective. Am J Respir Crit Care Med 172:798–806
Matthay MA, Zimmerman GA (2005) Acute lung injury and the acute respiratory distress syndrome: four decades of inquiry into pathogenesis and rational management. Am J Respir Cell Mol Biol 33:319–327
Ware LB, Camerer E, Welty-Wolf K, Schultz MJ, Matthay MA (2006) Bench to bedside: targeting coagulation and fibrinolysis in acute lung injury. Am J Physiol Lung Cell Mol Physiol 291:L307–L311
Ware LB, Matthay MA, Parsons PE, Thompson BT, Januzzi JL, Eisner MD (2007) Pathogenetic and prognostic significance of altered coagulation and fibrinolysis in acute lung injury/acute respiratory distress syndrome. Crit Care Med 35:1821–1828
Blasi F, Carmeliet P (2002) uPAR: a versatile signalling orchestrator. Nat Rev Mol Cell Biol 3:932–943
Idell S (2002) Endothelium and disordered fibrin turnover in the injured lung: newly recognized pathways. Crit Care Med 30:S274–S280
Abraham E, Gyetko MR, Kuhn K, Arcaroli J, Strassheim D, Park JS, Shetty S, Idell S (2003) Urokinase-type plasminogen activator potentiates lipopolysaccharide-induced neutrophil activation. J Immunol 170:5644–5651
van der Poll T, Levi M, Nick JA, Abraham E (2005) Activated protein C inhibits local coagulation after intrapulmonary delivery of endotoxin in humans. Am J Respir Crit Care Med 171:1125–1128
Levi M, Schultz MJ, Rijneveld AW, van der Poll T (2003) Bronchoalveolar coagulation and fibrinolysis in endotoxemia and pneumonia. Crit Care Med 31:S238–S242
Choi G, Schultz MJ, van Till JW, Bresser P, van der Zee JS, Boermeester MA, Levi M, van der Poll T (2004) Disturbed alveolar fibrin turnover during pneumonia is restricted to the site of infection. Eur Respir J 24:786–789
Schultz MJ, Haitsma JJ, Zhang H, Slutsky AS (2006) Pulmonary coagulopathy as a new target in therapeutic studies of acute lung injury or pneumonia: a review. Crit Care Med 34:871–877
Groeneveld AB, Kindt I, Raijmakers PG, Hack CE, Thijs LG (1997) Systemic coagulation and fibrinolysis in patients with or at risk for the adult respiratory distress syndrome. Thromb Haemost 78:1444–1449
Prabhakaran P, Ware LB, White KE, Cross MT, Matthay MA, Olman MA (2003) Elevated levels of plasminogen activator inhibitor-1 in pulmonary edema fluid are associated with mortality in acute lung injury. Am J Physiol Lung Cell Mol Physiol 285:L20–L28
Idell S (2003) Coagulation, fibrinolysis, and fibrin deposition in acute lung injury. Crit Care Med 31:S213–S220
El Solh AA, Bhora M, Pineda L, Aquilina A, Abbetessa L, Berbary E (2006) Alveolar plasminogen activator inhibitor-1 predicts ARDS in aspiration pneumonitis. Intensive Care Med 32:110–115
Wang XQ, Bdeir K, Yarovoi S, Cines DB, Fang W, Abraham E (2006) Involvement of the urokinase kringle domain in lipopolysaccharide-induced acute lung injury. J Immunol 177:5550–5557
Kwak S-H, Mitra S, Bdeir K, Strassheim D, Park JS, Kim JK, Idell S, Cines DL, Abraham E (2005) The kringle domain of urokinase-type plasminogen activator potentiates LPS-induced neutrophil activation through interaction with {alpha}V{beta}3 integrins. J Leukoc Biol 78:937–945
Irigoyen JP, Munoz-Canoves P, Montero L, Koziczak M, Nagamine Y (1999) The plasminogen activator system: biology and regulation. Cell Mol Life Sci 56:104–132
Przybylowska K, Smolarczyk K, Kulig A, Romanowicz-Makowska H, Dziki A, Ulanska J, Pander B, Blasiak J (2002). Antigen levels of the urokinase-type plasminogen activator and its gene polymorphisms in colorectal cancer. Cancer Lett 181:23–30
