Abstract
Objective
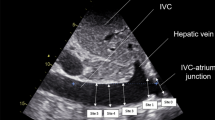
To investigate whether the respiratory variation in inferior vena cava diameter (ΔDIVC) could be related to fluid responsiveness in mechanically ventilated patients.
Design
Prospective clinical study.
Setting
Medical ICU of a non-university hospital.
Patients
Mechanically ventilated patients with septic shock (n=39).
Interventions
Volume loading with 8 mL/kg of 6% hydroxyethylstarch over 20 min.
Measurements and results
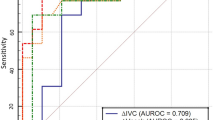
Cardiac output and ΔDIVC were assessed by echography before and immediately after the standardized volume load. Volume loading induced an increase in cardiac output from 5.7±2.0 to 6.4±1.9 L/min (P<0.001) and a decrease in ΔDIVC from 13.8±13.6 vs 5.2±5.8% (P<0.001). Sixteen patients responded to volume loading by an increase in cardiac output ≥15% (responders). Before volume loading, the ΔDIVC was greater in responders than in non-responders (25±15 vs 6±4%, P<0.001), closely correlated with the increase in cardiac output (r=0.82, P<0.001), and a 12% ΔDIVC cut-off value allowed identification of responders with positive and negative predictive values of 93% and 92%, respectively.
Conclusion
Analysis of ΔDIVC is a simple and non-invasive method to detect fluid responsiveness in mechanically ventilated patients with septic shock.



Similar content being viewed by others
References
Michard F, Teboul JL (2002) Predicting fluid responsiveness in ICU patients. A critical analysis of the evidence. Chest 121:2000–2008
Morgan BC, Martin WE, Hornbein TF, Crawford EW, Guntheroth WG (1966) Hemodynamic effects of intermittent positive pressure respiration. Anesthesiology 27:584–590
Natori H, Tamaki S, Kira S (1979) Ultrasonographic evaluation of ventilatory effect on inferior vena caval configuration. Am Rev Respir Dis 1979; 120:421–427
Perel A (1998) Assessing fluid responsiveness by the systolic pressure variation in mechanically ventilated patients. Anesthesiology 89:1309–1310
Tavernier B, Makhotine O, Lebuffe G, Dupont J, Scherpereel P (1998) Systolic pressure variation as a guide to fluid therapy in patients with sepsis-induced hypotension. Anesthesiology 89:1313–1321
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, Richard C, Pinsky MR, Teboul JL (2000) Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med 162:134–138
Feissel M, Michard F, Mangin I, Ruyer O, Faller JP, Teboul JL (2001) Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest 119:867–873
Berkenstadt H, Margalit N, Hadani M, Friedman Z, Segal E, Villa Y, Perel A (2001) Stroke volume variation as a predictor of fluid responsiveness in patients undergoing brain surgery. Anesth Analg 92:984–989
Reuter DA, Felbinger TW, Schmidt C, Kilger E, Goedje O, Lamm P, Goetz AE (2002) Stroke volume variations for assessment of cardiac responsiveness to volume loading in mechanically ventilated patients after cardiac surgery. Intensive Care Med 28:392–398
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G, International sepsis definitions conference (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International sepsis definitions conference. Intensive Care Med 29:530–538
Theres H, Binkau J, Laule M, Heinze R, Hundertmark J, Blobner M, Erhardt W, Baumann G, Stangl K (1999) Phase-related changes in right ventricular cardiac output under volume-controlled mechanical ventilation with positive end-expiratory pressure. Crit Care Med 27:953–958
Mitaka C, Nagura T, Sakanishi N, Tsunoda Y, Amaha K (1989) Two-dimensional echocardiographic evaluation of inferior vena cava, right ventricle, and left ventricle during positive-pressure ventilation with varying levels of positive end-expiratory pressure. Crit Care Med 17:205–210
Magder S, Georgiadis G, Cheong T (1992) Respiratory variations in right atrial pressure predict the response to fluid challenge. J Crit Care 7:76–85
Jardin F, Delorme G, Hardy A, Auvert B, Beauchet A, Bourdarias JP (1990) Reevaluation of hemodynamic consequences of positive pressure ventilation: emphasis on cyclic right ventricular afterloading by mechanical lung inflation. Anesthesiology 72:966–970
Permutt, S, Howell JB, Proctor DF, Riley RL (1961) Effects of lung inflation on static pressure-volume characteristics of pulmonary vessels. J Appl Physiol 16:64–70
Squara P, Dhainaut JF, Schremmer B, Sollet JP, Bleichner G (1990) Decreased paradoxic pulse from increased venous return in severe asthma. Chest 97:377–383
Vieillard-Baron A, Augarde R, Prin S, Page B, Beauchet A, Jardin F (2001) Influence of superior vena caval zone condition on cyclic changes in right ventricular outflow during respiratory support. Anesthesiology 95:1083–1088
Vieillard-Baron A, Chergui K, Augarde R, Prin S, Page B, Beauchet A, Jardin F (2003) Cyclic changes in arterial pulse during respiratory support revisited by Doppler echocardiography. Am J Respir Crit Care Med 168:671–676
Amoore JN, Santamore WP (1994) Venous collapse and the respiratory variability in systemic venous return. Cardiovasc Res 28:472–479
Michard F, Teboul JL, Richard C (2003) Influence of tidal volume on stroke volume variation. Does it really matter? Intensive Care Med 29:1613
Acknowledgements
The authors thank Dr. Luca Bigatello (Massachusetts General Hospital-Harvard Medical School, Boston, MA) for reviewing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Feissel, M., Michard, F., Faller, JP. et al. The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med 30, 1834–1837 (2004). https://doi.org/10.1007/s00134-004-2233-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2233-5