Abstract
Aims
This study examined the association between the Major Depression Inventory (MDI) and the Schedules for Clinical Assessment in Neuropsychiatry (SCAN).
Methodology
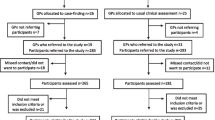
A questionnaire including the MDI was sent out to an adult population and was completed by a total of 10448 persons. Psychiatrists used SCAN and interviewed a subsample (n=1093).
Results
The specificity of the MDI was 0.22, the sensitivity 0.67 and Kappa 0.25 when Major Depression according to SCAN was considered as the index of validity, and with all depressive disorders the specificity was 0.44, the sensitivity 0.51 and Kappa 0.33. Higher educated persons and those with reported disability were less likely to be false negatives. The sensitivity and specificity for different cut-off scores when using the MDI total score were calculated.
Conclusion
The result from this study suggests that, when MDI is used in population-based samples, cut-off scores rather than the algorithm for depression should be used. The optimal cut-off score must be chosen according to the aims of the study.
Similar content being viewed by others
References
American Psychiatric Association (1994) Diagnostic and Statistical manual of Mental Disorders. American Psychiatric Association (4th ed, rev). Washington, DC, APA
Anthony JC, Folstein MF, Romanovski AJ, Von Korff MR, Nestadt GR, Chahal R, Merchant A, Brown CH, Sapiro S, Kramer M, Gruenberg EM (1985) Comparison of the lay Diagnostic Interview Schedule and a standardized psychiatric diagnosis: experience in eastern Baltimore. Arch Gen Psychiatry 42:667–675
Bech P, Stage K, Nair NPV, Larsen JK, Kragh-Sorensen P, Gjeriss P (1997) The Major Depression Rating Scale (MDS). Inter-rater reliability and validity across different settings in randomised moclobemide trials. J Affect Disord 42:39–48
Bech P, Wermuth, L (1998) Applicability and validity of the Major Depression Inventory in patients with Parkinson’s disease. Nord J Psychiatry 52:305–309
Bech P, Rasmussen NA, Raabaer K, Olsen L, Noerholm V, Abilgard W (2001) The sensitivity and specificity of the Major Depression Inventory using the Present State Examination as the index of diagnostic validity. J Aff Disord 66:159–164
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571
Beck AT, Steer RA, Ball R, Ranieri W (1996) Comparison of the Beck Depression inventories IA and II in psychiatric outpatients. J Pers Assess 132:381–385
Eaton WW, Neufeld K, Chen L-S, Cai G (2000) A comparison of self-reports and clinical diagnostic interviews for depression. Arch Gen Psychiatry 57:217–222
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36
Helzer JE, Robins LN, McEvoy LT, Spitznagel EL, Stoltzman RK, Farmer A, Brockington IF (1985) A comparison of clinical and Diagnostic Interview Schedule diagnoses: re-examination of lay-interviewed cases in the general population. Arch Gen Psychiatry 42:657–666
Hsiao JK, Bartko JJ, Potter WZ (1989) Diagnosing diagnoses. Arch Gen Psychiatry 46:664–668
Janca A, Kastrup M, Katschnig H, Lopez-Ibor JJ Jr, MezzIich JE, Sartorius N (1996) The World Health Organisation Short Disability Assessment Schedule (WHO DAS-S): a tool for the assessment of difficulties in selected areas of functioning of patients with mental disorders. Soc Psychiatry Psychiatr Epidemiol 31(6):349–354
Leentjens AFG, Verhey FRJ, Lousberg R, Spitsbergen H, Wilmink FW (2000) The validity of the Hamilton and Montgomery-Åsberg depression rating scales as screening for depression and diagnostic tools for depression in Parkinson’s disease. Int J Ger Psychiatry 15:644–649
Regier DA, Kaelber CT, Rae DS, Farmer ME, Kanauper B, Kessler RC, Norquist GS (1998a) Limitations of diagnostic criteria and assessment instruments for mental disorders. Arch Gen Psychiatry 55:109–115
Regier DA (1998b) In reply, Letters to the editor. Arch Gen Psychiatry 55:1146–1147
Robins LN, Helzer JE, Croughan J, Ratcliff KS (1981) National Institute of Mental Health Diagnostic Interview Schedule: history, characteristics and validity. Arch Gen Psychiatry 38:381–389
Tomov T, Nikolov V (1990) Reliability of SCAN categories and scores: results of the field trials. In: Stefanis CN, Rabavilas AD, Soldatos CR (eds) Vol 1: Classification and Psychopathology, Child Psychiatry, Substance Use: Proceedings of the VIII World Congress of Psychiatry, Athens,12–19 October 1989. Amsterdam, the Netherlands: Excerpta Medica
Wing JK, Babor T, Brugha T, Burke J (1990) SCAN. Schedules for Clinical Assessment in Neuropsychiatry. Arch Gen Psychiatry 47(6):589–593
Zung WWK (1965) A self-rating depression scale. Arch Gen Psychiatry 12:63–70
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Forsell, Y. The Major Depression Inventory versus Schedules for Clinical Assessment in Neuropsychiatry in a population sample. Soc Psychiat Epidemiol 40, 209–213 (2005). https://doi.org/10.1007/s00127-005-0876-3
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s00127-005-0876-3