Majsterek I, Przybylowska K, Mlynarski W, Drzewoski J, Blasiak J (2005) Distribution of C–>T and T–>C polymorphisms of the urokinase-type plasminogen activator gene in children with type 1 diabetes mellitus and insulin resistance. Clin Exp Med 4:202–206
Ertekin-Taner N, Ronald J, Feuk L, Prince J, Tucker M, Younkin L, Hella M, Jain S, Hackett A, Scanlin L, Kelly J, Kihiko-Ehman M, Neltner M, Hersh L, Kindy M, Markesbery W, Hutton M, de Andrade M, Petersen RC, Graff-Radford N, Estus S, Brookes AJ, Younkin SG (2005) Elevated amyloid beta protein (Abeta42) and late onset Alzheimer's disease are associated with single nucleotide polymorphisms in the urokinase-type plasminogen activator gene. Hum Mol Genet 14:447–460
Riemenschneider M, Konta L, Friedrich P, Schwarz S, Taddei K, Neff F, Padovani A, Kolsch H, Laws SM, Klopp N, Bickeboller H, Wagenpfeil S, Mueller JC, Rosenberger A, Diehl-Schmid J, Archetti S, Lautenschlager N, Borroni B, Muller U, Illig T, Heun R, Egensperger R, Schlegel J, Forstl H, Martins RN, Kurz A (2006) A functional polymorphism within plasminogen activator urokinase (PLAU) is associated with Alzheimer's disease. Hum Mol Genet 15:2446–2456
Huang CM, Chen CL, Tsai JJ, Tsai CH, Tsai FJ (2004) Association between urokinase gene 3'-UTR T/C polymorphism and Chinese patients with rheumatoid arthritis in Taiwan. Clin Exp Rheumatol 22:219–222
Begin P, Tremblay K, Daley D, Lemire M, Claveau S, Salesse C, Kacel S, Montpetit A, Becker A, Chan-Yeung M, Kozyrskyj AL, Hudson TJ, Laprise C (2007) Association of urokinase-type plasminogen activator with asthma and atopy. Am J Respir Crit Care Med 175:1109–1116
Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, Schoenfeld D, Thompson BT (2004) Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med 351:327–336
Scheet P, Stephens M (2006) A fast and flexible statistical model for large-scale population genotype data: applications to inferring missing genotypes and haplotypic phase. Am J Hum Genet 78:629–644
Zhao J, Jin L, Xiong M (2006) Test for interaction between two unlinked loci. Am J Hum Genet 79:831–845
Zhao J, Jin L, Xiong M (2006) Nonlinear tests for genomewide association studies. Genetics 174:1529–1538
Zhao JY, Xiong MM, Huang W, Wang H, Zuo J, Wu GD, Chen Z, Qiang BQ, Zhang ML, Chen JL, Ding W, Yuan WT, Xu HY, Jin L, Li YX, Sun Q, Liu QY, Boerwinkle E, Fang FD (2005) An autosomal genomic scan for loci linked to type 2 diabetes in northern Han Chinese. J Mol Med 83:209–215
Lin DY, Zeng D, Millikan R (2005) Maximum likelihood estimation of haplotype effects and haplotype-environment interactions in association studies. Genet Epidemiol 29:299–312
Zeng D, Lin DY (2005) Estimating haplotype-disease associations with pooled genotype data. Genet Epidemiol 28:70–82
Zeng D, Lin DY, Avery CL, North KE, Bray MS (2006) Efficient semiparametric estimation of haplotype-disease associations in case–cohort and nested case–control studies. Biostatistics 7:486–502
Schaid DJ, Rowland CM, Tines DE, Jacobson RM, Poland GA (2002) Score tests for association between traits and haplotypes when linkage phase is ambiguous. Am J Hum Genet 70:425–434
Lake SL, Lyon H, Tantisira K, Silverman EK, Weiss ST, Laird NM, Schaid DJ (2003) Estimation and tests of haplotype-environment interaction when linkage phase is ambiguous. Hum Hered 55:56–65
Guo SW, Thompson EA (1992) Performing the exact test of Hardy–Weinberg proportion for multiple alleles. Biometrics 48:361–372
