Abstract
Aims/hypothesis
There are strong associations between measures of inflammation and type 2 diabetes, but the causal directions of these associations are not known. We tested the hypothesis that common gene variants known to alter circulating levels of inflammatory proteins, or known to alter autoimmune-related disease risk, influence type 2 diabetes risk.
Methods
We selected 46 variants: (1) eight variants known to alter circulating levels of inflammatory proteins, including those in the IL18, IL1RN, IL6R, MIF, PAI1 (also known as SERPINE1) and CRP genes; and (2) 38 variants known to predispose to autoimmune diseases, including type 1 diabetes. We tested the associations of these variants with type 2 diabetes using a meta-analysis of 4,107 cases and 5,187 controls from the Wellcome Trust Case Control Consortium, the Diabetes Genetics Initiative, and the Finland–United States Investigation of NIDDM studies. We followed up associated variants (p < 0.01) in a further set of 3,125 cases and 3,596 controls from the UK.
Results
We found no evidence that inflammatory or autoimmune disease variants are associated with type 2 diabetes (at p ≤ 0.01). The OR observed between the variant altering IL-18 levels, rs2250417, and type 2 diabetes (OR 1.00 [95% CI 0.99–1.03]), is much lower than that expected given (1) the effect of the variant on IL-18 levels (0.28 SDs per allele); and (2) estimates, based on other studies, of the correlation between IL-18 levels and type 2 diabetes risk (approximate OR 1.15 [95% CI 1.09–1.21] per 0.28 SD increase in IL-18 levels).
Conclusions/interpretation
Our study provided no evidence that variants known to alter measures of inflammation, autoimmune or inflammatory disease risk, including type 1 diabetes, alter type 2 diabetes risk.
Similar content being viewed by others
Introduction
Inflammatory and immunological factors are associated with type 2 diabetes, but the causal direction of this association is not known. Evidence for a possible causal role of inflammatory and immunological processes in type 2 diabetes comes from several sources. These include prospective studies that show raised levels of pro-inflammatory, and lower levels of anti-inflammatory, cytokines many years before the onset of type 2 diabetes [1]. Specific examples include the presence of raised circulating IL-18 [1] and macrophage migration inhibitory factor (MIF) [2] levels in the KORA study, where average follow-up time to diagnosis of type 2 diabetes is 10 years, and similar findings observed with raised C-reactive protein (CRP) or IL-6 levels in several other prospective studies [3–5]. Second, mouse knockout models of certain cytokine genes, including IL18, IL1RN, IL1A and IL1B, result in adverse effects on obesity and insulin resistance in mouse models [6–8]. For example, the CD11B (also known as MAC-1 or ITGAM) knockout mouse is susceptible to diet-induced obesity compared with wild-type litter mates [9]. A common variant in the CD11B gene has recently been established as a risk factor for systemic lupus erythematosus (SLE) [10], suggesting a possible link between autoimmune diseases and metabolic traits. Common variants in the CDKAL1 gene are associated with type 2 diabetes, psoriasis and Crohn’s disease [11], although the associated polymorphisms are different and not correlated (in linkage disequilibrium) with each other. Finally, recent data indicating a critical role for IL-1β in beta cell function [12] have led to a small randomised controlled trial of recombinant human IL-1 receptor antagonist (IL-1RA) (anakinra) treatment in type 2 diabetes that showed improved beta cell function and reduced levels of markers of systemic inflammation in 35 anakinra-administered patients with type 2 diabetes [13].
Further evidence is needed to establish whether inflammation has a causal role in type 2 diabetes in humans. Observed changes in inflammatory protein levels/concentrations with disease progression may be secondary to early disease processes and knockout animal studies suggest that if inflammatory processes have a role it is more likely to be through obesity-induced changes. Genetics studies can add to the evidence for or against the causal role of a trait in disease. This is because genetic variants cannot be influenced by disease processes and are much less likely to be confounded than non-genetic factors. This principle of ‘Mendelian randomisation’ has been used before to indicate that raised CRP levels are likely to be a consequence rather than cause of continuous metabolic traits [14].
