Abstract
Background and objective
Angiotensin II type 1 receptor antagonists (ARBs) are widely used as a substitute for angiotensin-converting enzyme inhibitors (ACEIs) to treat patients without heart failure, but their effect on cardiovascular morbidity and mortality has not been clearly determined. A systematic review and metaanalysis was undertaken to determine the impact of ARBs on cardiovascular outcomes in high-risk patients without heart failure.
Methods
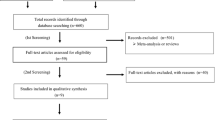
A computerized literature search was carried out using PubMed, the Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library, MEDLINE, and EMBASE, from January 1990 to April 2008. The following search terms were used: ‘hypertension’, ‘clinical trial’, ‘sartan’, ‘ARB’, ‘angiotensin receptor antagonist’, ‘losartan’, ‘candesartan’, ‘valsartan’, ‘irbesartan’, ‘eprosartan’, ‘telmisartan’, ‘olmesartan’, ‘coronary disease’, ‘coronary heart disease’, ‘myocardial infarction’, ‘cardiovascular disease’, ‘cerebrovascular disease’, and ‘stroke’. Criteria for inclusion of clinical trials in our meta-analysis were the use of a randomized control group not receiving an ARB and the availability of outcome data for any one of four endpoints: myocardial infarction (MI), stroke, cardiovascular death, and all-cause death (these were not always pre-specified endpoints in all trials). Out of 45 potentially relevant studies, 37 trials met the inclusion criteria. We tabulated all occurrences of these four adverse outcomes.
Results
Homogenous subgroups were combined by means of a fixed-effects model, while heterogenous subgroups were not combined. In the subgroup without heart failure, ARBs, when compared with the control group, had an odds ratio of 1.09 (95% CI 1.00, 1.18; p = 0.05) for MI. Other endpoints, namely, cardiovascular death and all-cause death, did not reach statistical significance. There was a clear trend for fewer strokes in the ARB group, but these studies were clearly heterogenous, and therefore a pooled risk estimate was not computed.
Conclusion
After pooling more than 89 000 patients, there is no evidence to suggest that ARBs confer cardiovascular protection akin to ACEIs, and the results that emerged are not in favor of ARB therapy in terms of its use as a substitute for ACEIs in non-heart failure patients. ARBs may have a small benefit in terms of stroke risk, but the studies are heterogenous, making it very difficult to quantify this effect. Given that ACEIs protect against both stroke and MI, caution is advised in the use of ARBs as a substitute for ACEIs in patients without a heart failure indication, who are tolerant of an ACEI.











Similar content being viewed by others
References
Pitt B, Segal R, Martinez FA, et al. Randomised trial of losartan versus captopril in patients over 65 with heart failure (Evaluation of Losartan in the Elderly Study, ELITE). Lancet 1997; 349: 747–52
Pitt B, Poole-Wilson PA, Segal R, et al. Effect of losartan compared with captopril on mortality in patients with symptomatic heart failure: randomized trial. The Losartan Heart Failure Survival Study ELITE II. Lancet 2000; 355: 1582–7
Cohn JN, Tognoni G. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med 2001; 345: 1667–75
Pfeffer MA, Swedberg K, Granger CB, et al. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programme. Lancet 2003; 362: 759–66
Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 2001; 345: 861–9
Levy BI. Can angiotensin II type 2 receptors have deleterious effects in cardiovascular disease? Implications for therapeutic blockade of the random-angiotensin system. Circulation 2004; 109: 8–13
Swedberg K, McMurray JJ. Angiotensin receptor blockers and heart failure: still CHARMing after VALIANT? Eur Heart J 2004; 25: 357–8
McMurray JJ. Angiotensin receptor blockers for chronic heart failure and acute myocardial infarction. Heart 2001; 86: 97–103
Stafford RS, Monti V, Furberg CD, et al. Long-term and short-term changes in antihypertensive prescribing by office-based physicians in the United States. Hypertension 2006; 48: 213–8