Myers AJ, Marshall H, Holmans P, Compton D, Crook RJ, Mander AP, Nowotny P, Smemo S, Dunstan M, Jehu L, Wang JC, Hamshere M, Morris JC, Norton J, Chakraventy S, Tunstall N, Lovestone S, Petersen R, O'Donovan M, Jones L, Williams J, Owen MJ, Hardy J, Goate A (2004) Variation in the urokinase-plasminogen activator gene does not explain the chromosome 10 linkage signal for late onset AD. Am J Med Genet B Neuropsychiatr Genet 124:29–37
Manocha S, Russell JA, Sutherland AM, Wattanathum A, Walley KR (2007) Fibrinogen-beta gene haplotype is associated with mortality in sepsis. J Infect 54:572–577
Arcaroli J, Fessler MB, Abraham E (2005) Genetic polymorphisms and sepsis. Shock 24:300–312
Maris NA, de Vos AF, Bresser P, van der Zee JS, Meijers JC, Lijnen HR, Levi M, Jansen HM, van der Poll T (2005) Activation of coagulation and inhibition of fibrinolysis in the lung after inhalation of lipopolysaccharide by healthy volunteers. Thromb Haemost 93:1036–1040
Schultz MJ, Millo J, Levi M, Hack CE, Weverling GJ, Garrard CS, van der Poll T (2004) Local activation of coagulation and inhibition of fibrinolysis in the lung during ventilator associated pneumonia. Thorax 59:130–135
Rijneveld AW, Weijer S, Bresser P, Florquin S, Vlasuk GP, Rote WE, Spek CA, Reitsma PH, van der Zee JS, Levi M, van der Poll T (2006) Local activation of the tissue factor–factor VIIa pathway in patients with pneumonia and the effect of inhibition of this pathway in murine pneumococcal pneumonia. Crit Care Med 34:1725–1730
Idell S (1994) Extravascular coagulation and fibrin deposition in acute lung injury. New Horiz 2:566–574
Abraham E (2000) Coagulation abnormalities in acute lung injury and sepsis. Am J Respir Cell Mol Biol 22:401–404
Gunther A, Mosavi P, Heinemann S, Ruppert C, Muth H, Markart P, Grimminger F, Walmrath D, Temmesfeld-Wollbruck B, Seeger W (2000) Alveolar fibrin formation caused by enhanced procoagulant and depressed fibrinolytic capacities in severe pneumonia. Comparison with the acute respiratory distress syndrome. Am J Respir Crit Care Med 161:454–462
Ware LB, Bastarache JA, Wang L (2005) Coagulation and fibrinolysis in human acute lung injury: new therapeutic targets? Keio J Med 54:142–149
Gyetko MR, Sitrin RG, Fuller JA, Todd RF, Petty H, Standiford TJ (1995) Function of the urokinase receptor (CD87) in neutrophil chemotaxis. J Leukoc Biol 58:533–538
Resnati M, Guttinger M, Valcamonica S, Sidenius N, Blasi F, Fazioli F (1996) Proteolytic cleavage of the urokinase receptor substitutes for the agonist-induced chemotactic effect. Embo J 15:1572–1582
Mondino A, Resnati M, Blasi F (1999) Structure and function of the urokinase receptor. Thromb Haemost [Suppl 1] 82:19–22
Sitrin RG, Pan PM, Blackwood RA, Huang J Petty HR (2001) Cutting edge: evidence for a signaling partnership between urokinase receptors (CD87) and L-selectin (CD62L) in human polymorphonuclear neutrophils. J Immunol 166:4822–4825
Shetty S, Bdeir K, Cines DB, Idell S (2003) Induction of plasminogen activator inhibitor-1 by urokinase in lung epithelial cells. J Biol Chem 278:18124–18131
Reuning U, Magdolen V, Hapke S, Schmitt M (2003) Molecular and functional interdependence of the urokinase-type plasminogen activator system with integrins. Biol Chem 384:1119–1131
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by NIH grant R01 HL76206.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Arcaroli, J., Sankoff, J., Liu, N. et al. Association between urokinase haplotypes and outcome from infection-associated acute lung injury. Intensive Care Med 34, 300–307 (2008). https://doi.org/10.1007/s00134-007-0930-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0930-6