Detailed studies of genetic variation across genes encoding inflammatory proteins have identified an increasing number of common variants that alter circulating levels of these proteins. These include variants in or near the IL18 [15–17], IL1RN [17, 18], IL6R, PAI1 (also known as SERPINE1) [17, 19], MIF [20] and CRP genes [17, 21, 22], all associated with robust statistical confidence with levels of their respective protein products. In addition the variant in IL6R is associated with IL-6 levels as well as levels of its soluble receptor (sIL-6R) [23, 24].
Recent genome-wide association (GWA) studies have resulted in a greatly increased knowledge of common gene variants that predispose to systemic or organ-specific autoimmune and inflammatory diseases. These include convincing genetic associations between variants at 30 loci, outside the HLA region, and Crohn’s disease [25, 26], type 1 diabetes [27], rheumatoid arthritis [28, 29], coeliac disease [30, 31], ankylosing spondylitis [32], SLE [10, 33, 34] and multiple sclerosis [32, 35]. Five of these loci include variants that alter the risk of more than one inflammatory disease.
It has been suggested that type 1 and type 2 diabetes share a partially overlapping aetiology [36] but there is mixed evidence to support this. Recent studies show that known type 2 diabetes variants in the TCF7L2 and FTO loci do not predispose to type 1 diabetes [37, 38] In contrast, a recent Scandinavian study indicates that individuals with adult latent autoimmune diabetes have an increased frequency of both type 1 and type 2 diabetes risk alleles [39].
In this study we aimed to provide further insight into the possible role of inflammatory and autoimmune processes in type 2 diabetes. To do this we tested the hypothesis that common gene variants known to alter either circulating levels of inflammatory proteins or autoimmune and inflammatory disease risk also alter the risk of type 2 diabetes.
Methods
Study participants
Initial type 2 diabetes GWA meta-analysis
We used the p values and ORs from a meta-analysis of three type 2 diabetes GWA scans (http://www.well.ox.ac.uk/DIAGRAM/) that had recently been carried out using 2.2 million single-nucleotide polymorphisms (SNPs) (directly typed and imputed) with 4,107 type 2 diabetes cases and 5,187 controls, to identify associations between the selected polymorphisms and type 2 diabetes. The meta-analysis included samples used in GWA scans from the Wellcome Trust Case Control Consortium (WTCCC) (1,924 type 2 diabetes cases and 2,938 population controls, all from the UK), the Diabetes Genetics Initiative (DGI) (1,022 type 2 diabetes cases and 1,075 matched controls and 326 sibships discordant for diabetes) and the Finland–United States Investigation of NIDDM Genetics (FUSION) (1,161 type 2 diabetes cases and 1,174 normal glucose-tolerant controls, from Finland) studies [40]. Each SNP passed quality control criteria in each individual type 2 diabetes GWA study, as recently described [40]. Each study analysed the data under a model that is additive on the log-odds scale. ORs from each sample, excluding the DGI sibships, were combined using a fixed-effects model [41]. Patients in the WTCCC and DGI studies positive for anti-GAD antibodies were not included [40, 42]. The FUSION GWA case sample is composed of 789 cases from FUSION and 372 cases from FINRISK 2002. FUSION cases were excluded if they were positive for anti-GAD antibodies, had a short time to onset of insulin treatment following diagnosis, or had known or probable type 1 diabetes first-degree relatives [43]. Brief details of study participants are given in Electronic supplementary material (ESM) Table 1.
Replication study participants
For replication we genotyped SNPs nominally associated with type 2 diabetes using the UK Type 2 Diabetes Genetics Consortium Collection of 3,125 cases and 3,596 controls. All study participants were recruited from the Tayside region in Dundee, Scotland and were of European origin. Cases with monogenic forms of diabetes or with a history of treatment with regular insulin therapy within 1 year of diagnosis were excluded [44]. Controls were restricted to individuals <80 years of age and participants with evidence of hyperglycaemia were excluded from the study [44]. Details are given in ESM Table 1.