Strauss MH, Hall AS. Angiotensin receptor blockers may increase risk of myocardial infarction: unraveling the ARB-MI paradox. Circulation 2006; 114: 838–54
Verma S, Strauss M. Angiotensin receptor blockers and myocardial infarction. BMJ 2004; 329: 1248–9
ARB and myocardial infarction. Med Lett 2005; 47: 38–9
Yusuf S, Teo KK, Pogue J, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med 2008; 358: 1547–59
Dahlof B, Devereux RB, Kjeldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomized trial against atenolol. Lancet 2002; 359: 995–1003
McMurray JJ, Ostergren J, Swedberg K, et al. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function taking angiotensin-converting-enzyme inhibitors: the CHARM-Added trial. Lancet 2003; 362: 767–71
Yusuf S, Pfeffer MA, Swedberg K, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet 2003; 362: 777–81
Granger CB, McMurray JJ, Yusuf S, et al. Effects of candesartan in patients with chronic heart failure and reduced left-ventricular systolic function intolerant to angiotensin-converting-enzyme inhibitors: the CHARM-Alternative trial. Lancet 2003; 362: 772–6
Lithell H, Hansson L, Skoog I, et al. The Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trial. J Hypertens 2003; 21: 875–86
Lindholm LH, Persson M, Alaupovic P, et al. Metabolic outcome during 1 year in newly detected hypertensives: results of the Antihypertensive Treatment and Lipid Profile in a North of Sweden Efficacy Evaluation (ALPINE study). J Hypertens 2003; 21: 1563–74
Barnett AH. Preventing renal complications in diabetic patients: the Diabetics Exposed to Telmisartan And enalaprIL (DETAIL) study. Acta Diabetol 2005; 42 Suppl. 1: S42–9
Julius S, Kjeldsen SE, Weber M, et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomized trial. Lancet 2004; 363: 2022–31
Mochizuki S, Dahlof B, Shimizu M, et al. Valsartan in a Japanese population with hypertension and other cardiovascular disease (Jikei Heart Study): a randomized, open-label, blinded endpoint morbidity-mortality study. Lancet 2007; 369: 1431–9
Dickstein K, Kjekshus J. Effects of losartan and captopril on mortality and morbidity in high-risk patients after acute myocardial infarction: the OPTIMAAL randomized trial. Optimal Trial in Myocardial Infarction with Angiotensin II Antagonist Losartan. Lancet 2002; 360: 752–60
McMurray J, Solomon S, Pieper K, et al. The effect of valsartan, captopril, or both on atherosclerotic events after acute myocardial infarction: an analysis of the Valsartan in Acute Myocardial Infarction Trial (VALIANT). J Am Coll Cardiol 2006; 47: 726–33
Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 2001; 345: 851–60
Bakris G, Sica D, Ram V, et al. A comparative trial of controlled-onset, extended-release verapamil, enalapril, and losartan on blood pressure and heart rate changes. Am J Hypertens 2002; 15: 53–7
Haneda M, Kikkawa R, Sakai H, et al. Antiproteinuric effect of candesartan cilexetil in Japanese subjects with type 2 diabetes and nephropathy. Diabetes Res Clin Pract 2004; 66: 87–95
Granger CB, Ertl G, Kuch J, et al. Randomized trial of candesartan cilexetil in the treatment of patients with congestive heart failure and a history of intolerance to angiotensin-converting enzyme inhibitors. Am Heart J 2000; 139: 609–17
Crozier I, Ikram H, Awan N, et al. Losartan in heart failure: hemodynamic effects and tolerability. Losartan Hemodynamic Study Group. Circulation 1995; 91: 691–7
Riegger GA, Bouzo H, Petr P, et al. Improvement in exercise tolerance and symptoms of congestive heart failure during treatment with candesartan cilexetil. Symptom, Tolerability, Response to Exercise Trial of Candesartan Cilexetil in Heart Failure (STRETCH) Investigators. Circulation 1999; 100: 2224–30
Mitrovic V, Willenbrock R, Miric M, et al. Acute and 3-month treatment effects of candesartan cilexetil on hemodynamics, neurohormones, and clinical symptoms in patients with congestive heart failure. Am Heart J 2003; 145: E14