SNP selection
We selected three sets of SNPs from previous studies that have either been directly genotyped [28, 30–32, 35, 40, 42, 43] or imputed in the three-study diabetes meta-analysis [40]. These included: (1) Eight SNPs previously associated with circulating IL-1RA [17, 18], sIL-6R [24, 45], IL-18 [16, 17], CRP [17], plasminogen activator inhibitor (PAI)-1 [19] or MIF levels [20]. All SNPs were ‘cis’ effects in that they were present in or near the gene that codes for the protein they are associated with. This together with the statistical confidence (p ≤ 10−5) of the associations between the SNP and protein levels means the associations are very unlikely to be false-positive results. For IL1RN and IL18 genes [16–18] there is evidence for two independent association signals (r 2 between variants <0.5) and we therefore included both the SNPs associated with respective protein levels in each case. (2) Seven SNPs from five loci: IL23R, PTPN2, PTPN22, SH2B3 and IL2RA, which are associated with more than one inflammatory/autoimmune disease [25–27, 29, 31, 32, 35]. (3) Thirty-one independently associated variants from 30 loci proven to be autoimmune disease risk variants after robust replications (overall p ≤ 10−8) and excluding the SNPs in the MHC locus. These SNPs are associated with seven diseases (Crohn’s disease, type 1 diabetes, rheumatoid arthritis, coeliac disease, ankylosing spondylitis, SLE and multiple sclerosis).
All the 46 SNPs tested for an association passed QC control criteria in each individual study, as recently described [40]. Briefly all SNPs below a minor allele frequency (MAF) of 1% were excluded from analysis and all genotyped SNPs were in Hardy–Weinberg equilibrium in each individual study (p > 10−4 for WTCCC, p ≥ 10−6 for DGI and p ≥ 10−6 for FUSION). Where genotyping data were unavailable, imputed SNPs were used for analysis as has previously been described [40]. In total 54% (25), 50% (23) and 52% (24) of the tested 46 SNPs lacked direct genotype information in the FUSION, WTCCC and DGI studies, respectively, and were therefore imputed. All imputed SNPs, except in five situations, had quality scores (r 2hat in DGI and FUSION, imputation information scores in WTCCC) >80% and all, except in 17 situations, had quality scores >90%.
Individual genotyping in the replication study
We used a p value of <0.01 in the three-way meta-analysis to take SNPs forward into the replication samples. The exception to this was SNPs in the IL1RN and IL18 genes, where we used the less stringent p < 0.1. SNPs in these two genes influence circulating levels and have a stronger prior case for their products’ involvement in type 2 diabetes given previous trial and prospective studies. Genotyping was performed by KBiosciences (Hoddesdon, UK) using their own system of fluorescence-based competitive allele-specific PCR (KASPar).
Statistics
Meta-analysis of p values using an additive effects model in WTCCC, DGI and FUSION samples has been previously described [40]. The ORs were calculated excluding the related component of the DGI study. To combine the previously published meta-analysis data with replication data we performed a meta-analysis using a fixed-effects inverse variance method using the summary ORs and 95% CIs from the three-way analysis as one study and the ORs and 95% CIs from the replication samples as a second study. This meta-analysis was performed using the ‘Metan’ module in STATA version 9.1. In the three-study meta-analysis we had 80% power to detect an OR of 1.20 for a SNP with a MAF of 0.09 (the lowest MAF of all 46 SNPs) at p = 0.05. For a more common SNP (MAF = 0.30) we had 80% power to detect an OR of 1.10 at p = 0.05. Power calculations were performed using STATA version 9.1.
Sensitivity analysis using directly genotyped SNPs
For 34 of the 46 SNPs the direct genotypes, or direct genotypes at an r 2 > 0.8 proxy, were available in the WTCCC and DGI studies (total 2,946 cases and 4,013 controls typed on the Affymetrix 500 K chip). For eight of these 34 SNPs the r 2 > 0.8 proxy was also available in FUSION. To confirm that the use of imputed data was not substantially influencing our results, we therefore repeated the analyses using only directly genotyped variants for these 34 SNPs.
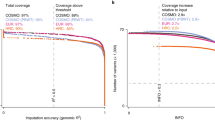
Estimating expected effect sizes of inflammatory protein variants on type 2 diabetes risk
We calculated the approximate effect size we would expect a SNP that alters inflammatory protein levels to have on the risk of type 2 diabetes, if the inflammatory protein is causal to type 2 diabetes. We used the triangulation approach outlined in Fig. 1 to (1) estimate the expected per allele effect of a SNP on type 2 diabetes risk (A in Fig. 1), given (2) the per allele effect of the SNP on inflammatory protein levels (B in Fig. 1), and (3) the correlation between inflammatory protein levels and type 2 diabetes (C in Fig. 1). We did not have measures of inflammatory-related proteins in our cases and controls and so we used data from previous studies to obtain approximate effect sizes. For example, each allele of rs2250417, in the IL18 gene, raises IL-18 levels by 0.28 SDs in the InCHIANTI study [17]. In the same study, a 0.28 SD (68 pg/ml) rise in IL-18 levels is associated with an OR of 1.15 (95% CI 1.09–1.21) for type 2 diabetes risk (L. Ferrucci, unpublished results). The prospective KORA study of type 2 diabetes showed that individuals in the top quartile of IL-18 levels, had IL-18 levels 242 pg/ml higher than those in the bottom quartile [46], and a risk ratio for type 2 diabetes of 1.96 (95% CI 1.49–2.58). Using these figures we calculated that an allele effect of 68 pg/ml will equate to an approximate expected effect of a risk ratio of 1.21 (95% CI 1.12–1.30) for type 2 diabetes. Similar calculations using the previously reported effect of rs8192284 in the IL6R gene on IL-6 levels [24] and risk estimates from prospective studies of IL-6 with type 2 diabetes [47], suggest we would expect an approximate per allele effect of rs8192284 of 1.06 (95% CI 1.04–1.08) for type 2 diabetes risk. Using the previously reported effect of rs12093699 in the CRP gene on CRP levels [17] and risk estimates from prospective studies of CRP with type 2 diabetes [5] we would expect an approximate per allele effect of rs12093699 of a risk ratio of 1.34 (95% CI 1.23–1.39) for type 2 diabetes risk (ESM Table 2). These estimates are very approximate because they use circulating measures from different studies. In the case of prospective studies, estimates are based on risk ratios rather than ORs but the incidence of type 2 diabetes (5–10%) means that risk ratios and ORs will be approximately equivalent.
Associations between the SNP rs2250417 and IL-18 levels, IL-18 levels and type 2 diabetes and the expected and observed effects of rs2250417 on type 2 diabetes. ORs and risk ratios for the IL-18 levels–type 2 diabetes association are those estimated for a 0.28 SD increase in IL-18 levels, the effect of rs2250417 on IL-18 levels, from the InCHIANTI [17] and KORA studies [46]. Odds ratios and risk ratios are shown with 95% CIs
Results
SNPs known to alter circulating levels of inflammatory proteins
We found no strong evidence that eight SNPs, robustly associated with circulating levels of inflammatory proteins, alter the risk of type 2 diabetes. Associations with type 2 diabetes risk for two SNPs, one in each of the IL18 and IL1RN genes, reached p < 0.1 in the three-study meta-analysis. The protein products of these two genes have both been strongly implicated in type 2 diabetes in trial and prospective studies and so we assigned a less-stringent statistical threshold for follow-up. At the time of study the SNP in each of these genes that represented the strongest association with circulating levels was uncertain. We therefore decided to increase the confidence of our genetic association findings (negative or positive) by increasing the sample size for all four SNPs in IL1RN and IL18. Meta-analysis using a total GWA and replication sample of 7,232 cases and 8,783 controls showed no strong evidence of association (Table 1). Subsequent analysis [17] indicated that rs2250417 had the strongest association with circulating IL-18 levels. The OR observed between the IL-18-altering variant, rs2250417, and type 2 diabetes is 1.00 (95% CI 0.99–1.03) (Fig. 1d). This is much lower than that expected given (1) the effect of the variant on IL-18 levels (0.28 SDs per allele [17]), and (2) estimates, based on other studies, of the correlation between IL-18 levels and type 2 diabetes risk, which are 1.15 (95% CI 1.09–1.21) per 0.28 SD increase in IL-18 levels in the InCHIANTI study (L. Ferrucci, unpublished results), and a risk ratio of 1.21 (95% CI 1.12–1.30) based on the KORA prospective study [46] (Fig. 1).
All ORs and p values from the meta-analysis are given in Table 1. The upper 95% CIs for risk alleles did not exceed 1.10. There was no evidence of association when limiting the analysis to the directly genotyped proxies, which captured six of the eight SNPs through directly genotyped proxies at r 2 > 0.8, in the WTCCC and DGI studies (ESM Table 3).