Matsumori A. Efficacy and safety of oral candesartan cilexetil in patients with congestive heart failure. Eur J Heart Fail 2003; 5: 669–77
Di Pasquale P, Bucca V, Scalzo S, et al. Does the addition of losartan improve the beneficial effects of ACE inhibitors in patients with anterior myocardial infarction? A pilot study. Heart 1999; 81: 606–11
Mazayev VP, Fomina IG, Kazakov EN, et al. Valsartan in heart failure patients previously untreated with an ACE inhibitor. Int J Cardiol 1998; 65: 239–46
Dunselman PH. Effects of the replacement of the angiotensin converting enzyme inhibitor enalapril by the angiotensin II receptor blocker telmisartan in patients with congestive heart failure. The replacement of angiotensin converting enzyme inhibition (REPLACE) investigators. Int J Cardiol 2001; 77: 131–8; discussion 139–40
Willenheimer R, Helmers C, Pantev E, et al. Safety and efficacy of valsartan versus enalapril in heart failure patients. Int J Cardiol 2002; 85: 261–70
Spinar J, Vitovec J, Spinarova L, et al. A comparison of intervention with losartan or captopril in acute myocardial infarction. Eur J Heart Fail 2000; 2:91–100
Dickstein K, Chang P, Willenheimer R, et al. Comparison of the effects of losartan and enalapril on clinical status and exercise performance in patients with moderate or severe chronic heart failure. J Am Coll Cardiol 1995; 26: 438–45
Lang RM, Elkayam U, Yellen LG, et al. Comparative effects of losartan and enalapril on exercise capacity and clinical status in patients with heart failure. The Losartan Pilot Exercise Study Investigators. J Am Coll Cardiol 1997; 30: 983–91
Weber M. Clinical safety and tolerability of losartan. Clin Ther 1997; 19: 604–16; discussion 603
Hamroff G, Katz SD, Mancini D, et al. Addition of angiotensin II receptor blockade to maximal angiotensin-converting enzyme inhibition improves exercise capacity in patients with severe congestive heart failure. Circulation 1999; 99: 990–2
McKelvie RS, Yusuf S, Pericak D, et al. Comparison of candesartan, enalapril, and their combination in congestive heart failure: randomized evaluation of strategies for left ventricular dysfunction (RESOLVD) pilot study. The RESOLVD Pilot Study Investigators. Circulation 1999; 100: 1056–64
Baruch L, Anand I, Cohen I, et al. Augmented short- and long-term hemodynamic and hormonal effects of angiotensin receptor blocker added to angiotensin converting enzyme inhibitor therapy in patients with heart failure. Circulation 1999; 99: 2658–64
Sharma D, Buyse M, Pitt B, et al. Meta-analysis of observed mortality data from all-controlled, double-blind, multiple-dose studies of losartan in heart failure. Losartan Heart Failure Mortality Meta-analysis Study Group. Am J Cardiol 2000; 85: 187–92
Jong P, Demers C, McKelvie RS, et al. Angiotensin receptor blockers in heart failure: meta-analysis of randomized controlled trials. J Am Coll Cardiol 2002; 39: 463–70
McDonald MA, Simpson SH, Ezekowitz JA, et al. Angiotensin receptor blockers and risk of myocardial infarction: systematic review. BMJ 2005; 331: 873
Lee VC, Rhew DC, Dylan M, et al. Meta-analysis: angiotensin-receptor blockers in chronic heart failure and high-risk acute myocardial infarction. Ann Intern Med 2004; 141: 693–704
Bax L, Yu LM, Ikeda N, et al. Development and validation of MIX: comprehensive free software for meta-analysis of causal research data. BMC Med Res Methodol 2006; 6: 50
Cucherat M, Boissel JP, Leizorovicz A, et al. EasyMA: a program for the meta-analysis of clinical trials. Comput Methods Programs Biomed 1997; 53: 187–90
Peto R. Why do we need systematic overviews of randomized trials? Stat Med 1987; 6: 233–44
Thompson SG, Pocock SJ. Can meta-analyses be trusted? Lancet 1991; 338: 1127–30
Poole C, Greenland S. Random-effects meta-analyses are not always conservative. Am J Epidemiol 1999; 150: 469–75
Epstein BJ, Gums JG. Angiotensin receptor blockers versus ACE inhibitors: prevention of death and myocardial infarction in high-risk populations. Ann Pharmacother 2005; 39: 470–80