SNPs known to alter the risk of autoimmune diseases
We found no strong evidence that SNPs robustly associated with multiple autoimmune diseases alter the risk of type 2 diabetes. ORs and p values from the three-study meta-analysis are given in Table 2. The upper 95% CIs for risk alleles did not exceed 1.12. We found no strong evidence that SNPs robustly associated with individual autoimmune diseases, including type 1 diabetes, alter the risk of type 2 diabetes. ORs and p values from the three-study meta-analysis are given in Table 3. The upper 95% CIs for risk alleles did not exceed 1.19. There was also no evidence of association when limiting the analysis to directly genotyped proxies, which captured 28 of the 38 SNPs at r 2 > 0.8 in the WTCCC and DGI studies (ESM Table 3).
Discussion
We have found no evidence that common gene variants known to alter circulating levels of inflammatory proteins, or those robustly associated with autoimmune or inflammatory-based diseases, influence risk of type 2 diabetes. We have not corrected for multiple testing because, given that our results are consistent with no association, this would be anti-conservative, rather than conservative. We included variants that influence inflammatory protein levels that are altered many years before the onset of diabetes. Included in our study were variants known to alter IL-1RA levels. This inflammatory protein is of particular interest because administration of recombinant human IL-1RA (anakinra) in a recent parallel group trial improved beta cell function in type 2 diabetic patients. However, we found no evidence that lifetime exposure to slightly lower IL-1RA levels, as determined by IL1RN genotypes, predisposes to type 2 diabetes.
Our results are consistent with chronic inflammation being secondary to type 2 diabetes disease processes rather than being causal. This does not rule out a role for other inflammatory or autoimmune processes, for which there is no known genetic variant. There are a number of limitations to our study. The main limitation is that we have not measured inflammatory proteins in our cases and controls. This means that we cannot perform a formal Mendelian randomisation analysis, where it is preferable to have the SNP, inflammatory protein levels and disease status measured in the same study. However, using data from other studies we estimated that variants that alter IL-18, IL-6 and CRP levels should predispose to type 2 diabetes with ORs of approximately 1.15 to >1.21, 1.06 and 1.34, respectively (ESM Table 2), if these pro-inflammatory proteins are causally related to type 2 diabetes. The upper 95% CI of the effect sizes we observed (1.05, 1.02 and 1.09 for IL18, IL6R and CRP variants, respectively) are lower than the expected effect size. This is consistent with raised IL-18, IL-6 and CRP levels being secondary to, rather than causally predisposing to, type 2 diabetes. Further studies are needed with measures of inflammatory proteins in large numbers of cases and controls. It is also possible that these variants are not altering inflammatory pathways even if they are altering circulating levels.
A second limitation is that variants known to alter the risk of autoimmune and inflammatory diseases may not have an inflammatory effect in the general population. However, the identification of variants associated with inflammatory and autoimmune-related diseases indicates that the variant may be altering the expression, processing or function of a nearby gene that is critical to an inflammatory or autoimmune process prior to disease onset. Most of the autoimmune disease-associated variants have only been discovered very recently and so the disease mechanisms are not completely understood. However, early studies indicate that the variant in the IL2RA region predisposing to type 1 diabetes and multiple sclerosis alters circulating levels of IL2RA protein [48], the variant predisposing to coeliac disease in the IL18RAP locus alters mRNA levels of IL-18 receptor accessory protein in lymphocytes [31] and the variant in the IL7RA (also known as IL7R) gene predisposing to multiple sclerosis alters levels of soluble IL-7 receptor antagonist because of differential splicing of a key exon [49]. It is also suggested that the variant predisposing to ankylosing spondylitis in the ARTS1 (also known as ERAP-1) gene may have a general pro-inflammatory effect because it cleaves cell surface receptors for IL-1, IL-6 and TNF-α [32].
A final possible limitation is that we have used imputed SNP genotypes for association analysis for the majority of the 46 studied variants. However, this is unlikely to have resulted in appreciable differences in OR estimates, as has previously been shown [40, 50] and there were no positive associations when we used the strongest available directly genotyped proxies (r 2 > 0.8) instead of the imputed SNPs (ESM Table 3).
A further implication of our study is that it does not support the hypothesis of a genetic overlap between type 1 and type 2 diabetes. Our results are consistent with the recent studies which show that the known type 2 diabetes- and BMI-associated variants in the TCF7L2 [37] and FTO [38] genes do not predispose to type 1 diabetes.
In conclusion, in a large case–control study of type 2 diabetes, we tested 46 SNPs associated with inflammatory diseases or inflammatory protein levels, and identified no associations with type 2 diabetes. Our study is consistent with inflammatory processes being secondary, rather than causal, to type 2 diabetes.
Abbreviations
- CRP:
-
C-reactive protein
- DGI:
-
Diabetes Genetics Initiative
- FUSION:
-
Finland–United States Investigation of NIDDM
- GWA:
-
genome-wide association
- IL-1RA:
-
IL-1 receptor antagonist
- MAF:
-
minor allele frequency
- MIF:
-
macrophage migration inhibitory factor
- PAI:
-
plasminogen activator inhibitor
- sIL-6R:
-
soluble IL-6 receptor
- SLE:
-
systemic lupus erythematosus
- SNP:
-
single-nucleotide polymorphism
- WTCCC:
-
Wellcome Trust Case Control Consortium
References
Kolb H, Mandrup-Poulsen T (2005) An immune origin of type 2 diabetes. Diabetologia 48:1038–1050
Herder C, Kolb H, Koenig W et al (2006) Association of systemic concentrations of macrophage migration inhibitory factor with impaired glucose tolerance and type 2 diabetes: results from the Cooperative Health Research in the Region of Augsburg, Survey 4 (KORA S4). Diabetes Care 29:368–371
Duncan BB, Schmidt MI, Pankow JS et al (2003) Low-grade systemic inflammation and the development of type 2 diabetes: the atherosclerosis risk in communities study. Diabetes 52:1799–1805
Barzilay JI, Abraham L, Heckbert SR et al (2001) The relation of markers of inflammation to the development of glucose disorders in the elderly: the Cardiovascular Health Study. Diabetes 50:2384–2389
Spranger J, Kroke A, Mohlig M et al (2003) Inflammatory cytokines and the risk to develop type 2 diabetes: results of the prospective population-based European Prospective Investigation into Cancer and Nutrition (EPIC)–Potsdam Study. Diabetes 52:812–817
Netea MG, Joosten LA, Lewis E et al (2006) Deficiency of interleukin-18 in mice leads to hyperphagia, obesity and insulin resistance. Nat Med 12:650–656
Matsuki T, Horai R, Sudo K, Iwakura Y (2003) IL-1 plays an important role in lipid metabolism by regulating insulin levels under physiological conditions. J Exp Med 198:877–888
Chida D, Osaka T, Hashimoto O, Iwakura Y (2006) Combined interleukin-6 and interleukin-1 deficiency causes obesity in young mice. Diabetes 55:971–977
Dong ZM, Gutierrez-Ramos JC, Coxon A, Mayadas TN, Wagner DD (1997) A new class of obesity genes encodes leukocyte adhesion receptors. Proc Natl Acad Sci U S A 94:7526–7530
Nath SK, Han S, Kim-Howard X et al (2008) A nonsynonymous functional variant in integrin-alpha(M) (encoded by ITGAM) is associated with systemic lupus erythematosus. Nat Genet 40:152–154
Wolf N, Quaranta M, Prescott NJ et al (2008) Psoriasis is associated with pleiotropic susceptibility loci identified in type II diabetes and Crohn disease. J Med Genet 45:114–116
Donath MY, Storling J, Maedler K, Mandrup-Poulsen T (2003) Inflammatory mediators and islet beta-cell failure: a link between type 1 and type 2 diabetes. J Mol Med 81:455–470
Larsen CM, Faulenbach M, Vaag A et al (2007) Interleukin-1-receptor antagonist in type 2 diabetes mellitus. N Engl J Med 356:1517–1526
Timpson NJ, Lawlor DA, Harbord RM et al (2005) C-reactive protein and its role in metabolic syndrome: Mendelian Randomisation Study. Lancet 366:1954–1959
Tiret L, Godefroy T, Lubos E et al (2005) Genetic analysis of the interleukin-18 system highlights the role of the interleukin-18 gene in cardiovascular disease. Circulation 112:643–650