Yusuf S. From the HOPE to the ONTARGET and the TRANSCEND studies: challenges in improving prognosis. Am J Cardiol 2002; 89: 18A–25A; discussion 25–6A
Levy BI. How to explain the differences between random angiotensin system modulators. Am J Hypertens 2005; 18: 134S–141S
Wong J, Patel RA, Kowey PR. The clinical use of angiotensin-converting enzyme inhibitors. Prog Cardiovasc Dis 2004; 47: 116–30
Bennett MR, Macdonald K, Chan SW, et al. Cooperative interactions between RB and p53 regulate cell proliferation, cell senescence, and apoptosis in human vascular smooth muscle cells from atherosclerotic plaques. Circ Res 1998; 82: 704–12
Diep QN, Li JS, Schiffrin EL. In vivo study of AT(1) and AT(2) angiotensin receptors in apoptosis in rat blood vessels. Hypertension 1999; 34: 617–24
Thone-Reineke C, Zimmermann M, Neumann C, et al. Are angiotensin receptor blockers neuroprotective? Curr Hypertens Rep 2004; 6: 257–66
Li J, Culman J, Hortnagl H et al. Angiotensin AT2 receptor protects against cerebral ischemia-induced neuronal injury. FASEB J 2005; 19: 617–9
Iwai M, Liu HW, Chen R et al. Possible inhibition of focal cerebral ischemia by angiotensin II type 2 receptor stimulation. Circulation 2004; 110:843–8
Krikov M, Thone-Reineke C, Muller S, et al. Candesartan but not ramipril pretreatment improves outcome after stroke and stimulates neurotrophin BNDF/TrkB system in rats. J Hypertens 2008; 26: 544–52
Zhang H, Thijs L, Staessen JA. Blood pressure lowering for primary and secondary prevention of stroke. Hypertension 2006; 48: 187–95
Yusuf S, Sleight P, Pogue J, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 2000; 342: 145–53
Verdecchia P, Reboldi G, Angeli F, et al. Angiotensin-converting enzyme inhibitors and calcium channel blockers for coronary heart disease and stroke prevention. Hypertension 2005; 46: 386–92
2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens 2003; 21: 1011–53
Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction). Circulation 2004; 110:e82–292
Cheung BM, Cheung GT, Lauder IJ, et al. Meta-analysis of large outcome trials of angiotensin receptor blockers in hypertension. J Hum Hypertens 2006; 20: 37–43
Pfeffer MA, McMurray JJ, Velazquez EJ, et al. Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med 2003; 349: 1893–906
Scheen AJ. VALUE: analysis of results [letter]. Lancet 2004;364:932–3; author reply 935
Scheen AJ. Renin-angiotensin system inhibition prevents type 2 diabetes mellitus: part 1. A meta-analysis of randomized clinical trials. Diabetes Metab 2004; 30: 487–96
Diener HC, Sacco RL, Yusuf S, et al. Effects of aspirin plus extended-release dipyridamole versus clopidogrel and telmisartan on disability and cognitive function after recurrent stroke in patients with ischaemic stroke in the Prevention Regimen for Effectively Avoiding Second Strokes (PRoFESS) trial: a double-blind, active and placebo-controlled study. Lancet Neurol 2008; 7: 875–84
Yusuf S, Diener HC, Sacco RL, et al. Telmisartan to prevent recurrent stroke and cardiovascular events. N Engl J Med 2008; 359: 1225–37
Yusuf S, Teo K, Anderson C, et al. Effects of the angiotensin-receptor blocker telmisartan on cardiovascular events in high-risk patients intolerant to angiotensin-converting enzyme inhibitors: a randomised controlled trial. Lancet 2008; 372: 1174–83
Lin Z. An issue of statistical analysis in controlled multi-centre studies: how shall we weight the centres? Stat Med 1999; 18: 365–73
Senn S. Some controversies in planning and analysing multi-centre trials. Stat Med 1998; 17: 1753–65; discussion 1799–800
Acknowledgments
No sources of funding were used to assist in the preparation of this meta-analysis. The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Al Khalaf, M.M., Thalib, L. & Doi, S.A.R. Cardiovascular Outcomes in High-Risk Patients without Heart Failure Treated with ARBs. Am J Cardiovasc Drugs 9, 29–43 (2009). https://doi.org/10.1007/BF03256593
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03256593