Frayling TM, Rafiq S, Murray A et al (2007) An interleukin-18 polymorphism is associated with reduced serum concentrations and better physical functioning in older people. J Gerontol A Biol Sci Med Sci 62:73–78
Melzer D, Perry JR, Hernandez D et al (2008) A genome-wide association study identifies protein quantitative trait loci (pQTLs). PLoS Genet 4:e1000072
Rafiq S, Stevens K, Hurst AJ et al (2007) Common genetic variation in the gene encoding interleukin-1-receptor antagonist (IL-1RA) is associated with altered circulating IL-1RA levels. Genes Immun 8:344–351
Kathiresan S, Gabriel SB, Yang Q et al (2005) Comprehensive survey of common genetic variation at the plasminogen activator inhibitor-1 locus and relations to circulating plasminogen activator inhibitor-1 levels. Circulation 112:1728–1735
Herder C, Klopp N, Baumert J et al (2008) Effect of macrophage migration inhibitory factor (MIF) gene variants and MIF serum concentrations on the risk of type 2 diabetes: results from the MONICA/KORA Augsburg Case-Cohort Study, 1984–2002. Diabetologia 51:276–284
Russell AI, Cunninghame Graham DS, Shepherd C et al (2004) Polymorphism at the C-reactive protein locus influences gene expression and predisposes to systemic lupus erythematosus. Hum Mol Genet 13:137–147
Zee RY, Ridker PM (2002) Polymorphism in the human C-reactive protein (CRP) gene, plasma concentrations of CRP, and the risk of future arterial thrombosis. Atherosclerosis 162:217–219
Reich D, Patterson N, Ramesh V et al (2007) Admixture mapping of an allele affecting interleukin 6 soluble receptor and interleukin 6 levels. Am J Hum Genet 80:716–726
Rafiq S, Frayling TM, Murray A et al (2007) A common variant of the interleukin 6 receptor (IL-6r) gene increases IL-6r and IL-6 levels, without other inflammatory effects. Genes Immun 8:552–559
Parkes M, Barrett JC, Prescott NJ et al (2007) Sequence variants in the autophagy gene IRGM and multiple other replicating loci contribute to Crohn’s disease susceptibility. Nat Genet 39:830–832
Rioux JD, Xavier RJ, Taylor KD et al (2007) Genome-wide association study identifies new susceptibility loci for Crohn disease and implicates autophagy in disease pathogenesis. Nat Genet 39:596–604
Todd JA, Walker NM, Cooper JD et al (2007) Robust associations of four new chromosome regions from genome-wide analyses of type 1 diabetes. Nat Genet 39:857–864
Thomson W, Barton A, Ke X et al (2007) Rheumatoid arthritis association at 6q23. Nat Genet 39:1431–1433
Plenge RM, Cotsapas C, Davies L et al (2007) Two independent alleles at 6q23 associated with risk of rheumatoid arthritis. Nat Genet 39:1477–1482
van Heel DA, Franke L, Hunt KA et al (2007) A genome-wide association study for celiac disease identifies risk variants in the region harboring IL-2 and IL-21. Nat Genet 39:827–829
Hunt KA, Zhernakova A, Turner G et al (2008) Newly identified genetic risk variants for celiac disease related to the immune response. Nat Genet 40:395–402
Burton PR, Clayton DG, Cardon LR et al (2007) Association scan of 14,500 nonsynonymous SNPs in four diseases identifies autoimmunity variants. Nat Genet 39:1329–1337
Harley JB, Alarcon-Riquelme ME, Criswell LA et al (2008) Genome-wide association scan in women with systemic lupus erythematosus identifies susceptibility variants in ITGAM, PXK, KIAA1542 and other loci. Nat Genet 40:204–210
Kozyrev SV, Abelson AK, Wojcik J et al (2008) Functional variants in the B cell gene BANK1 are associated with systemic lupus erythematosus. Nat Genet 40:211–216
Hafler DA, Compston A, Sawcer S et al (2007) Risk alleles for multiple sclerosis identified by a genomewide study. N Engl J Med 357:851–862
Wilkin TJ (2006) The accelerator hypothesis: a unifying explanation for type-1 and type-2 diabetes. Nestle Nutr Workshop Ser Clin Perform Programme 11:139–150; discussion 150–133
Field SF, Howson JM, Smyth DJ, Walker NM, Dunger DB, Todd JA (2007) Analysis of the type 2 diabetes gene, TCF7L2, in 13,795 type 1 diabetes cases and control subjects. Diabetologia 50:212–213
Field SF, Howson JM, Walker NM, Dunger DB, Todd JA (2007) Analysis of the obesity gene FTO in 14,803 type 1 diabetes cases and controls. Diabetologia 50:2218–2220
Cervin C, Lyssenko V, Bakhtadze E et al (2008) Genetic similarities between latent autoimmune diabetes in adults, type 1 diabetes, and type 2 diabetes. Diabetes 57:1433–1437
Zeggini E, Scott LJ, Saxena R et al (2008) Meta-analysis of genome-wide association data and large-scale replication identifies additional susceptibility loci for type 2 diabetes. Nat Genet 40:638–645
Kavvoura FK, Ioannidis JP (2008) Methods for meta-analysis in genetic association studies: a review of their potential and pitfalls. Hum Genet 123:1–14
Saxena R, Voight BF, Lyssenko V et al (2007) Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science 316:1331–1336
Scott LJ, Mohlke KL, Bonnycastle LL et al (2007) A genome-wide association study of type 2 diabetes in Finns detects multiple susceptibility variants. Science 316:1341–1345
Zeggini E, Weedon MN, Lindgren CM et al (2007) Replication of genome-wide association signals in UK samples reveals risk loci for type 2 diabetes. Science 316:1336–1341
Galicia JC, Tai H, Komatsu Y, Shimada Y, Akazawa K, Yoshie H (2004) Polymorphisms in the IL-6 receptor (IL-6R) gene: strong evidence that serum levels of soluble IL-6R are genetically influenced. Genes Immun 5:513–516
Thorand B, Kolb H, Baumert J et al (2005) Elevated levels of interleukin-18 predict the development of type 2 diabetes: results from the MONICA/KORA Augsburg Study, 1984–2002. Diabetes 54:2932–2938
Hu FB, Meigs JB, Li TY, Rifai N, Manson JE (2004) Inflammatory markers and risk of developing type 2 diabetes in women. Diabetes 53:693–700
Lowe CE, Cooper JD, Brusko T et al (2007) Large-scale genetic fine mapping and genotype-phenotype associations implicate polymorphism in the IL2RA region in type 1 diabetes. Nat Genet 39:1074–1082
Gregory SG, Schmidt S, Seth P et al (2007) Interleukin 7 receptor alpha chain (IL7R) shows allelic and functional association with multiple sclerosis. Nat Genet 39:1083–1091
Marchini J, Howie B, Myers S, McVean G, Donnelly P (2007) A new multipoint method for genome-wide association studies by imputation of genotypes. Nat Genet 39:906–913
Acknowledgements
M. N. Weedon is a Vandervell Foundation research fellow. The FUSION study was funded by an intramural grant (NIH DK 062370) from the US National Institutes of Health (NIH). E. Zeggini is a Wellcome Trust Career Development Fellow. D. Melzer’s work is supported in part by NIH/National Institute on Aging (NIH/NIA) Grant R01 AG24233. Details of the DIAGRAM (Diabetes Genetics Replication And Meta-analysis) Consortium can be found at http://www.well.ox.ac.uk/DIAGRAM/index.html.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
Characteristics of initial scan and replication study participants (18 kb)
ESM Table 2
Description of SNP effects on circulating protein levels in the InCHIANTI study [21] and measures used from previous type 2 diabetes prospective studies to derive estimates of expected effects of SNP on type 2 diabetes risk (24 kb)
ESM Table 3
Results for inflammatory and autoimmune disease SNPs using the best available directly genotyped proxies (45 kb)
Rights and permissions
About this article
Cite this article
Rafiq, S., Melzer, D., Weedon, M.N. et al. Gene variants influencing measures of inflammation or predisposing to autoimmune and inflammatory diseases are not associated with the risk of type 2 diabetes. Diabetologia 51, 2205–2213 (2008). https://doi.org/10.1007/s00125-008-1160-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-008-1160-3